FIGURE 1.
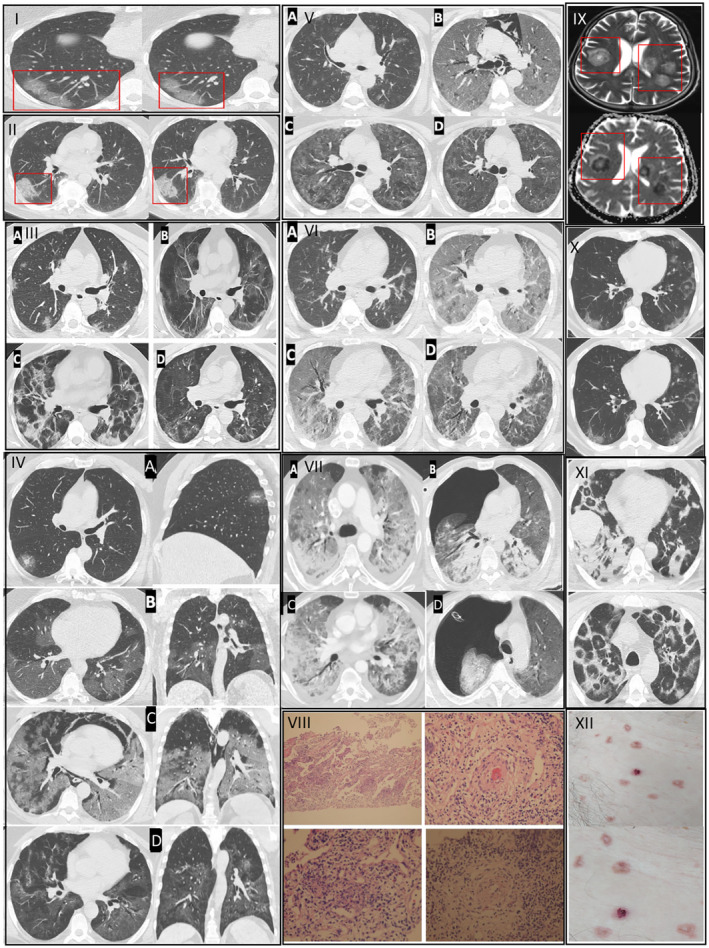
Consists of seven cases with variable stages of COVID‐19 and examples of early and severe endotheliitis in the brain, pulmonary and skin tissues. Histopathological and radiological findings of pneumonitis changed depending on the phase of the disease (early, progressive, severe and dissipative, respectively), which leads to a divergence in treatment groups. Examples of patients who were convenient for Group A treatment are depicted in Sections I and II. I. Case 1. HRCT images showed patchy, subpleural and peripheral perivascular ground‐glass opacities, corresponding to the early phase of pneumonitis. She received Group A treatment. GGOs in transaxial images were located in the subpleural area, where the microvascular endoteheliitis and endothelial destructions mostly likely occur because of the interaction with toxic plasma in the capillaries of pulmonary interstitial space. II. Case 2. HRCT images showed characteristics of an early phase COVID‐19 pneumonitis (end‐capillary microangiopathy, explained in 1I) and perivascular consolidation. It appeared as the continuation of the crazy‐paving pattern, which was demonstrated by the thickening in inter‐lobular and intra‐lobular septa. Lung involvement was limited and monofocal. Hence, the patient received Group A treatment. An example of a patient who was convenient for Group B treatment is depicted in Section III. III. Case 3. Transaxial HRCT image in the first day of positivity shows bilateral and patchy nodulary GGOs as expected in early phase (IIIa). On the 5th day of positivity, affected pulmonary areas were advanced into scattered consolidations (IIIb). This appearance was noted as the progressive phase of pneumonitis and was considered as the representation of clinical deterioration clinically (ie, dyspnoea, respiratory failure). On the 15th day of positivity, fibroreticular consolidations were conspicuous (IIIc). The dissipative phase was the healing process, characterised by the resolution in lung parenchyma and residual GGO, observed after 35 days of positivity (IIId). Parenchymal bands, originated from previous fibroreticular proliferation, were also visible (IIId). If the patients have a tendency of severe phase and/or unresponsiveness to Group B therapy, Group C treatment was used. Representative cases of this group are shown in Sections IV–VII This group of patients also undergo early and progressive phases of COVID‐19 but they also showed further deterioration of lung involvement and endothelial damage, therefore, they received the last group of treatment. For the description of early and progressive phases, Sections I, II and can be referred. IV. Case 4. Coronal, sagittal and axial planes of HRCT images initially showed small GGO with a local subpleural sparing, particularly around the microvascular area on the first day of positivity (IVa). On the fifth day of treatment, increased GGOs were visible in the progressive phase (IVb). After 18 days of positivity, pneumomediastinum, Diffuse Alveolar Damage (DAD) and ARDS were seen in a severe phase (IVc). Lastly, the dissipative phase was seen, after 30 days of positivity, with residual fibrotic parenchyma (IVd). V. Case 5. The first HRCT image, on the second day of positivity, showed COVID‐19‐related bilateral and multifocal nodular GGOs (Va). After 10 days of positivity, DAD developed along with ARDS and pneumomediastinum characterised with the severe phase (Vb). She recovered and discharged after 30 days of positivity with the dissipative phase (Vc). The regression in pulmonary lesions was visible on the HRCT image 2 months after diagnosis (Vd). VI. Case 6. HRCT image showed moderate pneumonia in the early phase (VIa). After 12 days of positivity, the severe phase develops with DAD and ARDS (VIb). On the 25th day of positivity, recovery was observed in the dissipative phase (VIc). The extent of improvement in pulmonary lesions can be noticed in VId, which was 40 days after the diagnosis. VII. Case 7. First HRCT showed ARDS pattern with dense consolidations (VIIa). Pneumothorax developed after 2 weeks from diagnosis (VIIb). In addition to the respiratory failure, haemorrhagical intracranial areas were seen in the T2‐weighted MRI. (VIIc). He was lost on the 20th day of positivity. Representative histopathological and radiological images of endotheliitis are seen in Sections VIII, IX, X, XI. VIII Haematoxylin&Eosin‐stained sections from representative areas of lung parenchyma were seen with the mixt‐type inflammatory‐cell infiltration of lung tissue and exudative capillaritis with thickened microvascular walls. Interstitial and intra‐alveolar proliferation of fibroblasts is noted. IX. Diffusion MRI of the head image of COVID‐19 positive patient showing characteristic COVID‐19 related endotheliitis causing characteristic lesions and intracranial haemorrhage. X. Early endotheliitis. XI. Late endotheliitis. XII. Papulovesicular eruptions as the skin manifestations of COVID‐19‐related endotheliitis
