Abstract
Opioid use in pregnancy has increased in parallel to the opioid crisis observed in the general population. Rising rates of peripartum opioid use pose a significant public health concern for both mothers and their children. Pregnancy also represents a unique opportunity for healthcare providers to screen women for opioid use disorder and engage them in appropriate care. In the present review, we describe patterns of opioid use in pregnancy and how this relates to maternal and neonatal health outcomes. We also examine screening for and treatment of opioid use disorder in pregnancy, neonatal outcomes following maternal opioid use, and breastfeeding recommendations for women taking opioids postpartum.
Keywords: Addiction, breastfeeding, clinical pharmacology, drug safety, opioids
Introduction
The past two decades have witnessed dramatic increases in opioid prescribing in North America. In concert, there have been increases in opioid-related adverse health outcomes particularly among young and middle-aged adults.1,2 The associated years of life lost is striking: in 2016 there were more than 1.6 million years lost (5.2 per 1000 population) in the United States.1 Consequently, the opioid epidemic has become one of the foremost public health crises in recent years.2
At present, Canada and the United States have the highest per capita opioid consumption worldwide.1 In 2017, there were almost 60 opioid prescriptions written for every 100 people in the United States.3 Today in North America, one in six people receives an opioid prescription annually.3 Most prescriptions are issued for acute pain, end-of-life care, and post-surgical pain. However, there have also been significant increases in prescriptions to patients with chronic noncancer pain. In these patients, opioids are often prescribed in larger quantities and for longer durations than initially intended, leading to net harm.4,5
Opioid use in pregnancy has increased in tandem with the epidemic observed in the general population. In 2012, approximately one in three reproductive-aged women filled an opioid prescription.6 Maternal opioid use during pregnancy increased five-fold from 2000 to 2009, and recent data suggest that one in five women in the United States will fill an opioid prescription during pregnancy.7 Unsurprisingly, there has been a contemporaneous 15-fold increase in the prevalence of neonatal abstinence syndrome (NAS).8,9
Increasing rates of opioid use in pregnancy pose a significant public health concern for both mothers and their children. Here, we describe opioid use in pregnancy and how it relates to maternal and neonatal health outcomes. We specifically examine screening for and treatment of opioid use disorder in pregnancy, neonatal outcomes following maternal opioid use in pregnancy, and breastfeeding recommendations for women taking opioids postpartum.
Pharmacology of opioids
Opioids are a group of endogenous and exogenous substances that bind to and activate central and peripheral mu (MOR), kappa (KOR), and delta (DOR) opioid receptors. They provide analgesia via their ability to inhibit nociceptive input at opioid receptors in the nervous system. They are also used for the treatment of cough and diarrhea, exerting their effects through peripheral MOR activation in the smooth muscle of the bronchi and intestines respectively. Their psychoactive properties—primarily euphoria and a feeling of tranquility—often underlie nonmedical use.
Opioids can be classified based on their chemical structure, duration of action, route of administration, and potency. Some opioids are naturally occurring opium alkaloids (e.g. codeine and morphine), while others are semi-synthetic forms of naturally occurring opioids (e.g. heroin and oxycodone) or fully synthetic (e.g. methadone and fentanyl).
Opioids can be further subdivided based on their activity at the MOR into pure agonists or partial agonists. Most opioids used for analgesia are full agonists, while partial agonists such as buprenorphine have lower intrinsic activity at the MOR. Opioids can be administered orally, sublingually, intranasally, subcutaneously, intravenously, rectally, transdermally, and via inhalation. The oral drugs are available in immediate-release or extended-release preparations, with the onset and intensity of effect varying depending on the route of administration, dose, and formulation.
Short-term adverse effects from opioids include respiratory depression, sedation, and drug dependence. Long-term adverse effects are less well recognized, but include depression, systemic infection (from intravenous use), sexual dysfunction, falls, traffic accidents, and sleep-disordered breathing.10 Chronic opioid use can lead to receptor sensitization and paradoxical worsening of pain, a phenomenon termed “opioid-induced hyperalgesia”.10 Emerging data suggest that chronic opioid use can also impact function of the hypothalamic–pituitary–adrenal axis, which may be particularly relevant for women who are pregnant or trying to conceive.10
Opioid use disorder in pregnancy
Women may take opioids during pregnancy for management of acute or chronic pain or as replacement therapy for an opioid use disorder (OUD). Less than 1% of pregnant women report opioid misuse.11 However, this number has risen 130% over the last two decades and today, more than 50% of admissions to substance use programs during pregnancy are opioid-related.11 A summary of the management of OUD in pregnancy and postpartum is shown in Table 1.
Table 1.
Summary of the management of opioid use disorder in pregnancy and postpartum.
| Prenatal screening |
| • All persons who are pregnant or who may become pregnant should be offered screening for substance use, including opioid use disorder (OUD). |
| • Screening should be accompanied by counseling on risks of substance use in pregnancy and available harm reduction strategies. |
| • Routine urine toxicology screening is not recommended in pregnancy, and should only be performed for specific clinical indications. |
| Treatment |
| • Abrupt opioid withdrawal is not recommended. Withdrawal can lead to adverse pregnancy outcomes such as preterm labor, and is associated with high rates of relapse. |
| • All individuals with OUD who are pregnant, or may become pregnant, should be offered opioid agonist treatment (OAT). Individuals treated with OAT are more likely to engage in appropriate prenatal care, and are less likely to suffer from serious obstetric complications such as growth restriction and preterm labor. |
| • Choice of OAT should be individualized and should take into consideration factors such as a woman’s preference, current treatment, and availability of local comprehensive programs for OUD. |
| • Methadone and buprenorphine/naloxone (suboxone) are both acceptable first line treatments for OUD in pregnancy. Both drugs have comparable safety and efficacy in pregnancy. |
| • If stable on a treatment regimen, transitioning between methadone and suboxone in pregnancy is not recommended unless clinically indicated. |
| • It is not necessary to switch to buprenorphine monotherapy in pregnancy in women who are stable on suboxone. |
| Pain management during labor and postpartum care |
| • OAT should be continued during labor and postpartum. Increasing the dose of OAT is not recommended, but converting a once daily dose to split doses may help to maintain consistent drug concentrations for analgesia. |
| • Consider multimodal pain strategies (including regional anesthesia) and involvement of specialists in pain management for treatment of labor and postpartum pain. |
| • If opioids are required for analgesia, preference should be given to drugs that were not previously misused. |
| • Rooming-in is recommended as part of the treatment for infants suffering from neonatal abstinence syndrome because it helps facilitate care for the mother–baby dyad. |
| Breastfeeding |
| • Women treated with OAT should be encouraged to breastfeed. |
| • All opioids pass into breastmilk resulting in small quantities ingested by breastfeeding infants. Under typical circumstances, infants are exposed to low amounts of opioids through breastfeeding, and instances of neonatal opioid toxicity from breastfeeding are exceeding rare. |
Information adapted from the British Columbia Centre on Substance Use: a guideline for the clinical management of opioid use disorder – pregnancy supplement.71
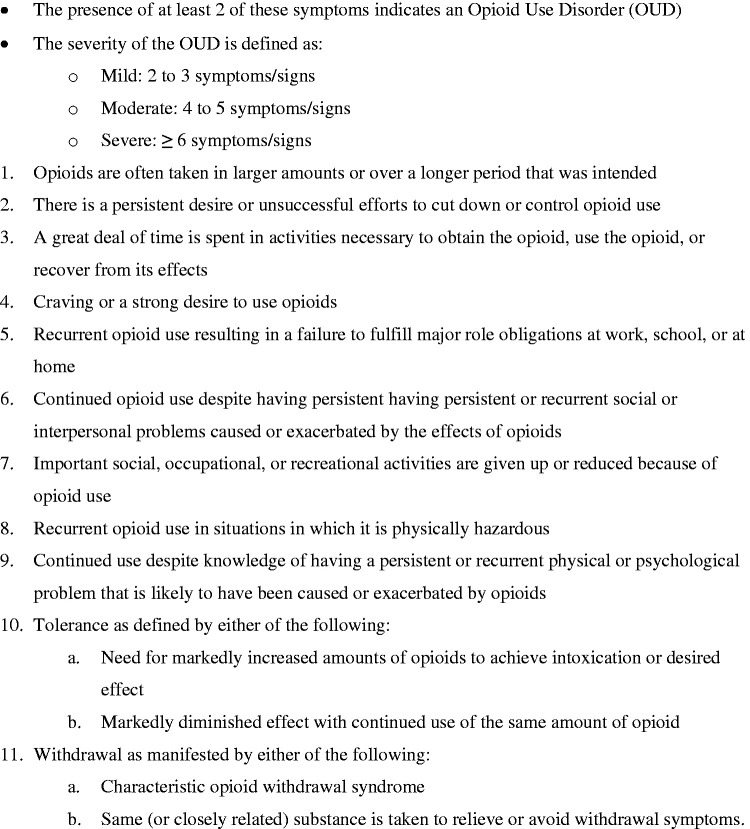
Opioid use disorder has defined diagnostic criteria (Figure 1) characterized by a pattern of tolerance, dependence, and inability to control use despite negative consequences. Tolerance is typified by use of escalating doses of drug to achieve the same therapeutic effect. Opioid dependence is an adaptive physical state following repeated drug exposure, resulting in withdrawal symptoms (agitation, yawning, sweating, tearing, mydriasis, piloerection, diarrhea, pain, mood disorders, and insomnia) upon cessation of use. A distinction is often drawn between dependence and addiction, with dependence as a largely physical phenomenon whereas addiction (or substance use disorder) is characterized by ongoing drug use despite adverse consequences.
Figure 1.
DSM-5 criteria for opioid use disorder.
Screening for OUD
Pregnancy offers a unique opportunity to screen and identify women with OUD, yet pregnant women may have several reasons not to disclose opioid use, including stigma, child custody issues, and potential legal consequences. These issues may also discourage women with OUD from seeking appropriate care.
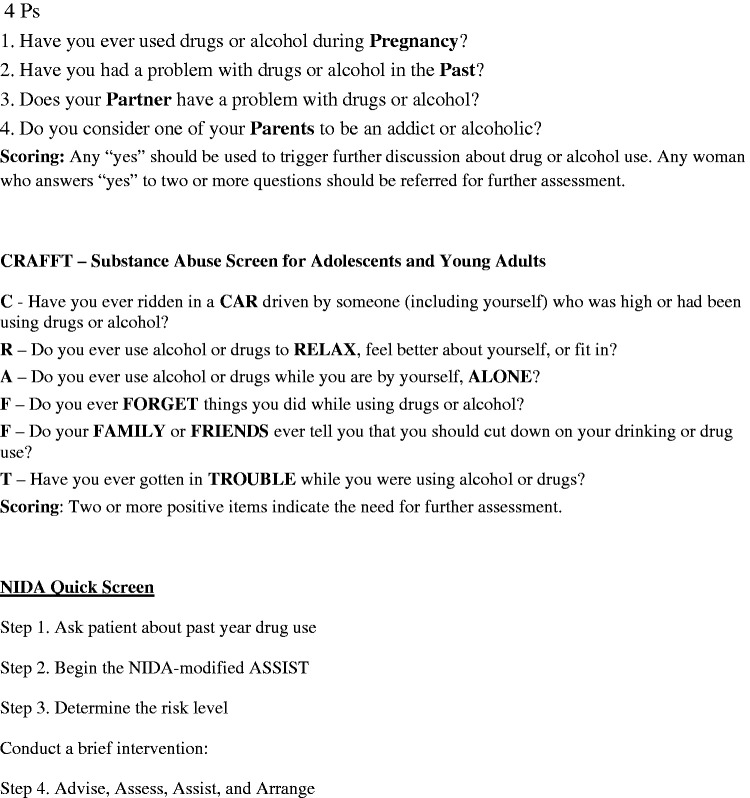
Professional societies including the American College of Obstetrics and Gynecology and the Society for Obstetrics and Gynecology of Canada endorse universal screening for substance use in pregnancy.12,13 Validated screening tools including the 4Ps, CRAFFT, and NIDA Quick screen (Figure 2) demonstrate good sensitivity for ruling out substance use in pregnancy.13–15 Routine toxicology testing (e.g. urine drug screens) is not recommended and should only be performed for a clinical indication with the woman aware of the potential ramifications of a positive result. Urine drug screens are also prone to false positive and false negative results, and may not rule out ongoing use.
Figure 2.
Clinical screening tools for substance use disorder in pregnancy.13
Treatment
Women with OUD require timely access to comprehensive addiction care, from pre-pregnancy through to the postpartum period. If left untreated, addiction in pregnancy is associated with high-risk sexual activity, violence, legal troubles and incarceration.13 Women with OUD disorder often suffer from comorbid mental illness and are more likely to use other substances.13 They are also less likely to engage in appropriate prenatal care, and their babies are more likely to suffer from obstetric complications including fetal growth restriction, placental abruption, preterm labor, and death.13,16
Treatment of OUD in pregnancy should mirror that in the general population, and is preferable to abrupt opioid cessation.13 Opioid agonist therapy (OAT) typically refers to opioid replacement with methadone or buprenorphine and has been shown to reduce maternal relapse and improve adherence to obstetric care.13
Pregnant women can take either methadone or buprenorphine for treatment of OUD. Both drugs have comparable efficacy and safety in pregnancy, although use of buprenorphine has been associated with a lower risk of preterm birth, greater birth weight, and larger neonatal head circumference.17,18 Studies have also shown that neonates whose mothers took buprenorphine have milder courses of NAS (shorter length of stay in hospital, shorter duration of treatment, and require lower doses of morphine) compared to neonates of mothers who took methadone.19 However, the Cochrane review on maintenance agonist treatment for opioid-dependent pregnant women found that treatment retention was better in women treated with methadone compared to those treated with buprenorphine.18 While both drugs are acceptable options for OAT in pregnancy, larger randomized controlled trials with appropriate drug dosing and longer follow-up periods are needed to further evaluate methadone and buprenorphine for treatment of pregnant women with OUD.18
The choice of OAT (methadone versus buprenorphine) in pregnancy requires a shared decision making approach. Factors to consider include a woman’s preference (including what may have worked well in the past), current treatment, and availability of local comprehensive programs for management of OUD. Methadone and buprenorphine are compared in Table 2. It bears mentioning that buprenorphine can be used in pregnancy on its own but is often combined with naloxone (a MOR antagonist) to discourage intravenous use. Naloxone is not pharmacologically active when taken sublingually, but can induce opioid withdrawal if injected. Initial concerns about the reproductive safety of naloxone (mainly due to lack of data) had originally led to recommendations that buprenorphine be used without naloxone in pregnancy. However, subsequent studies assessing the combined product have demonstrated similar neonatal outcomes with no evidence of added harm.20,21
Table 2.
Comparison of methadone versus buprenorphine use in pregnancy.
| Methadone | Buprenorphine | |
|---|---|---|
| Type of opioid | Synthetic long-acting agonist | Semi-synthetic long-acting partial agonist |
| Route of administration | Oral (liquid), tablet | Sublingual, transdermal |
| Typical dose range | 20–120 mg | 4–24 mg |
| Dose increase interval | 3 days | 1 day |
| Costa approximate (USD/week) including medical care | $126 | $115 |
| Dispensed | Daily by pharmacy (with options for small numbers of carries with proof of adherence and depending on urine drug testing results). | Maximum 100-day prescription in Canada (and other jurisdictions). Can be taken by patients unsupervised. |
| Dose modification in pregnancy | May be necessary to increase the dose towards end of pregnancy due to CYP3A4 and CYP2B6 induction and increased metabolism (particularly in 3rd trimester). | Generally not required, although some studies have suggested the need for small dose increases towards the end of pregnancy. |
| Breastfeeding | Safe | Safe |
| Advantages | • Difficult to divert:• supervised consumption• liquid dissolved in orange juice• No requirement for patients to demonstrate signs and symptoms of opioid withdrawal prior to starting treatment. Careful supervised dose titration is required once initiated. | • Fewer drug–drug interactions• No QTc prolongation• Higher ceiling for respiratory depression• Can be prescribed in the office setting and patients can take buprenorphine unsupervised. |
| Disadvantages | • In most jurisdictions prescribers need authorization to prescribe. • Higher risk of adverse events: overdose, respiratory depression. • Dose-dependent QTc prolongation. • Important drug–drug interactions, including but not limited to antiretroviral drugs, anticonvulsants, rifampin. • Care must be taken when combining with other drugs that can cause CNS depression or lower the respiratory rate (e.g. benzodiazepines). | • Risk of abuse and diversion, particularly with the buprenorphine monoproduct. • Initiation typically requires the patient to be in mild opioid withdrawal.b This can be problematic in pregnancy as opioid withdrawal can lead to premature labor and other adverse pregnancy outcomes. • In patients taking full opioid agonists, starting buprenorphine in the absence of withdrawal symptoms can precipitate opioid withdrawal. |
aFrom: How much does opioid treatment cost. NIH National Institute on Drug Abuse. www.drugabuse.gov/publications/research-reports/medications-to-treat-opioid-addiction/how-much-does-opioid-treatment-cost.
bNewer buprenorphine microdosing protocols may avoid the need to have patients go into withdrawal.
QTc, electrocardiogram corrected QT interval
Pain management during labor and postpartum
Treating labor and postpartum pain in women taking OAT can be complex and challenging. As a general principle, multimodal strategies (including regional anesthesia) and higher doses of opioids may be required to achieve adequate pain control. To guide treatment, it may be useful to involve experts in peripartum pain management, addictions, or an acute pain service. While the management of intrapartum and postpartum pain is beyond the scope of this review, there are a few key principles to consider.
OAT should be continued during delivery and postpartum. While increasing the dose of methadone or buprenorphine is generally not recommended to treat acute pain, some providers will convert a once daily dose into split doses (three times daily) to maintain more consistent drug concentrations for analgesia. There is also a tendency to under-medicate acute pain in women treated for OUD.22 Women who take opioids and those on OAT will naturally require higher doses for effective analgesia compared to those who are opioid-naïve. It is important to appreciate that additional opioid agonists (including those in epidural analgesia solutions) can be safely administered in these women (even in the presence of buprenorphine or methadone) without an increased risk of relapse.22 If additional opioids are required, preference should be given to opioids that were not previously misused. Opioids with partial agonist or agonist-antagonist properties—nalbuphine, pentazocine, butorphanol, meptazinol—should be avoided.
Maternal opioid use and pregnancy outcomes
Opioids can cross the placenta and the infant blood–brain barrier, posing a potential risk to the fetus in utero.23 Prenatal opioid exposure has been linked to obstetric complications including premature rupture of membranes, placental abruption, preeclampsia, and fetal death.24 Adverse neonatal outcomes associated with prenatal maternal opioid use include preterm birth,24–28 small for gestational age infants,24,26–28 reduced head circumference,28 and sudden infant death syndrome.29 While a recent meta-analysis showed no significant impairment in neurobehavioral and developmental outcomes in children exposed to chronic opioids in utero, more research is required on this topic.30
Limited research has examined the association between opioid use during pregnancy and the risk of congenital malformations, with the few published studies generating conflicting findings.17,31–34 While some have identified an increased risk of cardiac, neural tube and abdominal wall defects,32,33 others have not.17,34,35 A recent ecological study using data from 20 US states identified an association between areas of high maternal opioid use and an increasing prevalence of gastroschisis (a congenital anomaly of the abdominal wall).36 From 2006 to 2015, the prevalence of gastroschisis was 1.6 times higher in areas with high opioid prescription rates compared to areas with low prescription rates.36 This finding has yet to be replicated in larger studies.
It is important to keep in mind that most studies examining associations between maternal opioid use and fetal outcomes are likely to suffer from biases. Chief among them is confounding by indication, in which the clinical indication for the drug, or circumstances surrounding the use of the drug, are also related to the outcome.37 In other words, women who use opioids in pregnancy may have coexisting conditions (e.g. use of other substances, medical or psychiatric illnesses, poor nutrition, etc.), or disrupted social situations that could predispose to poor birth outcomes. Therefore, a major challenge in assessing opioid-related neonatal outcomes is isolating the effects of opioids from other potential confounders. In addition, it is unknown whether intermittent in utero exposure to illicit opioids has different effects on a developing fetus than consistent exposure to OAT throughout the duration of pregnancy.
Neonatal abstinence syndrome
NAS is a drug withdrawal syndrome in babies born to mothers who used opioids in pregnancy.38 It is characterized by gastrointestinal (poor feeding, vomiting, and diarrhea), autonomic (diaphoresis, tachypnea, temperature dysregulation) and central nervous system (tremors, irritability, crying, and seizures) disturbances.38,39 It typically begins in the first 72 h following delivery and can last weeks. However, most cases are self-limited and resolve with appropriate treatment within seven days.38
Today in North America, one child is born every 15 min with signs of neonatal opioid withdrawal.40 Over the last two decades, the incidence of NAS has risen between 5- and 15-fold, and disproportionately in rural areas.9,41 NAS is associated with significant healthcare utilization and costs—over $500 million per year in the USA in 2016—as most babies require extended hospital stays, many in the neonatal intensive care unit (NICU).9,42,43 While the rise in NAS mirrors the increasing prevalence of opioid use in pregnancy, there may be other factors at play. First, there may be an element of diagnostic bias whereby providers are more likely to diagnose NAS because of increasing awareness of the ongoing opioid epidemic. Second, studies have also demonstrated higher rates of NAS in babies of mothers who take opioids with other co-prescribed drugs: antidepressants, benzodiazepines, and gabapentin.44 Maternal use of antidepressants in particular has been linked to a neonatal withdrawal syndrome similar to NAS even in the absence of maternal opioid use.45
Babies with NAS are treated in a variety of hospital settings: newborn nursery, pediatric ward, or NICU. While the NICU provides the highest level of monitoring, it also disrupts the mother–baby dyad and interferes with breastfeeding. “Rooming-in”, a practice where the baby is kept in a crib at the mother’s bedside, has been shown to be an important nonpharmacologic intervention for babies with NAS.46 A US-based study showed that a coordinated treatment program for NAS centered around rooming-in led to a four-day decrease in hospital length of stay, less morphine use, and more than a 50% decrease in hospital costs.47 However, three-quarters of the mothers on OAT in the study were taking buprenorphine, which too might explain the observed decreases in neonatal length of stay and morphine use.47 In addition, such a program may be difficult to implement in settings where pediatric and obstetric services are not located in the same physical location.
Babies with NAS are monitored for withdrawal symptoms using the modified Finnegan Neonatal Abstinence Scoring System. While most are treated with oral morphine, emerging data suggest that buprenorphine may be just as good or possibly more effective. The Blinded Buprenorphine or Neonatal Morphine Solution (BBORN) trial was a single-center randomized controlled trial comparing oral morphine to buprenorphine in the treatment of NAS. The median duration of treatment (15 days vs. 28 days, p < 0.001) and length of hospital stay (21 days vs. 33 days, p < 0.001) were shorter for infants treated with buprenorphine compared to morphine.48 The rates of adverse events were similar between the two groups, although the study was underpowered to detect safety differences.48 However, there are concerns regarding the external generalizability of the BBORN study because of the small sample size (n = 63), exclusion of preterm and breastfeeding infants, and infants whose mothers were taking benzodiazepines in the 30 days prior to birth.48
Postpartum opioid use and breastfeeding
In addition to opioids prescribed during pregnancy, there has been a substantial increase in opioids prescribed to mothers following childbirth. While there is regional variation in prescribing practices, in some jurisdictions up to 30% of women are prescribed opioids following vaginal delivery, and more than 80% following caesarean delivery.49 In addition, some studies have shown that the amount of opioids prescribed postpartum exceeds what is required for adequate pain control.50,51
There is no “standard” number of tablets or duration of therapy appropriate for postpartum analgesia. Therefore, opioids should be prescribed on a case-by-case basis taking into consideration individual needs. One study showed that an individualized shared-decision making approach reduced the quantity of opioids prescribed to postpartum women by 50%.52
It is estimated that hundreds of thousands of women breastfeed while taking opioids each year. Most of these women are opioid-naïve, and some are at risk of persistent opioid use.51,53 US data suggest approximately 1 to 2% of opioid-naive women who receive a first opioid prescription postpartum go on to exhibit patterns of persistent use.54 Previously identified risk factors for persistent opioid use in postpartum women include substance abuse, psychiatric conditions, and initial prescriptions with high opioid milligram equivalents.54 The extent to which new maternal postpartum opioid use may lead to harm for both mother and baby is an area of much needed research.
Opioid transfer into breastmilk
Opioids can pass into the breast milk leading to small quantities ingested by breastfeeding infants. The amount ingested is best quantified by the relative infant dose (RID): the average daily dose of drug ingested by the infant expressed as a percentage of the weight-adjusted average maternal daily dose.55 An RID of 100% means that the infant receives the same daily dose per kilogram as the mother. For most drugs, an RID of 10% or less is considered the safety cutoff for breastfeeding.55 The RIDs of most opioids range from approximately 1% to 7% (Table 3).55 Therefore, under typical circumstances, infants are exposed to low amounts of opioids through breastfeeding.
Table 3.
Approximate relative infant dose of opioids.63
| Opioid | Primary metabolic pathway | RID (%)a |
|---|---|---|
| Morphine | UGT2B7 | 2.5–7.5 |
| Codeine | CYP2D6 | 0.3–1.2 |
| Oxycodone | CYP3A4 (2D6, minor) | 2.6–7.6 |
| Tramadol | CYP2D6 | 2.3 |
| Fentanyl | CYP3A4 | 1.2 |
| Hydromorphone | UGT | 0.7 |
| Hydrocodone | CYP2D6/UGT | 1.6–3.7 |
| Methadone | CYP3A4/2B6 | 1.2–7 |
| Buprenorphine | CYP3A4 | 0.4 |
Enzymes responsible for opioid metabolism and estimated relative infant dose of opioids expected during breastfeeding.
RID: relative infant dose; CYP: cytochrome P450 enzymes; UGT: UDP-glucuronyltransferase.
aData from Lactmed: https://toxnet.nlm.nih.gov/newtoxnet/lactmed.htm, and e-lactancia: www.e-lactancia.org/
Neonatal opioid toxicity from breastfeeding
Most major societies recommend exclusive breastfeeding for all newborns in the first six months of life.56 This recommendation should not be altered for women taking opioids postpartum. Despite only small amounts of opioids passed into the breastmilk, concerns exist about the potential for neonatal opioid toxicity via breastfeeding. Opioids have a low therapeutic index (ratio of toxic dose to therapeutic dose) and there have been a few scattered cases interpreted as instances of neonatal opioid toxicity from breastfeeding.57,58
In one notable case, a 13-day-old breastfeeding child died of a respiratory arrest secondary to opioid toxicity while the mother was taking Tylenol #3 (codeine/paracetamol combination).57,58 While the interpretation of this case has been disputed,59–63 it led major regulatory bodies including Health Canada,64 the United States Food and Drug Administration,65 and the European Medicines Agency,66 to caution against codeine use by nursing mothers. In its place, more potent opioids such as oxycodone and hydromorphone are now increasingly prescribed following childbirth.49,67 This shift in practice may place new mothers at greater risk of persistent opioid use and addiction, and may also pose a hazard to toddlers in the home due to accidental ingestion.68
Despite the above concerns, instances of neonatal opioid toxicity from breastfeeding are exceedingly rare.63,69 Mothers should generally however, limit the duration of opioid use during breastfeeding (two to three days is suggested) and to the lowest effective dose because of the absence of long-term safety data, as well as the potential for maternal harm.55,63
Breastfeeding while taking opioid agonist therapy
Women who take OAT (methadone and buprenorphine) should be encouraged to breastfeed in conjunction with close monitoring of the mother–baby dyad. Infants in this scenario have typically been exposed to opioids in utero and may have different sensitivities. Breastfeeding encourages bonding, promotes maternal confidence, and may in fact mitigate neonatal withdrawal symptoms.70
In addition, the amount of methadone or buprenorphine ingested through breastfeeding represents a small fraction of the weight-based dose (RID) for infants.55 A breast-fed infant of a mother taking methadone might receive 15% to 45% of the lowest starting dose of methadone appropriate for an infant; for buprenorphine, that number is closer to 1% to 4%.55
Conclusions
Amid increasing rates of opioid use in pregnancy, a concerted public health effort is needed to treat affected women and their children. Early universal screening programs for substance use and referral to specialized multidisciplinary care have the potential to improve both maternal and neonatal outcomes. The peripartum period affords a unique opportunity to screen and identify women using opioids. By taking advantage of this brief window, clinicians can support women and their families and engage them in appropriate care.
We are in the infancy of learning about the maternal and neonatal effects of opioids used during pregnancy and post-partum. Well-designed obstetric and neonatal research is needed to examine both immediate and long-term outcomes. Key areas for future work are in maternal addiction, reproductive toxicology, neurobehavioral outcomes in neonates, and the safety of opioids while breastfeeding. The challenge is designing studies to account for the complex socioeconomic factors associated with opioid use in pregnancy and other in utero exposures that too, may impact health outcomes.
Footnotes
Contributorship: JZ and DJ developed the idea and structure for the article. JZ performed the literature review and wrote the first draft of the article. JZ and DJ reviewed and edited the article and approved the final version.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: JZ has received payments for medicolegal opinions regarding the safety and effectiveness of analgesics, including opioids; DJ is an unpaid member of Physicians for Responsible Opioid Prescribing (PROP), which is sometimes cast as an “anti-opioid” group but in actuality is invested in safer and more evidence-based opioid prescribing. DJ is also a member of the American College of Medical Toxicology. Both PROP and ACMT have publicly available positions related to opioid prescribing. DJ has received payment for lectures and medicolegal opinions regarding the safety and effectiveness of analgesics, including opioids.
Ethical approval: Not applicable.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: JZ.
Informed consent: Not applicable.
ORCID iD: Jonathan Zipursky https://orcid.org/0000-0002-9776-807X
References
- 1.Gomes T, Tadrous M, Mamdani MM, et al. The burden of opioid-related mortality in the United States. JAMA Netw Open 2018; 1: e180217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudd RA, Seth P, David F, et al. Increases in drug and opioid-involved overdose deaths – United States, 2010-2015. MMWR Morb Mortal Wkly Rep 2016; 65: 1445–1452. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC). Changes in opioid prescribing practices. Opioid overdose, www.cdc.gov/drugoverdose/data/prescribing/prescribing-practices.html (2019, accessed 15 August 2020).
- 4.Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg 2017; 152: e170504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gomes T, Mamdani MM, Paterson JM, et al. Trends in high-dose opioid prescribing in Canada. Can Fam Physician 2014; 60: 826–832. [PMC free article] [PubMed] [Google Scholar]
- 6.Ailes EC, Dawson AL, Lind JN, et al. Opioid prescription claims among women of reproductive age–United States. MMWR Morb Mortal Wkly Rep 2015; 64: 2008–2012. [PMC free article] [PubMed] [Google Scholar]
- 7.Desai RJ, Hernandez-Diaz S, Bateman BT, et al. Increase in prescription opioid use during pregnancy among Medicaid-enrolled women. Obstet Gynecol 2014; 123: 997–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patrick SW, Schumacher RE, Benneyworth BD, et al. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA 2012; 307: 1934–1940. [DOI] [PubMed] [Google Scholar]
- 9.Turner SD, Gomes T, Camacho X, et al. Neonatal opioid withdrawal and antenatal opioid prescribing. C Open 2015; 3: E55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baldini AV, Korff M, Lin EHB. A review of potential adverse effects of long-term opioid therapy: a practitioner’s guide. Prim Care Companion CNS Disord 2012; 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maeda A, Bateman BT, Clancy CR, et al. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology 2014; 121: 1158–1165. [DOI] [PubMed] [Google Scholar]
- 12.Wong S, Ordean A, Kahan M, et al. SOGC clinical practice guidelines: Substance use in pregnancy: no. 256, April 2011. Int J Gynaecol Obstet 2011; 114: 190–202. [DOI] [PubMed] [Google Scholar]
- 13.ACOG Committee Opinion No. 742: postpartum pain management. Obstet Gynecol 2018; 132: e35–e43. [DOI] [PubMed]
- 14.Coleman-Cowger VH, Oga EA, Peters EN, et al. Accuracy of three screening tools for prenatal substance use. Obstet Gynecol 2019; 133: 952–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ondersma SJ, Chang G, Blake‐Lamb T, et al. Accuracy of five self‐report screening instruments for substance use in pregnancy. Addiction 2019; 114: 1683–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Center for Substance Abuse Treatment. Medication-assisted treatment for opioid addiction during pregnancy. Treatment Improvement Protocol (TIPS) Series. Subst Abus Ment Heal Serv Adm 2005; 43: 211–224. [Google Scholar]
- 17.Zedler BK, Mann AL, Kim MM, et al. Buprenorphine compared with methadone to treat pregnant women with opioid use disorder: a systematic review and meta-analysis of safety in the mother, fetus and child. Addiction 2016; 111: 2115–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Minozzi S, Amato L, Bellisario C, et al. Maintenance agonist treatments for opiate-dependent pregnant women. Cochrane Database Syst Rev 2013. [DOI] [PubMed] [Google Scholar]
- 19.Brogly SB, Saia KA, Walley AY, et al. Prenatal buprenorphine versus methadone exposure and neonatal outcomes: systematic review and meta-analysis. Am J Epidemiol 2014; 180: 673–686. [DOI] [PubMed] [Google Scholar]
- 20.Debelak K, Morrone WR, O’Grady KE, et al. Buprenorphine + naloxone in the treatment of opioid dependence during pregnancy-initial patient care and outcome data. Am J Addict 2013; 22: 252–254. [DOI] [PubMed] [Google Scholar]
- 21.Wiegand SL, Stringer EM, Stuebe AM, et al. Buprenorphine and naloxone compared with methadone treatment in pregnancy. Obstet Gynecol 2015; 125: 363–368. [DOI] [PubMed] [Google Scholar]
- 22.Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med 2006; 144: 127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hudak ML, Tan RC, Committee on Drugs, et al. Neonatal drug withdrawal. Pediatrics 2012; 129: e540–560. [DOI] [PubMed] [Google Scholar]
- 24.Källén B, Borg N, Reis M. The use of central nervous system active drugs during pregnancy. Pharmaceuticals (Basel) 2013; 6: 1221–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kelly L, Dooley J, Cromarty H, et al. Narcotic-exposed neonates in a First Nations population in northwestern Ontario: incidence and implications. Can Fam Physician 2011; 57: e441. [PMC free article] [PubMed] [Google Scholar]
- 26.Ludlow JP, Evans SF, Hulse G. Obstetric and perinatal outcomes in pregnancies associated with illicit substance abuse. Aust N Z J Obstet Gynaecol 2004; 44: 302–306. [DOI] [PubMed] [Google Scholar]
- 27.Cleary BJ, Donnelly JM, Strawbridge JD, et al. Methadone and perinatal outcomes: a retrospective cohort study. Am J Obstet Gynecol 2011; 204: 139.e1–9. [DOI] [PubMed] [Google Scholar]
- 28.Greig E, Ash A, Douiri A. Maternal and neonatal outcomes following methadone substitution during pregnancy. Arch Gynecol Obstet 2012; 286: 843–851. [DOI] [PubMed] [Google Scholar]
- 29.Burns L, Conroy E, Mattick RP. Infant mortality among women on a methadone program during pregnancy. Drug Alcohol Rev 2010; 29: 551–556. [DOI] [PubMed] [Google Scholar]
- 30.Baldacchino A, Arbuckle K, Petrie DJ, et al. Neurobehavioral consequences of chronic intrauterine opioid exposure in infants and preschool children: a systematic review and meta-analysis. BMC Psychiatry 2014; 14: 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bracken MB, Holford TR. Exposure to prescribed drugs in pregnancy and association with congenital malformations. Obstet Gynecol 1981; 58: 336–344. [PubMed] [Google Scholar]
- 32.Broussard CS, Rasmussen SA, Reefhuis J, et al. Maternal treatment with opioid analgesics and risk for birth defects. Am J Obstet Gynecol 2011; 204: 314.e1–11. [DOI] [PubMed] [Google Scholar]
- 33.Yazdy MM, Mitchell AA, Tinker SC, et al. Periconceptional use of opioids and the risk of neural tube defects. Obstet Gynecol 2013; 122: 838–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nezvalová-Henriksen K, Spigset O, Nordeng H. Effects of codeine on pregnancy outcome: results from a large population-based cohort study. Eur J Clin Pharmacol 2011; 67: 1253–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fishman B, Daniel S, Koren G, et al. Pregnancy outcome following opioid exposure: a cohort study. PLoS One 2019; 14: e0219061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Short TD, Stallings EB, Isenburg J, et al. Gastroschisis trends and ecologic link to opioid prescription rates – United States, 2006-2015. MMWR Morb Mortal Wkly Rep 2019; 68: 31–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kyriacou DN, Lewis RJ. Confounding by indication in clinical research. JAMA 2016; 316: 1818–1819. [DOI] [PubMed] [Google Scholar]
- 38.McQueen K, Murphy-Oikonen J. Neonatal abstinence syndrome. N Engl J Med 2016; 375: 2468–2479. [DOI] [PubMed] [Google Scholar]
- 39.Palla MR, Khan G, Haghighat ZM, et al. EEG findings in infants with neonatal abstinence syndrome presenting with clinical seizures. Front Pediatr 2019; 7: 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dramatic increases in maternal opioid use and neonatal abstinence syndrome. National Institute on Drug Abuse, www.drugabuse.gov/related-topics/trends-statistics/infographics/dramatic-increases-in-maternal-opioid-use-neonatal-abstinence-syndrome (2019, accessed 3 February 2020).
- 41.Ko JY, Patrick SW, Tong VT, et al. Incidence of neonatal abstinence syndrome – 28 States, 1999-2013. MMWR Morb Mortal Wkly Rep 2016; 65: 799–802. [DOI] [PubMed] [Google Scholar]
- 42.Winkelman TNA, Villapiano N, Kozhimannil KB, et al. Incidence and costs of neonatal abstinence syndrome among infants with Medicaid. Pediatrics 2018; 141: 2004–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Strahan AE, Guy GP, Bohm M, et al. Neonatal abstinence syndrome incidence and health care costs in the United States, 2016. JAMA Pediatr 2020; 174: 200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huybrechts KF, Bateman BT, Desai RJ, et al. Risk of neonatal drug withdrawal after intrauterine co-exposure to opioids and psychotropic medications: cohort study. BMJ 2017; 358: j3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moses-Kolko EL, Bogen D, Perel J, et al. Neonatal signs after late in utero exposure to serotonin reuptake inhibitors: literature review and implications for clinical applications. JAMA 2005; 293: 2372–2383. [DOI] [PubMed] [Google Scholar]
- 46.Sanlorenzo LA, Stark AR, Patrick SW. Neonatal abstinence syndrome: an update. Curr Opin Pediatr 2018; 30: 182–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Holmes AV, Atwood EC, Whalen B, et al. Rooming-in to treat neonatal abstinence syndrome: improved family-centered care at lower cost. Pediatrics 2016; 137. [DOI] [PubMed] [Google Scholar]
- 48.Kraft WK, Adeniyi-Jones SC, Chervoneva I, et al. Buprenorphine for the treatment of the neonatal abstinence syndrome. N Engl J Med 2017; 376: 2341–2348. doi:10.1056/NEJMoa1614835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Badreldin N, Grobman WA, Chang KT, et al. Opioid prescribing patterns among postpartum women. Am J Obstet Gynecol 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol 2017; 130: 29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Osmundson SS, Schornack LA, Grasch JL, et al. Postdischarge opioid use after cesarean delivery. Obstet Gynecol 2017; 130: 36–41. [DOI] [PubMed] [Google Scholar]
- 52.Prabhu M, McQuaid-Hanson E, Hopp S, et al. A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol 2017; 130: 42–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Osmundson SS, Min JY, Wiese AD, et al. Opioid prescribing after childbirth and risk for serious opioid-related events: a cohort study. Ann Intern Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Peahl AF, Dalton VK, Montgomery JR, et al. Rates of new persistent opioid use after vaginal or cesarean birth among US women. JAMA Netw Open 2019; 2: e197863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ito S. Opioids in breast milk: pharmacokinetic principles and clinical implications. J Clin Pharmacol 2018; 58: S151–S163. [DOI] [PubMed] [Google Scholar]
- 56.Critch JN. Canadian Paediatric Society N and GC. Nutrition for healthy term infants, birth to six months: an overview. Paediatr Child Health 2013; 18: 206–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Koren G, Cairns J, Chitayat D, et al. Pharmacogenetics of morphine poisoning in a breastfed neonate of a codeine-prescribed mother. Lancet 2006; 368: 704. [DOI] [PubMed] [Google Scholar]
- 58.Madadi P, Koren G, Cairns J, et al. Safety of codeine during breastfeeding: fatal morphine poisoning in the breastfed neonate of a mother prescribed codeine. Can Fam Physician 2007; 53: 33–35. [PMC free article] [PubMed] [Google Scholar]
- 59.Ferner RE. Did the drug cause death? Codeine and breastfeeding. Lancet 2008; 372: 606–608. [DOI] [PubMed] [Google Scholar]
- 60.Willmann S, Edginton AN, Coboeken K, et al. Risk to the breast-fed neonate from codeine treatment to the mother: a quantitative mechanistic modeling study. Clin Pharmacol Ther 2009; 86: 634–643. [DOI] [PubMed] [Google Scholar]
- 61.Bateman DN, Eddleston M, Sandilands E. Codeine and breastfeeding. Lancet 2008; 372: 625–626. [DOI] [PubMed] [Google Scholar]
- 62.Young M. Morphine in breast milk. Can Fam Physician 2007; 53: 1005; author reply 1005–1006. [PMC free article] [PubMed] [Google Scholar]
- 63.Zipursky J, Juurlink DN. The implausibility of neonatal opioid toxicity from breastfeeding. Clin Pharmacol Ther 2020. [DOI] [PubMed] [Google Scholar]
- 64.Lau C. Health Canada endorsed important safety information on TYLENOL with codeine products. Government of Canada: recalls and safety alerts, www.healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2008/14526a-eng.php (2008, accessed January 27, 2020).
- 65.Use of codeine and tramadol products in breastfeeding women – questions and answers. U.S. Food & Drug Administration: Drug Safety and Availability, www.fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm118113.htm (2017, accessed January 27, 2020).
- 66.Codeine not to be used in children below 12 years for cough and cold. European Medicines Agency, www.ema.europa.eu/en/medicines/human/referrals/codeine-containing-medicinal-products-treatment-cough-cold-paediatric-patients#all-documents-section (2015, accessed January 27, 2020).
- 67.Smolina K, Weymann D, Morgan S, et al. Association between regulatory advisories and codeine prescribing to postpartum women. JAMA 2015; 313: 1861–1862. [DOI] [PubMed] [Google Scholar]
- 68.Finkelstein Y, Macdonald EM, Gonzalez A, et al. Overdose risk in young children of women prescribed opioids. Pediatrics 2017; 139. [DOI] [PubMed] [Google Scholar]
- 69.Juurlink DN, Gomes T, Guttmann A, et al. Postpartum maternal codeine therapy and the risk of adverse neonatal outcomes: a retrospective cohort study. Clin Toxicol (Phila) 2012; 50: 390–395. [DOI] [PubMed] [Google Scholar]
- 70.Dieterich CM, Felice JP, O’Sullivan E, et al. Breastfeeding and health outcomes for the mother-infant dyad. Pediatr Clin North Am 2013; 60: 31–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.British Columbia Centre on Substance Use, B.C. Ministry of Health BCM of, Mental Health and Addictions & PSB. Guideline for the clinical management of opioid use disorder—pregnancy supplement. 2018; 1–32. www.bccsu.ca/care-guidance-%0Apublications/