Abstract
During the COVID‐19 pandemic, Portugal has experienced three distinct SARS‐CoV‐2 infection waves. We previously documented the prevalence of SARS‐CoV‐2 immunity, measured by specific antibodies, in September 2020, 6 months after the initial moderate wave. Here, we show the seroprevalence changes 6 months later, up to the second week of March 2021, shortly following the third wave, which was one of the most severe in the world, and 2 months following the start of the vaccination campaign. A longitudinal epidemiological study was conducted, with a stratified quota sample of the Portuguese population. Serological testing was performed, including ELISA determination of antibody class and titers. The proportion of seropositives, which was 2.2% in September 2020, rose sharply to 17.3% (95% CI: 15.8–18.8%) in March 2021. Importantly, circulating IgG and IgA antibody levels were very stable 6 months after the initial determination and up to a year after initial infection, indicating long‐lasting infection immunity against SARS‐CoV‐2. Moreover, vaccinated people had higher IgG levels from 3 weeks post‐vaccination when compared with previously infected people at the same time post‐infection.
Keywords: antibodies, COVID‐19, longitudinal survey, long‐lasting immunity, vaccination
During the COVID‐19 pandemic, Portugal experienced three distinct SARS‐CoV‐2 infection waves. We determined the presence of antibodies after the first wave, September 2020 resulting in 2.2% seropositivity, and after the 2/3 wave in March 2021, including a contribution of the vaccination campaign, seroprevelance of 17.3%. Longitudional survey from individuals infected during the first wave indicated long‐lasting immunity, slowly waning, 1 year after infection.

Introduction
On January 30, 2020, the WHO declared that the outbreak SARS‐CoV‐2 constituted a Public Health Emergency of International Concern (PHEIC), followed by its characterization as a pandemic on March 11, 2020. Since then, the infection has spread to almost every country in the world, with variable attack rates. Accurate estimates of anti‐SARS‐CoV‐2 antibody seroprevalence in the population remain critical to inform policy to contain and bring to an end the ongoing pandemic. Seroprevalence studies can uniquely determine population exposure and correlate with the quality of immunity, and are more inclusive than PCR‐based virus‐detection strategies. For example, they will include the prevalence of asymptomatic and pauci‐symptomatic cases, individuals often missed in symptom‐based infection screenings. Importantly, longitudinal seroprevalence studies provide a quantification of the evolution of exposure over time and associated demographics. Moreover, longitudinal designs can inform the duration of antibody seropositivity. From the start, uncertainties regarding immune response and the duration of immunity against a novel mucosal coronavirus were raised. We now have reports of good levels of antibodies, present at least 6 months post‐infection, and T cell immunity [1, 2, 3, 4, 5, 6, 7, 8, 9, 10]. Nevertheless, the majority of these studies use specific samples, such as health care workers, and do not provide a complete cross‐sectional picture of the population.
The true level of incidence of the infection is difficult to ascertain from official case reports, as has been shown by serological prevalence studies from multiple countries [11, 12, 13, 14]. For example, we conducted a national level study based on a stratified quota sample of the prevalence of people positive for antibodies against SARS‐CoV‐2, in September 2020, before the second wave of infection, as an indicator of past infection, and concluded that three to four times as many people had been infected than the official case number reports [15]. Moreover, this factor of extra infections was different among age groups, being approximately ninefold in people younger than 18 years. This difference between the number of registered cases and actual infections can be due to the number of asymptomatic or mild infections that go undetected, and overall testing policies.
Here, we report the results of a follow‐up seroprevalence study performed from March 1 to March 17, 2021, after the large increase of cases seen in January. Our primary objective was to assess the proportion of people with SARS‐CoV‐2 specific antibodies in Portugal, and how this varied by age group and population density. An important issue to determine an accurate estimate of the proportion of previous infections is how long antibodies can be detected after viral infection [1, 7, 17, 18]. Thus, in this follow‐up study, we also analyzed the antibody levels of people, who had tested positive in the first study, many of whom were infected during the first wave, up to ∼1 year before. Finally, because the vaccine rollout was initiated in Portugal at the end of December, we also kept track of the fraction of people vaccinated. Altogether, we found a 17.3% seroprevalence level in Portugal and that the vast majority of people maintain detectable antibodies, with some of these people almost 1 year after initial infection. This result provides insights into SARS‐CoV‐2‐specific antibody waning.
Results
SARS‐CoV‐2 antibody seroprevalence in the Portuguese population
In many countries, the epidemic proceeded in waves. Portugal is a good example of this pattern (Fig. 1A). The first case of SARS‐CoV‐2 infection was officially reported on March 2, 2020, at the beginning of the first wave, which led to multiple early containment measures. There was a second much larger rise in the incidence of infection in the months of October‐November, followed by a severe third wave during January 2021, when Portugal was for a few weeks one of the countries in the world with the most new deaths per million people (Fig. 1B).
Figure 1.
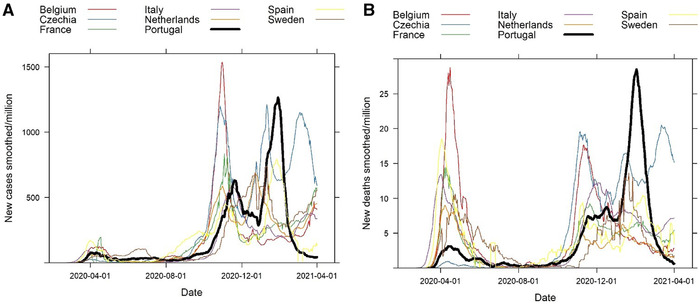
Comparison of the evolution of the COVID‐19 pandemic in Portugal and other selected European countries. Overview regarding SARS‐CoV‐2 infections for counties indicated, obtained from March 1, 2020 to April 1, 2021. (A) Number of new cases per million and (B) number of new deaths per million. These figures demonstrate the severity of the large third wave of cases in January in Portugal (black line) when compared with other select neighboring countries (Spain, France, Italy) and other countries of similar population size (Belgium, Czechia, Netherlands, and Sweden). Data from “Our World in Data” (https://ourworldindata.org/coronavirus).
We conducted a follow‐up to our seroprevalence study of September 2020 [15], with blood collections for serological assays between March 1 and March 17, 2021, when there were ∼810,000 confirmed cases in Portugal (with 58.3% of these cases occurring in December and January, Fig. 1A [16]). From the participants in that study, we recruited 2172 people, who had previously tested negative (negative cohort ‐ NC), and 263 people, who had previously tested positive (PC). In the NC, 43.6% were men (n = 948), and 10.3% (n = 224) were younger than 18, 46.3% (n = 1006) were between 18 and 54 years old, and 43.4% (n = 942) were 55 years or older. We asked about the participant status regarding vaccination against SARS‐CoV‐2 and 173 (7.1%) participants indicated that they had at least one dose of a vaccine (156 in the NC, and 17 in the PC). In Table 1, we show the characteristics of the two cohorts.
Table 1.
Socio‐demographic characteristics of the study sample
| Cohort "NC" | Cohort "PC" | ||||
|---|---|---|---|---|---|
| n | % | N | % | ||
| Sex | |||||
| Male | 948 | 43.6% | 126 | 47.9% | |
| Female | 1224 | 56.4% | 137 | 52.1% | |
| Age categories | |||||
| <18 years | 224 | 10.3% | 40 | 15.2% | |
| 18‐54 years | 1006 | 46.3% | 132 | 50.2% | |
| ≥55 years | 942 | 43.4% | 91 | 34.6% | |
| Population density | |||||
| Low or Medium | 1162 | 53.5% | 100 | 38.0% | |
| High | 1010 | 46.5% | 163 | 62.0% | |
| Household size | |||||
| 1 person | 390 | 18.0% | 24 | 9.1% | |
| 2 to 4 people | 1649 | 75.9% | 216 | 82.1% | |
| ≥5 people | 133 | 6.1% | 23 | 8.7% | |
| Education | |||||
| Less than high school | 619 | 29.4% | 73 | 27.8% | |
| High school, post high school (no undergraduate degree) | 749 | 35.5% | 73 | 27.8% | |
| Undergraduate or graduate degree | 704 | 33.4% | 108 | 41.1% | |
| Other | 37 | 1.8% | 9 | 3.4% | |
| Occupation | |||||
| Employed | 1272 | 58.6% | 156 | 59.3% | |
| Unemployed | 115 | 5.3% | 13 | 4.9% | |
| Student | 263 | 12.1% | 47 | 17.9% | |
| Retired | 438 | 20.2% | 36 | 13.7% | |
| Other, Disability, Homemaker | 84 | 3.9% | 11 | 4.1% | |
| Professional sector | |||||
| Commerce, Industry and Building | 229 | 18.0% | 28 | 10.6% | |
| Administration / services | 338 | 26.6% | 35 | 13.3% | |
| Education | 190 | 14.9% | 21 | 8.0% | |
| Health | 121 | 9.5% | 22 | 8.4% | |
| Health (no clinic) | 42 | 3.3% | 7 | 2.7% | |
| Transportation | 43 | 3.4% | 3 | 1.1% | |
| Other | 309 | 24.3% | 40 | 15.2% | |
| Current working arrangement (employed workers) | |||||
| Teleworking | 345 | 13.2% | 43 | 27.7% | |
| Physically at work, only in contact with colleagues | 386 | 14.8% | 54 | 34.8% | |
| Physically at work, no contact | 72 | 2.8% | 11 | 7.1% | |
| Physically at work, contact with public | 407 | 15.6% | 43 | 27.7% | |
| Mixed arrangements | 62 | 2.3% | 4 | 2.6% | |
| Body Mass Index | |||||
| Normal or underweight | 905 | 45.9% | 95 | 42.0% | |
| Overweight | 713 | 36.2% | 90 | 39.8% | |
| Obese | 353 | 17.9% | 41 | 18.1% | |
| Smoking status | |||||
| Non‐smoker | 1366 | 64.8% | 198 | 75.3% | |
| Ex‐smoker | 415 | 19.7% | 44 | 16.7% | |
| Smoker | 328 | 15.6% | 21 | 8.0% | |
| Physical Exercise | |||||
| No | 1141 | 52.5% | 138 | 52.5% | |
| Yes | 1031 | 47.5% | 125 | 47.5% | |
| COVID‐19 Vaccine | |||||
| No | 2016 | 92.8% | 246 | 93.5% | |
| Yes | 156 | 7.2% | 17 | 6.5% | |
We tested all participants for specific antibodies against SARS‐CoV‐2 RBD using a commercial assay (see Materials and Methods for details). Not including vaccinated people, there were 2016 people in the NC and 246 people in the PC, of these 214 tested positive in the NC and 239 in the PC. With these results, and adjusting for the strata (age groups and population density of place of residence), as well as sensitivity and specificity of the test, the global seroprevalence found in this study was 13.1% (95% CI: 11.8–14.6%) due to viral infection only (Table 2). In addition, considering the vaccinated people, who had already developed antibodies (more below), the fraction of seropositive in the population increases to 17.3% (95% CI: 15.8–18.8%).
Table 2.
SARS‐CoV‐2 antibody seroprevalence estimates in Portugal, March 2021. Estimates of seroprevalence for the population of Portugal, and by region of population density and age group. The n indicated in the table corresponds to the sample assessed, and is for information purposes
| Total | Non‐vaccinated only | ||||||
|---|---|---|---|---|---|---|---|
| n | Seroprevalence | 95% CI | n | Seroprevalence | 95% CI | ||
| Overall | 2435 | 17.3% | 15.8‐18.8 | 2262 | 13.1% | 11.8‐14.6 | |
| Population density | High (>500/km2) | 1173 | 17.3% | 15.0‐19.6 | 1104 | 13.5% | 11.5‐15.7 |
| Low/Medium (<500/km2) | 1262 | 17.0% | 15.0‐19.0 | 1158 | 12.5% | 10.7‐14.4 | |
| Age group | < 18 years | 264 | 15.0% | 11.0‐19.6 | 264 | 15.0% | 11.0‐19.6 |
| 18‐54 years | 1138 | 20.2% | 17.8‐22.4 | 1047 | 13.8% | 11.7‐15.8 | |
| ≥55 years | 1033 | 14.2% | 12.1‐16.3 | 951 | 10.9% | 9.0‐12.9 | |
Analyzing the results by the strata (Table 2), including all seropositive, whether by viral infection or vaccination, we found similar fraction of seropositivity by population density, 17.3% (95% CI: 15.0%–19.6%) for high density (>500 people/km2) and 17.0% (95% CI: 15.0%–19.0%) for low/medium density (≤500 people/km2). Furthermore, in terms of age groups the seroprevalence was 15.0% (11.0%–19.6%) in people <18 years old, 20.2% (17.8%–22.4%) for the 18–54 years old, and 14.2% (95% CI: 12.1%–16.3%) for ≥55 years old, which reflects the priorities of vaccination early on in the campaign in Portugal. This vaccination bias is clear if we compare these numbers with the seroprevalence estimated from viral infection only: 15.0% (11.0%–19.6%) in people <18 years old, 13.8% (11.7%–15.8%) for the 18–54 years old, and 10.9% (95% CI: 9.0%–12.9%) for ≥55 years old.
Evolution of SARS‐CoV‐2 antibody seroprevalence in the Portuguese population over the past 6 months
When we compare the results of seroprevalence obtained in this study, with its precursor 6 months before, we see that the overall prevalence increased from 2.2% to 13.1%, due to viral infection. The increase in seroprevalence was similar in the younger age group (<18 years) and intermediate age group (18‐54 years) from 2.4% to 15.0% and from 2.3% to 13.8%, respectively; but smaller in the eldest group, from 1.9% to 10.9%. In terms of population density, in September we obtained a significantly higher prevalence in high population density regions, but now the relative gap narrowed, since we found, considering only viral infection, 13.5% prevalence in high‐density regions and 12.5% in the other regions.
It is also interesting to compare the total number of cases estimated by these seroprevalence studies to the official number of cases reported by the Portuguese authorities. In September 2020, we found an overall prevalence of 2.2% o for antibodies against SARS‐CoV‐2 in the Portuguese population, corresponding to about 226,000 people, considering the 10.3 million people living in Portugal. In the current study, we found a prevalence of 13.1% antibody positive due to natural infection, corresponding to about 1,350,000 people. Assuming that it takes an average of 2 weeks from the time of infection for people to become seropositive [19, 20, 21], this seroprevalence reflects the extent of SARS‐CoV‐2 infection in Portugal 2 weeks before each study. Comparing with the cumulative confirmed cases in Portugal (58,243 on September 1, 2020 and 797,525 on February 21, 2021) [16], we can see that the multiplicative factor decreased from more than three to less than two, suggesting a higher testing rate.
In terms of vaccination, there were 0 people in September 2020, before any vaccine had been approved, and there were 7.1% of people who reported being vaccinated in the current study. This value compares well with the reported number of people with at least one dose of vaccination, at 6% on February 28 and 8% on March 14 [22].
Quantification of antibodies against SARS‐CoV‐2
In September 2020, in the first phase of this longitudinal study, we quantified, using our in‐house ELISA assay (see Materials and Methods), the titers of antibodies in 204 people, who also participated in the March 2021 phase of the study. Now, i.e., 6 months following the first determinations, we performed the same quantification in 201 of those same people (for the other 3, no sample was available). Of these, 13 had received at least one dose of a vaccine and were excluded from the analysis. Importantly all 188 (non‐vaccinated) previously screened seropositive persons remained seropositive 6 months later. When comparing antibody levels at the two time periods within each person, we found a reduction in IgM (P = 0.0006) and IgG (P = 0.0095) levels 6 months following the first assessment, but no significant difference in IgA (P = 0.1548; Fig. 2A). One individual had a substantial increase in IgG titer, suggesting reinfection with SARS‐CoV‐2. We next plotted the antibody titers over time since infection (confirmed by PCR or suspected due to symptoms) to provide an overview of the change in antibody levels within an individual since infection (Fig. 2B). Twenty‐two subjects were removed due to an unknown date of infection. Overall, the data demonstrate the longevity of antibodies, up to 12 months after initial infection (Fig. 2B). We calculated the half‐life of antibody decay using a linear mixed‐effect model, and found that t½ ∼ 29 months for IgM, t½ ∼ 28 months for IgG, and no decay for IgA. To account for the initial contraction phase taking place after the peak in antibody production, we separated the participants into two groups, according to how long after infection their antibody titers had been first analyzed: (i) less than 4 months or (ii) more than 4 months since infection, as reported by each individual in the questionnaire. Participants in the first group show a reduction in IgM and IgG levels, but stable IgA levels when we compare the two titer determinations 6 months apart (Fig. 2C). Those participants for whom the first antibody assay was done 5–7 months after infection show more stable levels for IgM and IgG isotypes at the second determination 6 months later (Fig. 2D), while IgA showed a small but significant increase. Collectively, this indicates that during the initial contraction phase, there is some waning of IgM and IgG antibodies levels, which subsequently stabilize resulting in detectable levels anti‐SARS‐CoV‐2 Spike antibodies for the first year after viral infection (Fig. 2).
Figure 2.
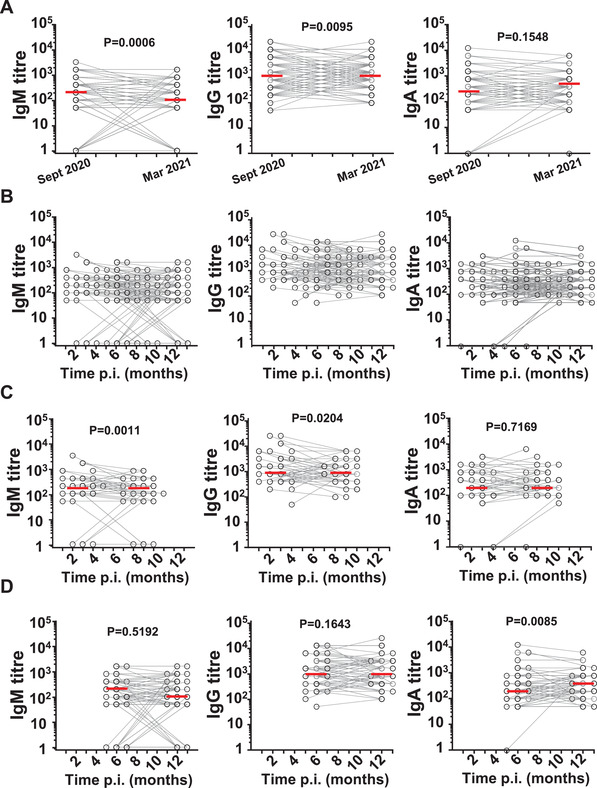
Evolution of antibody levels between the two phases of the longitudinal study. Donors who tested positive for antiSARS‐CoV‐2 RBD antibodies in September 2020 (first symbol) were re‐assessed 6 months later, March 2021 (second symbol), for the level of anti‐SARS‐CoV‐2 RBD antibodies, IgM, IgG, and IgA by ELISA using serial dilutions. A) Comparison of IgM, IgG, and IgA (from left to right in all rows) of the same individuals assayed in the two periods (n = 188), showing a significant decay in IgM and IgG, but not IgA, in a paired analyses over the two time points. (B) Same individuals as (A) but plotting each person's two antibody titer measurements versus time since their infection, which occurred at the time of PCR positive test or symptoms, as reported by the participants. First symbol indicates time from infection for the first titer measurement (in the first phase of the study), connected to the second time point of the same individual 6 months later in the current phase of the study (n = 166). (C) Same as (B) but including only those participants who were infected less than 4 months before the September 2020 serology study (n = 49), showing small but significant early declines in IgM and IgG titers (but not IgA). (D) same as (B) but including only those participants who were infected more than 4 months before the September 2020 serology study (n = 117), showing that from month 5 after infection onwards there was no significant decline in IgM or IgG titers. Together (C) and (D) show that early after infection there is a decline in antibody titers, but this decline slows down or is even absent later on. Red lines indicate average. P‐values for two‐sided Wilcoxon sing‐rank test for matched pairs.
To understand if antibody immunity against SARS‐CoV‐2 had altered after the first wave, we quantified the levels of antibodies for 194 newly infected and non‐vaccinated people, of whom 178 knew an approximate date of infection. These people who tested positive only in the second phase of the study had levels of IgG and IgA antibodies higher than the titers detected in the participants who were seropositive in the first phase of the study (Fig. 3A). To try to understand this difference, we note that the mean time since infection until assessment in the study in September was 151 days, whereas for the newly positive people in March, this median time was 76 days. This is consistent with the first phase of the study occurring several months after the first wave, in March‐April 2020; and the second screening occurring shortly after the severe third wave in January 2021. Grouping the people according to months since their infection indicated similar antibody levels after the first or second and third waves (Fig. 3B). This confirms that the quality of the antibody response against SARS‐CoV‐2 remained constant after the first wave.
Figure 3.
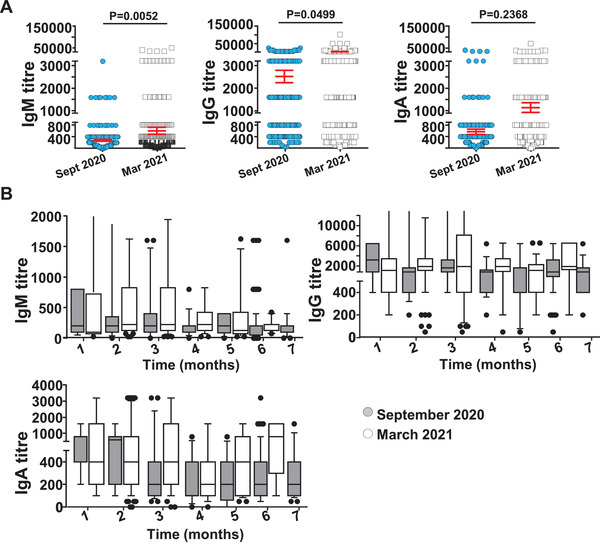
Comparison of antibody levels for people seropositive for the first time in September 2020 or March 2021 phases of the study. Serum samples from individuals infected with SARS‐CoV‐2 in the first 6 months of the pandemic (and thus were positive in the first phase of our study) were compared with individuals infected in the second 6 months (and thus were positive for the first time in the second phase of our study), for the level of anti‐SARS‐CoV‐2 RBD antibodies, IgM, IgG, and IgA by ELISA using serial dilutions. (A) Comparison of the levels of antibodies (IgM, IgG, and IgA) between participants who were positive in September 2020 (n = 188, blue) and those who were positive in March 2021 (n = 194, white), showing apparent larger titers of IgM and IgG in people infected after September 2020. (B) Same as (A), but binning the participants by time since infection, with participants positive in September 2020 in grey (n = 166) and those positive in March 2021 in white (n = 178). Box and Whiskers plot show 10–90 percentile. This panel shows that there are no differences in antibody levels between the two cohorts and the differences in panel A) are due to different distributions in time since infections. P‐values for two‐sided Mann–Whitney tests.
We also analyzed the level of antibody in non‐vaccinated participants by gender at birth, age, BMI, and smoking status controlling for time since infection when known, using general linear models. We found no differences by gender or BMI. However, when controlling for time since infection, older people tended to have higher levels of antibodies (IgM, IgG, and IgA, P = 10–5, P = 0.006 and P = 0.022, respectively) than younger people, and non‐smokers also had higher levels of antibodies (IgG and IgA, P = 0.0078, P = 0.012, respectively) than smokers, even when we controlled for age group and gender (P = 0.021, P = 0.013, for IgG and IgA, respectively).
SARS‐CoV‐2 vaccination in Portugal started December 27, 2020. We quantified antibody titers in 161 people, who reported in their questionnaire that they had the first dose of the vaccine between 1 and 73 days prior to providing a blood sample. Of these 13 were in seropositive participants from the first phase. Vaccines are intramuscular and in accordance, we observe little RBD‐specific IgM, but robust induction of IgG after the first 2 weeks, which may outcompete other isotypes for RBD binding in an ELISA setup, and modest IgA (Fig. 4A). Importantly, within the group of confirmed seropositive after viral infection with SARS‐CoV‐2 from our first study as expected vaccination did not significantly increase RBD‐specific IgM levels, but significantly boosted IgG and IgA levels as shown by our current analyses (Fig. 4B).
Figure 4.
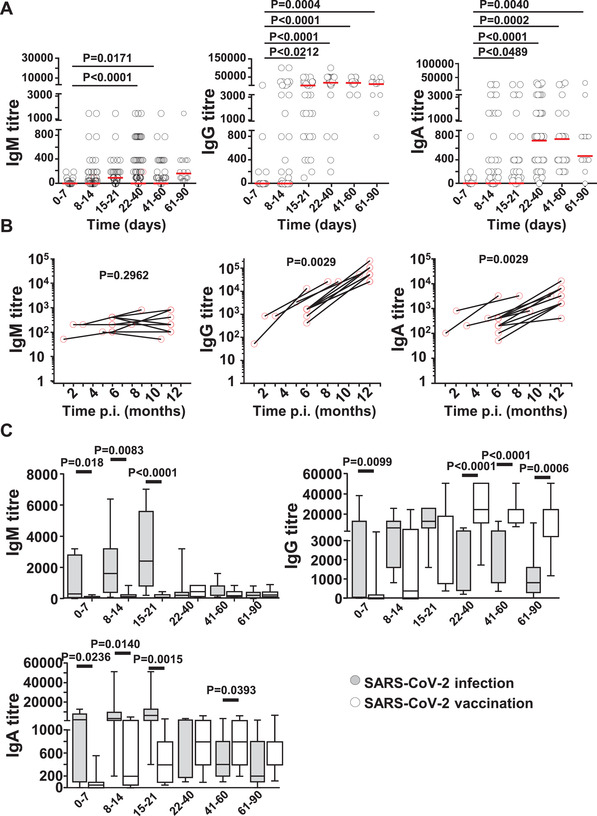
Antibody levels for participants after the first dose of SARS‐CoV‐2 vaccine. Serum samples from individuals vaccinated against SARS‐CoV‐2 were assessed for the level of anti‐SARS‐CoV‐2 RBD antibodies, IgM, IgG, and IgA by ELISA using serial dilutions. (A) Levels of IgM, IgG, and IgA (from left to right) for vaccinated participants (n = 148) grouped by time since the first vaccine dose. Note that, in most cases, a vaccine boost was given at 4 weeks, which can clearly be seen in the IgG titers. Red line indicates the geographic mean. (B) Antibody levels for the few participants who had been infected before receiving the vaccine (n = 13), clearly showing the boosting effect of a single dose of the vaccine in IgG and IgA. (C) Comparison of antibody titers after viral infection (grey, n = 287, includes data from [1]) or vaccine dose (1st dose 1–28 days, 2nd dose after 28 days) (white, n = 148) by time in days since that event (infection or vaccination). Box and Whiskers plot show 10–90 percentile. P‐values in (A) are for Kruskal‐Wallis test with Tukey correction for multiple comparisons; in (B) are for two‐sided Wilcoxon signed‐rank test for matched pairs; and in (C) are for two‐sided Mann‐Whitney tests at each time period.
Comparing antibody levels generated by a viral infection or the first dose of the vaccine (Fig. 4C), grouping people by time since infection or vaccination, showed high variability in the induced levels of antibodies, especially after viral infection; and that viral infection elicits stronger IgM, IgA, and IgG responses early on, but, at least for IgG, vaccine induced‐levels are higher from 3 weeks after dosing. These data underscore the potential of vaccines to maximize anti‐RBD IgG responses.
Discussion
We present the findings of a population‐based longitudinal study, conducted with a stratified quota sample of the Portuguese population, covering two distinct periods during the SARS‐CoV‐2 pandemic. Our first study was in September 2020, 6 months after a modest first SARS‐CoV‐2 wave in March to May 2020, and showed a low seroprevalence of 2.2%, approximately 226,000 people [15]. The current follow‐up study followed the second and third wave, the latter of which was very severe. Furthermore, the Portuguese national vaccination program started on December 27, 2020, albeit at a small scale due to limited supply in the beginning of 2021 and with priority given to healthcare staff and elderly care home residents (this latter group is not included in our study). Reflecting the high SARS‐CoV‐2 incidence in this period and the initial vaccination effort, over the first 12 months of the pandemic (until March 2021) we found a seroprevalence of 13.1% due to viral infection, corresponding to about 1,350,000 people. Considering that the number of official PCR‐confirmed cases reported at the beginning of September 2020 and in late February 2021 were ∼58,000 and ∼797,000, respectively [16]. The ratio between serological test and reported PCR positive cases reduced from approximately 3.9 to 1.7, reflecting the increased capacity for testing since the first wave hit Portugal [23]. Furthermore, allowing for a typical delay of three weeks from infection to death, the 16,684 deaths officially registered on March 14, 2021, suggest an overall infection fatality rate of 1.2%, at the top end of those reported in total populations using serology data (0.5%–1.2%) [15, 24–26], and increased from the 0.85% found in September 2020, reflecting the dire situation in Portugal during January 2021. When we also consider vaccinated people, the seroprevalence increased to 17.3% nationwide, approximately 1,782,000 people. This value is consistent with another (unpublished) study of seroprevalence in Portugal conducted between early February and late March, which found 15.5% seropositive people, including vaccinated [27].
We previously reported antibody kinetics during and shortly after acute SARS‐CoV‐2 infection [1]. These kinetics shows a characteristic rapid increase peaking at 3–4 weeks post‐infection followed by a subsequent contraction phase, but with the continued presence of SARS‐CoV‐2‐specific antibodies at least until months 6–7 post‐infection, and with rapid increases of the three isotypes assessed, similar as reported for the SARS and MERS responses [1, 28, 29]. An important question in SARS‐CoV‐2 immunology and also in the interpretation of serology studies, is how long seropositivity lasts. We made use of our established sensitive lab‐based ELISA, to quantify the antibody levels in 188 people, who were seropositive in the first phase of our longitudinal study, and who were re‐assessed in the current study. For many of these people, we know the date of diagnosis by PCR or the suspected date of infection by symptoms and epidemiological contact. We found an initial antibody waning for the isotypes IgM and IgG within the first four months after viral infection, with significantly reduced levels of SARS‐CoV‐2 RBD‐specific IgM and IgG levels in longitudinal testing. Of interest, IgA levels remained stable. After this initial decay, there is a plateau phase with those individuals first sampled five‐seven months after infection showing stable levels of anti‐SARS‐CoV‐2 RBD IgM, IgG, and IgA over time, with a trend indicating continued, but modest, antibody waning, maintaining detectable antibody levels up to 12 months after the initial infection in all sera tested. Indeed, it is remarkable that in all 188 people for whom we quantified titers in September 2020, and who represent a cross‐sectional sample of the Portuguese population, we could still detect antibodies (IgA, IgM, IgG) in March 2021. For these participants, we estimated very slow decays in antibody levels, with half‐lives of >2 years, which is substantially longer than previously reported [8]. This is likely explained by our finding that there seem to be two phases of decay, an initial contraction in antibody levels followed by a more stable plateau. The patients in the report by Dan et al. [8] were, in general, assayed earlier after infection than our participants. In fact, if we calculate the half‐life of patients identified earlier than 4 months post‐infection, it is much shorter at ∼300 days for both IgM and IgG, closer to those reported previously.
We also analyzed the effects of vaccination on antibody levels. For the most part, we confirmed expected results, with increasing levels of IgG and IgA detected after the first two‐ or 3‐weeks post‐vaccination, and a significant boost in antibody levels for those isotypes in people who had been infected before. It is important to note that even after just the first dose of vaccine (in Portugal at this time only the vaccines by AstraZeneca and Pfizer/BioNtech were approved) the levels of IgG generated are substantial and after 3 weeks tend to be even higher than viral infection, at a similar time. These results are important to inform models for most efficient vaccination strategies in the population [39].
Our study has some limitations. In the current study, we used a random sample from the participants in the original study [15], matching several characteristics to the Portuguese population for better representation. However, the 28% non‐participation rate (2173 of 3000 invitations), in line with the numbers of other population‐based studies [11, 24, 40], may introduce some bias in the sample, which is only partly ameliorated by our stratification strategy. Another issue is that we measured antibody titers, but not neutralization levels, which is arguably a better surrogate of immune protection [6, 10]. However, as a measure of past infection, how long antibodies last, and how to interpret serological studies, the levels of IgM, IgG, and IgA as assayed here are the gold standard. Moreover, antibody levels measured by ELISA and neutralization titres are typically well‐correlated [3]. It is also possible that some of the vaccinated people were infected before receiving the vaccine, and our assays does not distinguish between viral infection and vaccination. Thus, our estimate of viral infection could be slightly higher, however, this is mitigated by current guidelines in Portugal, which delay vaccination to previously infected people until a later phase of the campaign.
In spite of these limitations, our study is one of the few assessing seropositivity longitudinally in a large population‐wide National sample, allowing calculation of antibody waning. Most other recent National‐level studies with multiple serological assessment campaigns use a cross‐sectional, rather than a longitudinal design [27, 41‐43]. One recent study with a longitudinal design was conducted in the Faroe Islands [44], with results comparable to what we present here, especially in terms of two phases of decay and long duration of antibody positivity.
Serological studies rely on the maintenance of antibody levels to identify those who are immune and to quantify the extent of infection in populations. We found that antibody levels are measurable in the vast majority of people with times since infection spanning 3 to 12 months. This suggests good quality immunity is likely able to reduce illness severity upon reinfection and reduce future transmission in the population. In addition, it indicates the feasibility to retrospectively interrogate SARS‐CoV‐2 infection rates with help of serological studies at least a year into the pandemic.
Materials and methods
Study design, population, and sample size
We conducted an observational, follow‐up study to our previous non‐institutionalized population seroprevalence study from September 2020. From the participants in that study, we invited for the current study a random sample from among those who were seronegative – we call this the previously NC – and all the participants (n = 296) who tested positive for total antibodies against SARS‐CoV‐2 – we call this the previously PC. The global sample size was determined to allow no more than a 1.5% margin of error, at a 95% confidence level, for an expected prevalence of antibody positivity of 10%. With these assumptions, we estimated a sample of 2260 people, 2000 in the NC and 260 in the PC. To reach the desired sample size in the NC, we invited 3000 people from among those participants in our September study who were seronegative, which included over 13,000 people [15]. These 3000 people were selected randomly in strata by age group (<18, 18 to 54, ≥55 years) and by population density of the place of residence (≤500, >500 people/km2). In addition, using appropriate probabilities of inclusion in the sample, we ensured that the distributions by sex, household size, and level of formal education were consistent with those in the overall population of Portugal.
We used the PC cohort to analyze the evolution of the antibody levels in people who tested positive in the previous study.
Informed consent was obtained from all participants aged 16 years or older. In addition, parental or legal guardian consent was required for all participants below 18 years old. Participants were excluded if they had any contraindication for phlebotomy. Prior diagnosis of SARS‐CoV‐2 infection was not an exclusion criterion.
The study was conducted in compliance with data protection regulations in Portugal and was approved by the Ethics Committee of the Centro Académico de Medicina de Lisboa (CAML – the Lisbon Academic Medical Centre), under reference # 484/20 of February 23, 2021.
Serological tests and procedures
All blood collections and serological tests were done by Centro de Medicina Laboratorial Germano de Sousa (CMLGS), an ISO 9001:2015 certified private laboratory, which performs serological tests for SARS‐CoV‐2 according to the clinical guidelines issued by the Directorate‐General of Health (DGS), within the Portuguese Ministry of Health. CMLGS coordinated blood collection through their national network of collection sites, which allowed the participants to visit the center that was more convenient for them. Each participant donated 7–9 ml of blood collected into tubes with separation gel and without any anti‐coagulant, for a 4–5ml serum sample, obtained by centrifugation. All samples were transported to the central laboratory, according to usual procedures, where they were assayed.
Total antibodies, IgM plus IgG, against SARS‐CoV‐2 receptor‐binding domain (RBD) of the Spike protein were assessed using a chemiluminescent immunoassay test, Siemens® SARS‐CoV‐2 Total (COV2T) (Advia Centaur Siemens, Siemens Healthcare, Portugal) using the Atellica® IM Analyzer in a diagnostic lab setting and according to the manufacturer's instructions. Detailed information can be found at https://www.siemens‐healthineers.com/en‐us/laboratory‐diagnostics/assays‐by‐diseases‐conditions/infectious‐disease‐assays/cov2t‐assay. The overall sensitivity and specificity of this test are 98.1% and 99.9%, respectively, as estimated in a large study by independent researchers [45]. We used these values to correct the seroprevalence estimates with the Rogan‐Gladen estimator [46].
A majority of the samples that tested positive for total antibodies were sent to Biobanco‐iMM, Lisbon Academic Medical Centre, and stored at −80°C. Then they were further tested to quantify the level of antibodies using our in‐house developed protocol described in detail in [1, 47]. Briefly, flat‐bottom 96‐well plates (Microlon plates medium binding; Greiner) were coated with recombinant protein RBD or Spike prepared in PBS at a concentration of 2 μg/ml (50 μl/well). Plates were blocked with 200 μl/well of 3% non‐fat milk powder in PBS‐1%T for 1 hour at room temperature and then washed with PBS‐T 3×, 6×, or 10×, as described previously [1]. Serum samples were diluted in PBS‐0.1%T + 1% non‐fat milk powder, added (100 μl/well) and incubated for 1–2 h at room temperature, washed with PBS‐T 3×, 6× or 10×. Hereafter several antibody isotypes, namely IgG, IgM, and IgA antiSARS‐CoV2 were detected using HRP‐labelled goat anti‐human IgG Fc (Abcam, ab97225), IgM mu chain (Abcam, ab97205), IgA alpha chain (Abcam, ab97215), respectively. OD at 450nm was measured via SPARK (TECAN) plate reader. Each plate contained Quality control (QC) samples, composed of a pool of positive samples, tested in a high and low dilution.
To compare antibody titers after vaccination with those after viral infection, we included additional samples previously processed with identical method and reported in Figueiredo et al. [1]. These samples, from our previous study, were obtained shortly after infection and provide a better comparison with the vaccinated people, who we sampled in the current study shortly after vaccination.
Data collection and outcomes
All participants completed a questionnaire with socio‐demographic, general health, and clinical/epidemiological questions regarding SARS‐CoV‐2 exposure, including symptoms of interest, as well as COVID‐19 vaccination status. The full questionnaire was presented before [15].
The primary outcome was the proportion of serological positive cases in each of the twelve strata (six for each cohort), defined as the fraction of participants who tested positive for SARS‐CoV‐2 specific antibodies in the COV2T assay. With these fractions, we inferred the seroprevalence in the Portuguese population, adjusting for the weights of the strata and correcting for sensitivity and specificity of the tests. The secondary outcome included the proportion of previously positive people that remained positive, and the quantification of any decline in antibody levels.
Statistical analyses
We used sample weights to adjust the seroprevalence extrapolating from our strata (age groups and population density of the place of residence) to the whole population. In addition, we combined the results of seroprevalence in the two cohorts NC and PC, with appropriate weights for each, based on the results of the previous study [15], to obtain the overall estimation of seroprevalence in Portugal. We performed these calculations in two ways, excluding or including the people, who indicated that they had been vaccinated before the study.
The prevalence was calculated as weighted proportion and to calculate confidence intervals, we used the methodology described in [48], i.e., we used the exact limiting terms for the binomial parameter adapted for weighted proportions and combined stratum specific confidence intervals with the use of the adequate rescaling factor as proposed in [48].
We compared continuous variables (such as antibody titers) using non‐parametric tests (Wilcoxon sign‐rank test for paired design, Mann‐Whitney for unpaired designs, and Kruskal‐Wallis to compare more than two groups, with Tukey correction for multiple comparisons). To analyze antibody levels with time since infection (or vaccination), we used the dates of known PCR positive test or COVID‐19 symptoms, when known from the participants questionnaire. We then calculated the decay of (log) antibody titers over time using linear‐mixed effects models, where participant was the random factor. The half‐life of antibodies is then given by log(1/2)/slope of decay. We used general linear models to control for time since infection, when studying differences of antibody levels by gender, age, body mass index (BMI), and smoking status. We did not input any missing values. All statistical analyses were two‐sided, the significance level was α = 0.05, and reported confidence intervals are at the 95% level. Statistical analyses were done using R (version 3.6.1, R Foundation for Statistical Computing, Vienna, Austria) and GraphPad Prism 6.01 (GraphPad Software, San Diego, California USA).
Ethics statement
The study was conducted in compliance with data protection regulations in Portugal and was approved by the Ethics Committee of the Centro Académico de Medicina de Lisboa (CAML – the Lisbon Academic Medical Centre), under reference # 484/20 of 23rd of February 2021.
Conflict of interest
The authors declare no conflict of interest.
Peer review
The peer review history for this article is available at https://publons.com/publon/10.1002/eji.202149619
Abbreviations
- CMLGS
Centro de Medicina Laboratorial Germano de Sousa
- NC
negative cohort
- PC
positive cohort
- PHEIC
Public Health Emergency of International Concern
- RBD
receptor‐binding domain
Acknowledgments
The authors would like to thank all volunteers who helped with blood collections and donors for providing blood samples and cooperation to make this study possible. Serum samples were requested from Biobanco‐IMM, Lisbon Academic Medical Centre, Lisbon, Portugal. The authors would like to acknowledge funding from Sociedade Francisco Manuel dos Santos and Grupo Jerónimo Martins; the European Union Horizon 2020 research and innovation program (ERA project No 667824 – EXCELLtoINNOV, and ERA project No 952377 – iSTARS); Fundação para a Ciência e a Tecnologia (FCT, Portugal) through research4COVID19 (n° 231_596873172, and n° 729) UID/MAT/00006/2019 and PTDC/MAT‐APL/31602/2017, with additional support from the LANL LDRD program grant 20210730 ER. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors acknowledge the generous sharing of the expression constructs by Dr Florian Krammer, Icahn School of Medicine at Mount Sinai, New York, USA (Development of SARS‐CoV‐2 reagents was partially supported by the NIAID Centers of Excellence for Influenza Research and Surveillance (CEIRS) contract HHSN272201400008C), and the protein production by Drs Paula Alves and Rute Castro at Instituto de Biologia Experimental e Tecnológica (iBET) Oeiras, Portugal as part of the Serology4COVID consortium.
Contributor Information
Luísa Canto e Castro, Email: ldloura@fc.ul.pt.
Marc Veldhoen, Email: marc.veldhoen@medicina.ulisboa.pt.
Ruy M. Ribeiro, Email: ruy@lanl.gov.
Data availability statement
All data will be made available preserving anonymity upon reasonable request.
References
- 1. Figueiredo‐Campos, P. , Blankenhaus, B. , Mota, C. , Gomes, A. , Serrano, M. , Ariotti, S. , Costa, C. et al., Seroprevalence of anti‐SARS‐CoV‐2 antibodies in COVID‐19 patients and healthy volunteers up to 6 months post disease onset. Eur. J. Immunol. 2020. 50: 2025–2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grifoni, A. , Weiskopf, D. , Ramirez, S. I. , Mateus, J. , Dan, J. M. , Moderbacher, C. R. , Rawlings, S. A. et al., Targets of T cell responses to SARS‐CoV‐2 coronavirus in humans with COVID‐19 disease and unexposed individuals. Cell 2020. 181: 1489–1501 e1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Iyer, A. S. , Jones, F. K. , Nodoushani, A. , Kelly, M. , Becker, M. , Slater, D. , Mills, R. et al., Persistence and decay of human antibody responses to the receptor binding domain of SARS‐CoV‐2 spike protein in COVID‐19 patients. Sci. Immunol. 2020. 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Le Bert, N. , Tan, A. T. , Kunasegaran, K. , Tham, C. Y. L. , Hafezi, M. , Chia, A. , Chng, M. H. Y. et al., SARS‐CoV‐2‐specific T cell immunity in cases of COVID‐19 and SARS, and uninfected controls. Nature 2020. 584: 457–462. [DOI] [PubMed] [Google Scholar]
- 5. Ripperger, T. J. , Uhrlaub, J. L. , Watanabe, M. , Wong, R. , Castaneda, Y. , Pizzato, H. A. , Thompson, M. R. et al., Orthogonal SARS‐CoV‐2 serological assays enable surveillance of low‐prevalence communities and reveal durable humoral immunity. Immunity 2020. 53: 925–933 e924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wajnberg, A. , Amanat, F. , Firpo, A. , Altman, D. R. , Bailey, M. J. , Mansour, M. , McMahon, M. et al., Robust neutralizing antibodies to SARS‐CoV‐2 infection persist for months. Science 2020. 370: 1227–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Choe, P. G. , Kim, K. H. , Kang, C. K. , Suh, H. J. , Kang, E. , Lee, S. Y. , Kim, N. J. et al., Antibody responses 8 months after asymptomatic or mild SARS‐CoV‐2 infection. Emerg. Infect. Dis. 2021. 27: 928–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dan, J. M. , Mateus, J. , Kato, Y. , Hastie, K. M. , Yu, E. D. , Faliti, C. E. , Grifoni, A. et al., Immunological memory to SARS‐CoV‐2 assessed for up to 8 months after infection. Science 2021. 371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hartley, G. E. , Edwards, E. S. J. , Aui, P. M. , Varese, N. , Stojanovic, S. , McMahon, J. , Peleg, A. Y. et al., Rapid generation of durable B cell memory to SARS‐CoV‐2 spike and nucleocapsid proteins in COVID‐19 and convalescence. Sci. Immunol. 2020. 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Khoury, D. S. , Cromer, D. , Reynaldi, A. , Schlub, T. E. , Wheatley, A. K. , Juno, J. A. , Subbarao, K. et al., Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS‐CoV‐2 infection. Nat. Med. 2021. [DOI] [PubMed] [Google Scholar]
- 11. Pollan, M. , Perez‐Gomez, B. , Pastor‐Barriuso, R. , Oteo, J. , Hernan, M. A. , Perez‐Olmeda, M. , Sanmartin, J. L. et al., Prevalence of SARS‐CoV‐2 in Spain (ENE‐COVID): a nationwide, population‐based seroepidemiological study. Lancet 2020. 396: 535–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rostami, A. , Sepidarkish, M. , Leeflang, M. M. G. , Riahi, S. M. , Nourollahpour Shiadeh, M. , Esfandyari, S. , Mokdad, A. H. et al., SARS‐CoV‐2 seroprevalence worldwide: a systematic review and meta‐analysis. Clin. Microbiol. Infect. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stringhini, S. , Wisniak, A. , Piumatti, G. , Azman, A. S. , Lauer, S. A. , Baysson, H. , De Ridder, D. , et al., Seroprevalence of anti‐SARS‐CoV‐2 IgG antibodies in Geneva, Switzerland (SEROCoV‐POP): a population‐based study. Lancet 2020. 396: 313–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhang, Z. , Bi, Q. , Fang, S. , Wei, L. , Wang, X. , He, J. , Wu, Y. et al., Insight into the practical performance of RT‐PCR testing for SARS‐CoV‐2 using serological data: a cohort study. Lancet Microbe. 2021. 2: e79‐e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Canto e Castro, L. , Pereira, A. H. G. , Ribeiro, R. , Alves, C. , Veloso, L. , Vicente, V. , Alves, D. et al., Prevalence of SARS‐CoV‐2 antibodies after the first 6 months of COVID‐19 pandemic, Portugal. Emerg. Infect. Dis. 2021. Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Relatório de Situação ‐ COVID‐19 . Direcao Geral de Saude.
- 17. Choe, P. G. , Kang, C. K. , Suh, H. J. , Jung, J. , Song, K. H. , Bang, J. H. , Kim, E. S. et al., Waning antibody responses in asymptomatic and symptomatic SARS‐CoV‐2 infection. Emerg. Infect. Dis. 2021. 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shioda, K. , Lau, M. S. , Kraay, A. N. , Nelson, K. N. , Siegler, A. J. , Sullivan, P. S. , Collins, M. H. et al., Estimating the cumulative incidence of SARS‐CoV‐2 infection and the infection fatality ratio in light of waning antibodies. Epidemiology 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bar‐On, Y. M. , Flamholz, A. , Phillips, R. and Milo, R. , SARS‐CoV‐2 (COVID‐19) by the numbers. Elife 2020. 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Long, Q. X. , Liu, B. Z. , Deng, H. J. , Wu, G. C. , Deng, K. , Chen, Y. K. , Liao, P. et al., Antibody responses to SARS‐CoV‐2 in patients with COVID‐19. Nat. Med. 2020. 26: 845–848. [DOI] [PubMed] [Google Scholar]
- 21. Lou, B. , Li, T. D. , Zheng, S. F. , Su, Y. Y. , Li, Z. Y. , Liu, W. , Yu, F. et al., Serology characteristics of SARS‐CoV‐2 infection after exposure and post‐symptom onset. Eur. Respir. J. 2020. 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Relatório de Vacinação ‐ COVID‐19 . Direcao Geral de Saude.
- 23. Veldhoen, M. and Zuzarte‐Luis, V. , Academic labs supporting COVID‐19 diagnostics. Eur. J. Immunol. 2021. 51: 13–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hallal, P. C. , Hartwig, F. P. , Horta, B. L. , Silveira, M. F. , Struchiner, C. J. , Vidaletti, L. P. , Neumann, N. A. et al., SARS‐CoV‐2 antibody prevalence in Brazil: results from two successive nationwide serological household surveys. Lancet Glob Health 2020. 8: e1390‐e1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ioannidis, J. P. A. , Infection fatality rate of COVID‐19 inferred from seroprevalence data. Bull. World Health Organ. 2021. 99: 19–33F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pastor‐Barriuso, R. , Perez‐Gomez, B. , Hernan, M. A. , Perez‐Olmeda, M. , Yotti, R. , Oteo‐Iglesias, J. , Sanmartin, J. L. , Infection fatality risk for SARS‐CoV‐2 in community dwelling population of Spain: nationwide seroepidemiological study. BMJ 2020. 371: m4509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Equipa ISN COVID‐19 , Inquérito Serológico Nacional COVID‐19 (2ª fase): relatório de apresentação dos resultados. Instituto Nacional de Saúde Doutor Ricardo Jorge, IP; 2021. [Google Scholar]
- 28. Corman, V. M. , Albarrak, A. M. , Omrani, A. S. , Albarrak, M. M. , Farah, M. E. , Almasri, M. , Muth, D. et al., Viral shedding and antibody response in 37 patients with middle east respiratory syndrome coronavirus infection. Clin. Infect. Dis. 2016. 62: 477–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hsueh, P. R. , Huang, L. M. , Chen, P. J. , Kao, C. L. and Yang, P. C. , Chronological evolution of IgM, IgA, IgG and neutralisation antibodies after infection with SARS‐associated coronavirus. Clin. Microbiol. Infect. 2004. 10: 1062–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bradburne, A. F. , Bynoe, M. L. and Tyrrell, D. A. , Effects of a “new” human respiratory virus in volunteers. Br. Med. J. 1967. 3: 767–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Callow, K. A. , Effect of specific humoral immunity and some non‐specific factors on resistance of volunteers to respiratory coronavirus infection. J. Hyg. (Lond) 1985. 95: 173–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Callow, K. A. , Parry, H. F. , Sergeant, M. and Tyrrell, D. A. , The time course of the immune response to experimental coronavirus infection of man. Epidemiol. Infect. 1990. 105: 435–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Reed, S. E. , The behaviour of recent isolates of human respiratory coronavirus in vitro and in volunteers: evidence of heterogeneity among 229E‐related strains. J. Med. Virol. 1984. 13: 179–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Liu, L. , Xie, J. , Sun, J. , Han, Y. , Zhang, C. , Fan, H. , Liu, Z. et al., Longitudinal profiles of immunoglobulin G antibodies against severe acute respiratory syndrome coronavirus components and neutralizing activities in recovered patients. Scand. J. Infect. Dis. 2011. 43: 515–521. [DOI] [PubMed] [Google Scholar]
- 35. Liu, W. , Fontanet, A. , Zhang, P. H. , Zhan, L. , Xin, Z. T. , Baril, L. , Tang, F. et al., Two‐year prospective study of the humoral immune response of patients with severe acute respiratory syndrome. J. Infect. Dis. 2006. 193: 792–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Liu, W. J. , Zhao, M. , Liu, K. , Xu, K. , Wong, G. , Tan, W. and Gao, G. F. , T‐cell immunity of SARS‐CoV: Implications for vaccine development against MERS‐CoV. Antiviral Res. 2017. 137: 82–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Choe, P. G. , Perera, R. , Park, W. B. , Song, K. H. , Bang, J. H. , Kim, E. S. , Kim, H. B. et al., MERS‐CoV antibody responses 1 year after symptom onset, South Korea, 2015. Emerg. Infect. Dis. 2017. 23: 1079–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Veldhoen, M. and Simas, J. P. , Endemic SARS‐CoV‐2 will maintain post‐pandemic immunity. Nat. Rev. Immunol. 2021. 21: 131–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Viana, J. , van Dorp, C. H. , Nunes, A. , Gomes, M. C. , van Boven, M. , Kretzschmar, M. E. , Veldhoen, M. et al., Controlling the pandemic during the SARS‐CoV‐2 vaccination rollout: a modeling study. Nat. Commun. 2021. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Petersen, M. S. , Strom, M. , Christiansen, D. H. , Fjallsbak, J. P. , Eliasen, E. H. , Johansen, M. , Veyhe, A. S. et al., Seroprevalence of SARS‐CoV‐2‐specific antibodies, faroe Islands. Emerg. Infect. Dis. 2020. 26: 2761–2763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Espenhain, L. , Tribler, S. , Jørgensen, C. S. , Hansen, C. H. , Sönksen, U. W. and Ethelberg, S. , Prevalence of SARS‐CoV‐2 antibodies in Denmark 2020: results from nationwide, population‐based sero‐epidemiological surveys. Medrxiv 2021. [Google Scholar]
- 42. University of Tartu , Study on the prevalence of the coronavirus in Estonia 2021.
- 43. Ward, H. , Cooke, G. , Whitaker, M. , Redd, R. , Eales, O. , Brown, J. C. , Collet, K. et al., REACT‐2 Round 5: increasing prevalence of SARS‐CoV‐2 antibodies demonstrate impact of the second wave and of vaccine roll‐out in England. MedRxiv 2021. [Google Scholar]
- 44. Petersen, M. S. , Hansen, C. B. , Kristiansen, M. F. , Fjallsbak, J. P. , Larsen, S. , Hansen, J. L. , Jarlhelt, I. , SARS‐CoV‐2 natural antibody response persists for at least 12 months in a nationwide study from the faroe Islands. Open Forum Infect. Dis. 2021. 8: ofab378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. National SARS‐CoV‐Serology Assay Evaluation Group , Performance characteristics of five immunoassays for SARS‐CoV‐2: a head‐to‐head benchmark comparison. Lancet Infect. Dis. 2020. 20: 1390–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rogan, W. J. and Gladen, B. , Estimating prevalence from the results of a screening test. Am. J. Epidemiol. 1978. 107: 71–76. [DOI] [PubMed] [Google Scholar]
- 47. Stadlbauer, D. , Amanat, F. , Chromikova, V. , Jiang, K. , Strohmeier, S. , Arunkumar, G. A. , Tan, J. et al., SARS‐CoV‐2 seroconversion in humans: a detailed protocol for a serological assay, antigen production, and test setup. Curr. Protoc. Microbiol. 2020. 57: e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Waller, J. L. , Addy, C. L. , Jackson, K. L. and Garrison, C. Z. , Confidence intervals for weighted proportions. Stat. Med. 1994. 13: 1071–1082. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data will be made available preserving anonymity upon reasonable request.


