Abstract
Firefighters are occupationally exposed to products of combustion containing polycyclic aromatic hydrocarbons (PAHs) and flame retardants (FRs), potentially contributing to their increased risk for certain cancers. Personal protective equipment (PPE), including firefighter hoods, helps to reduce firefighters’ exposure to toxic substances during fire responses by providing a layer of material on which contaminants deposit prior to reaching the firefighters skin. However, over time hoods that retain some contamination may actually contribute to firefighters’ systemic dose. We investigated the effectiveness of laundering to reduce or remove contamination on the hoods, specifically PAHs and three classes of FRs: polybrominated diphenyl ethers (PBDEs), non-PBDE flame retardants (NPBFRs), and organophosphate flame retardants (OPFRs). Participants in the study were grouped into crews of 12 firefighters who worked in pairs by job assignment while responding to controlled fires in a single family residential structure. For each pair of firefighters, one hood was laundered after every scenario, and one was not. Bulk samples of the routinely laundered and unlaundered hoods from five pairs of firefighters were collected and analyzed. Residual levels of OPFRs, NPBFRs, and PAHs were lower in the routinely laundered hoods, with total levels of each class of chemicals being 56–81% lower, on average, than the unlaundered hoods. PBDEs, on average, were 43% higher in the laundered hoods, most likely from cross contamination. After this initial testing, four of the five unlaundered exposed hoods were subsequently laundered with other heavily exposed (unlaundered) and unexposed (new) hoods. Post-laundering evaluation of these hoods revealed increased levels of PBDEs, NPBFRs, and OPFRs in both previously exposed and unexposed hoods, indicating cross contamination. For PAHs, there was little evidence of cross contamination and the exposed hoods were significantly less contaminated after laundering (76% reduction; P = 0.011). Further research is needed to understand how residual contamination on hoods could contribute to firefighters’ systemic exposures.
Keywords: Firefighters, flame retardants, hoods, laundering, PAHs, PBDEs
INTRODUCTION
Firefighters’ occupational exposure to toxic substances is a topic of growing concern, as several recent studies have highlighted firefighters’ increased risk for certain cancers.(1–2) Firefighters’ exposure to polycyclic aromatic hydrocarbons (PAHs) are a primary concern, as some PAHs are known carcinogens and are released during incomplete combustion.(3) Exposure to flame retardants (FRs) has also become an increasing concern for firefighters,(4) especially during structural fire responses where FRs present in furnishings may be released into the air through combustion. Studies have found PAHs, FRs, phthalates, and other chemicals contaminating personal protective equipment (PPE).(3, 5–7, 10). These contaminants could be transferred to skin and then subsequently absorbed, inhaled, or inadvertently ingested. When PPE is doffed, often after self-contained breathing apparatus (SCBA) removal, dry contaminants can become airborne and inhaled. These studies also highlight the potential for take-home exposure. For example, it has been found that fire station dust had higher FR levels (e.g., decabromodiphenyl ether (BDE-209)) than other occupational settings. This could potentially come from contamination carried back from the fire environment (e.g., contaminated clothing or equipment).(8)
Protective hoods, characterized by NFPA as the interface element of the protective ensemble that provided limited protection to the coat/helmet/SCBA face-piece interface area(9), are worn by firefighters during responses. Protective hoods come in direct contact with neck and face skin, areas identified for significant dermal exposure to products of combustion.(11) Traditionally, hoods may be worn for multiple responses without laundering.
PAHs are common environmental pollutants present in fire smoke and have been associated with certain types of cancer.(10) In a study by Fent et al., PAH metabolites were identified in firefighters’ urine post firefighting even though SCBA were used, suggesting that dermal adsorption, potentially through contaminated PPE, may contribute to firefighters’ systemic levels.(3) Exposure to FRs and PAHs is also thought to be largely dependent on the job assignment or task completed by firefighters. We have reported that firefighters assigned to fire attack or search and rescue tasks inside the burning structure had the highest levels of contamination on their turnout coat compared to other fireground job assignments.(11)
There are a few distinct classes of FRs to which firefighters’ are potentially exposed. Polybrominated diphenyl ethers (PBDEs) are FRs that were used in a variety of consumer products (e.g. electronics, foam furniture and padding) starting in the 1970s.(5, 12–13) Due to human and environmental health concerns, PBDEs of the penta- and octa- BDE technical formulations were added in May 2009 to the Persistent Organic Pollutants (POPs) list of the Stockholm Convention, restricting their usage globally in signatory countries. Deca-formulation was added to this list in 2017.(14) PBDE production within the U.S. ended in 2013, but PBDEs will continue to be released into the environment from products with long usage lifetimes such as furniture and automobiles. PBDEs are persistent, accumulate in the body, and have been associated with altered hormone regulation and possible neurobehavioral effects.(15–16) Manufacturers have replaced PBDEs primarily with two groups of FRs: organophosphate flame retardants (OPFRs) and non-PBDE flame retardants (NPBFRs) which includes novel FRs.(5, 17) The physiological effects of many replacements to PBDEs are still relatively unknown. Dishaw et al. (13) found that OPFRs may affect neurodevelopment to a further extent than PBDEs, while another study found an association between OPFRs and cytotoxicity.(18) Additionally, NPBFRs 2-ethylhexyl-2,3,4,5-tetrabromobenzoate (TBB) and bis (2-ethylhexyl)-2,3,4,5-tetrabromophtalate (TBPH) were observed to be endocrine disruptors.(19) In a study conducted by Shaw et al.,(20) firefighters’ blood samples were found to have elevated levels of PBDE flame retardants (relative to the US population) within 24 hours of responding to a fire. Another recent study reported higher levels of OPFRs in firefighters’ urine than the general population.(21)
While we do not currently know the extent to which contaminated PPE may contribute to firefighters’ systemic dose, laundering firefighter gear may be an effective way to reduce firefighters’ overall exposure to PAHs and FRs. However, we are not aware of any studies that have investigated the effectiveness of laundering at removing such contamination from firefighting PPE. This study sought to estimate the effectiveness of laundering firefighter hoods in removing PAHs and three separate classes of flame retardants: PBDEs, OPFRs, and NPBFRs. Our hypothesis was that laundering would reduce FR and PAH contamination to pre-firefighting background or non-detectable levels.
METHODS
Study Design
Hood Contamination: Routinely Laundered vs. Unlaundered
This hood evaluation study was part of a larger project focused on chemical exposures and cardiovascular effects in 40 firefighters responding to controlled room and contents fires using typical early 21st century furnishings.(22)
In this study, crews of 12 firefighters responded to live fire scenarios in a fully-furnished structure simulating a one-story residential building, where fires were set in two of the four bedrooms. Furnishings in the fire rooms included a stuffed chair, mattress and foam topper, flat screen television, curtains, cushioned headboard, carpet and padding and were identical for each of the scenarios. Furnishings ranged in age and contained a variety of FRs (including some phased-out PBDEs) added by manufacturers; levels are reported elsewhere.(23)
Firefighters were assigned in pairs to jobs that included either fire attack, search and rescue, outside vent, command/pump operations, or two teams conducted overhaul operations. The attack team pulled a primary suppression line from the engine and entered the structure to extinguish all active fire. The search team entered the structure to search for and rescue two simulated occupants (75 kg manikins). The outside vent team deployed ladders to the structure and used hand tools to create openings at the windows and roof. The overhaul teams conducted low intensity operations outside of the structure during the firefight, then transitioned inside the building to perform overhaul operations such as removing drywall from the walls/ceiling and furniture from room to locate any hidden fire.(22) Command/pump teams established incident command and operated the pump panel outside of the structure.
Firefighters responded to two scenarios (only difference being two separate fire attack tactics), then were reassigned to a different job assignment and performed an additional two scenarios. Firefighters wore NFPA-1971(9) compliant personal protective ensembles, including double-layer Majestic Pac II Nomex® hoods. Ten of the 12 firefighters and their respective hoods were included in this study. In selecting the hoods for analysis, we first identified five pairs of firefighters with the same or similar job assignments, where one firefighter’s hood had been laundered after every scenario (routinely laundered), and the other firefighter’s hood had not been laundered. All of the laundered hoods in this study were laundered in a single load by following the manufacturer’s machine wash cleaning instructions and dried in open air after each scenario. In each case, a front load washing machine without an agitator was utilized with a 55 min wash/rinse cycle. Commercial ARM & HAMMER™ Plus OxiClean™ was used for the detergent. In total, routinely laundered hoods were cleaned four times, once after each scenario completed in a single load for each crew.
In selecting hoods for this analysis, we selected hoods from firefighters who had participated in either fire attack or search and rescue because firefighters in these job assignments had the highest exposures to smoke.(10) Job assignments for the other two scenarios were either overhaul or outside ventilation.
After all four scenarios had been completed (and laundering/drying performed where applicable), the hoods were placed into sealed plastic bags and shipped to the NIOSH laboratory. Three unused new hoods were also sent to the NIOSH laboratory to provide a baseline control (a previous study found FRs, specifically PBDEs, in unused hoods).(7)
Hood Contamination: Before and After Single Wash
On the basis of our preliminary results which indicated the potential of hood cross contamination during laundering, we added a post-hoc test that included previously laundered and unlaundered (i.e. new hoods). These were tested before and after a single laundering cycle. Samples were collected from the aforementioned five unlaundered hoods from the fireground study. Four of the five unlaundered hoods were then subsequently laundered (using the same conditions as before) together with the following set of hoods:
Two brand new, unexposed, unlaundered hoods. These hoods were included to evaluate whether clean hoods could become contaminated during laundering.
Two unexposed hoods that had been previously laundered 3 times by themselves. These hoods were included to assess whether the softening of the Nomex fabric from repeated laundering had any effect on the amount of cross-contamination retained by the hoods.
Four exposed, unlaundered hoods from a previous fire-attack study conducted by Underwriters Laboratories (UL). The hoods were switched out halfway through the study so each hood had approximately 12 fires of exposure.(24) These soiled hoods were included because they were used by firefighters in room and contents fires with identical furniture used in this study and, as such, were known to be highly contaminated with PAHs and FRs. Testing (using the methods described below) indicated total PBDE contamination ranging from 672 to 12,200 ng/g, NPBFR contamination ranging from 1360 to 4860 ng/g, and OPFR contamination ranging from 2650 to 5130 ng/g (Figure 2). These hoods were not tested for PAHs, but were assumed to contain heavy PAH contamination as well.
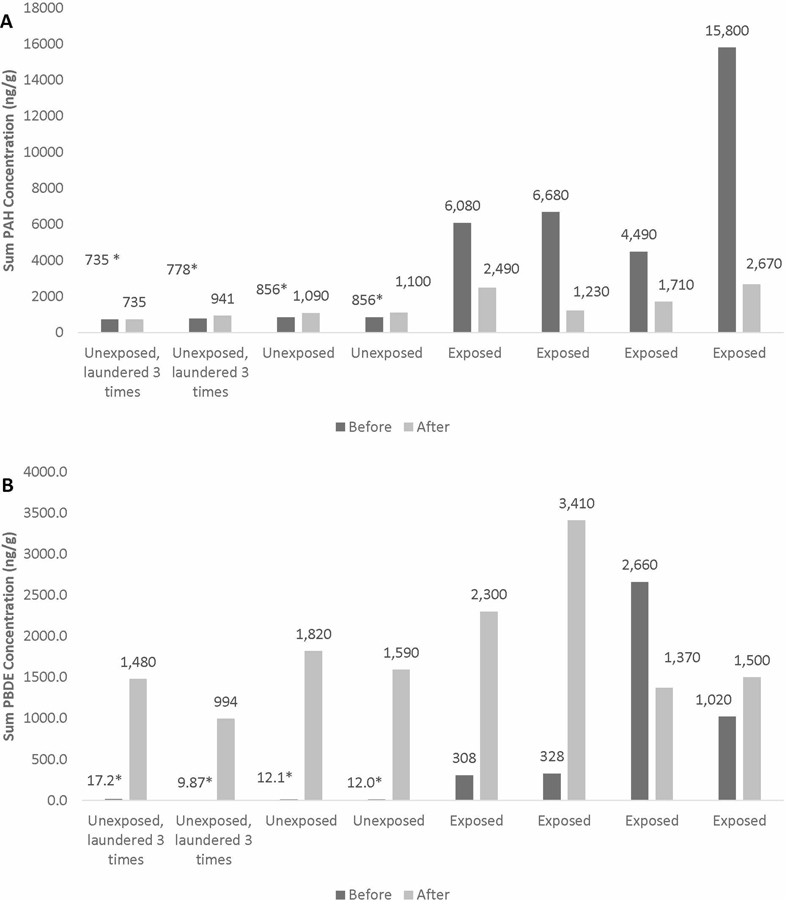
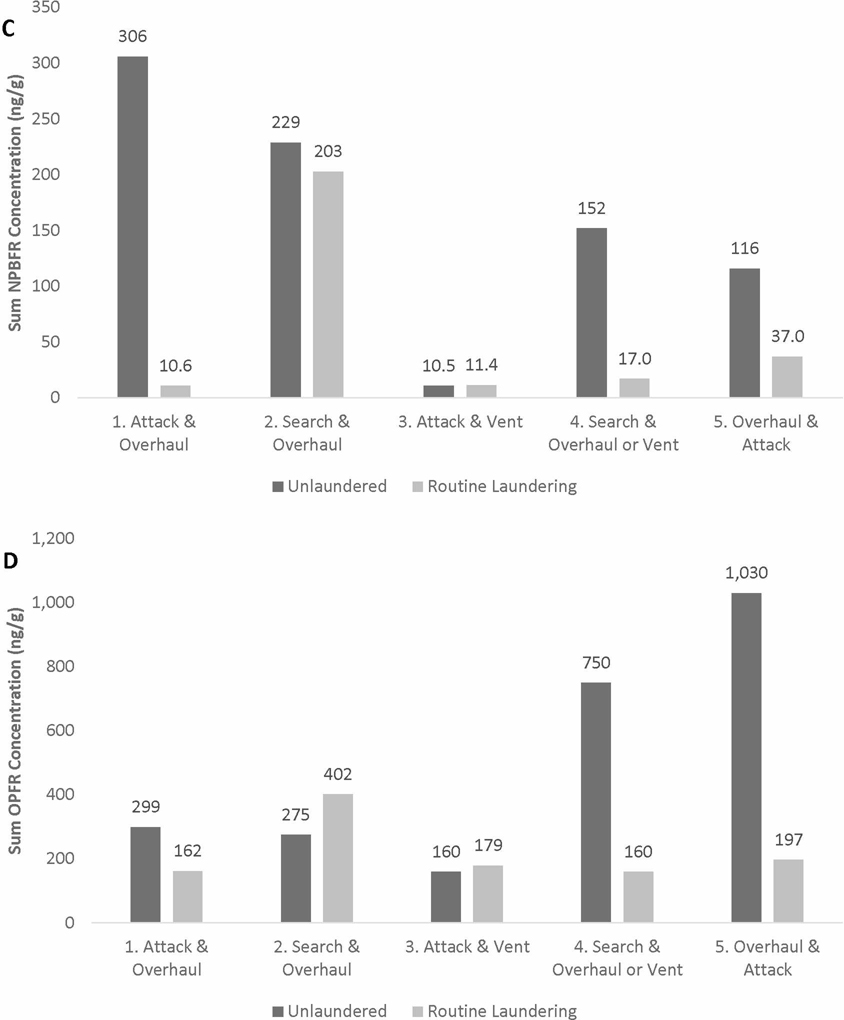
Figure 2.
Total levels of (A) PAHs, (B) PBDEs, (C) NPBFRs, (D) OPFRs in exposed and unexposed hoods before and after single laundering. Exposed, unlaundered hoods (n=4), new, unexposed hoods (n=2), unexposed hoods previously laundered 3 times (n=2), and additional soiled hoods (n=4) were laundered together in one washer to assess for cross contamination. Samples from exposed unlaundered hoods from UL were not taken after laundering as they were only included to provide additional contamination. Total PBDEs ranged from 672–12,200 ng/g, NPBFRs ranged from 1,360 to 4,860 ng/g, and OPFRs ranged from 2,650 to 5,130 ng/g in additional soiled hoods. Before measurements for all PBDEs, NPBFRs, and OPFRs on all unexposed hoods (n=4) were non-detect. Before measurements for all PAHs on unexposed hoods (n=4) were not collected and were assumed to be non-detect based on prior testing. For all non-detect results, values were assigned by taking LOD for each analyte and dividing by square root of 2. The non-detect results are identified with an asterisk (*).
This experiment provided an integrated test of both the cleaning efficiency and cross contamination under a realistic scenario (i.e, laundering multiple hoods containing various levels of contamination together in a single wash).
Hood Analysis
NIOSH investigators cut two side-by-side 100 cm2 square pieces of fabric from each hood, placed the samples into new sealed plastic bags, and shipped them to the analytical laboratory. Investigators changed nitrile gloves and cleaned the scissors with isopropanol after handling each hood. For the initial testing, sample locations were chosen based on the section of the unlaundered hood with the most visible contamination; the same general location was then selected for the paired laundered hood. Similar sample locations were selected for the post-hoc testing.
One fabric sample from each hood was analyzed for 15 PAHs using NIOSH Method 5506 (modified for bulk material analysis).(25) The other fabric sample was analyzed using ultra-performance liquid chromatography (UPLC) - atmospheric pressure photoionization (APPI) tandem mass spectrometry as previously described by La Guardia et al. (26) for the following compounds:
Polybrominated diphenyl ethers (PBDEs): 2,2’,4,4’-tetra-bromodiphenyl ether (BDE) (BDE-47), 2,2’,3,4,4’,-penta-BDE (BDE-85), 2,2’,4,4’,5-penta-BDE (BDE-99), 2,2’,4,4’,6-penta-BDE (BDE-100), 2,2’,4,4’,5,5’-hexa-BDE (BDE-153), 2,2’,4,4’,5,6’-hexa-BDE (BDE-154), 2,2’,3,4,4’,5,6-hepta-BDE (BDE-183), and deca-BDE (BDE-209)
Non-PBDE flame retardants (NPBFRs): 1,2-bis (2,4,6-tribromophenoxy) ethane (BTBPE), decabromodiphenylethane (DBDPE), 2-ethylhexyl 2,3,4,5-tetrabromobenzoate (TBB), di (2-ethylhexyl)-2,3,4,5-tetrabromophthalate (TBPH), hexabromocyclododecane (α-, β-, γ-HBCD), and tetrabromobisphenol-A (TBBPA)
Organophosphate flame retardants (OPFRs): tris (2-chloroethyl) phosphate (TCEP), tris (1-chloro-2-propyl) phosphate (TCPP) and tris (1,3-dichloro-2-propyl) phosphate (TDCPP)) and non-halogenated organophosphate flame retardants (non-HOPFRs): tricresyl phosphate (TCP) and triphenyl phosphate (TPP)
Data Analysis
In determining sum totals and summary statistics, non-detectable results for individual FRs and PAHs were assigned values by dividing the respective detection limits by square root of two. Contamination measured in unlaundered hoods were compared to routinely laundered hoods by paired job assignment, and then again after a single laundering. Contamination levels in unexposed (new) hoods before and after a single laundering were also compared. Descriptive statistics and paired t-tests comparing hoods before and after laundering were carried out using SAS (Version 9.4, SAS Institute, Inc., Cary, NC).
RESULTS
The results for the brand new hoods were non-detectable for all PAHs and FRs. For comparison, we also examined microscopic images of an unused hood, a 4-times laundered hood, and an unlaundered hood. There was a lack of microscopic visual evidence of change in fiber density after laundering (supplemental materials).
PAH Contamination on Hoods
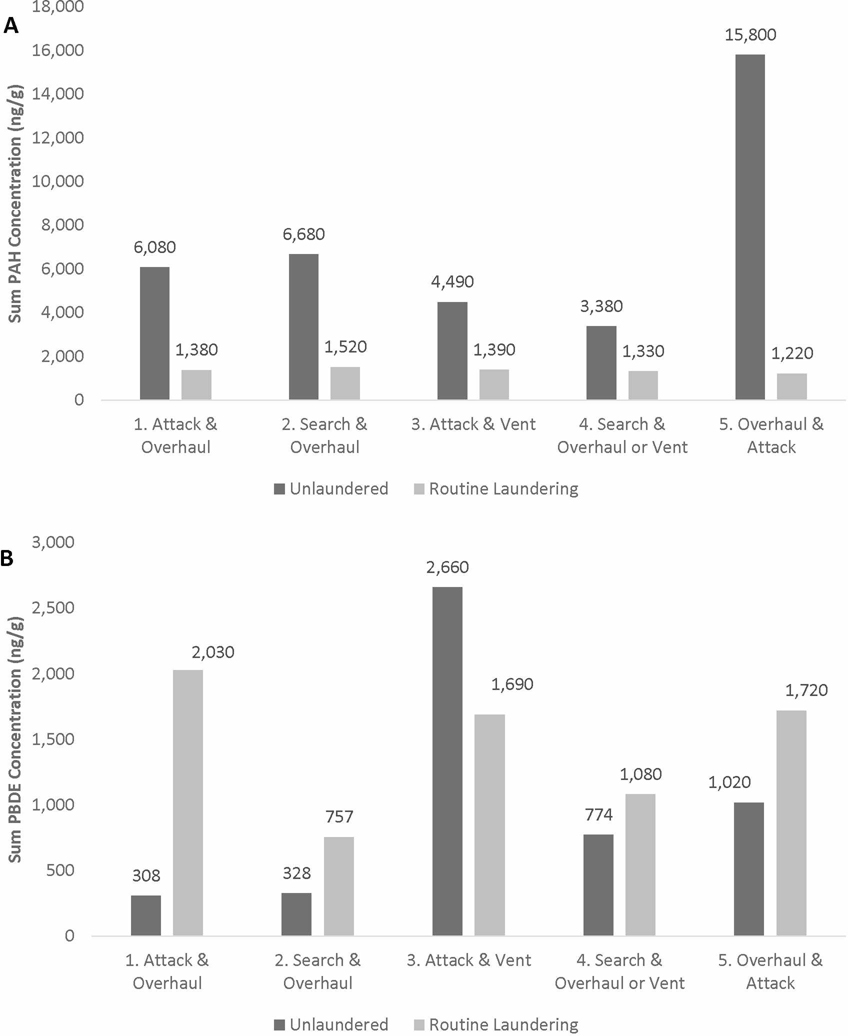
Figure 1A displays the total PAHs measured in the five unlaundered hoods and routinely laundered hoods, grouped by the fireground job assignment. Routinely laundered hoods in all five comparisons had markedly lower levels of total PAHs compared to the unlaundered hoods. When examining PAHs individually (supplemental materials, Table S1), most compounds were not detected on the routinely laundered hoods. Naphthalene was not detected in any hoods, which was expected given naphthalene’s volatile nature. Overall, total PAHs were on average 81% lower in routinely laundered hoods than unlaundered hoods.
Figure 1.
Total levels of (A) PAHs, (B) PBDEs, (C) NPBFRs, and (D) OPFRs measured in hoods routinely laundered or unlaundered after a total of 4 fire scenarios by job (1st two assignments & 2nd two assignments). All hoods (n=10) were exposed to 4 controlled modern structure fires. Routinely laundered hoods were laundered together after each exposure and unlaundered hoods were not laundered.
In the post-hoc testing, we saw a significant reduction in total PAHs in exposed hoods after a single laundering (Table 1; 76% decrease, P = 0.011). Interestingly, naphthalene was detected on two hoods after laundering, but not before. This is surprising given naphthalene’s volatile nature and the lack of naphthalene in unlaundered hood samples. Other than naphthalene, every other individual PAH decreased after laundering. Figure 2A also shows PAH levels before and after laundering for unexposed hoods. We measured either no change or a minimal increase in PAHs after laundering in these hoods and all levels were near detection limits.
Table 1.
Contamination levels of individual PAHs (ng/g) in exposed hoods before and after a single launderingA.
| Hoods before laundering (n=4) |
Hoods after laundering (n=4) |
|||||||
|---|---|---|---|---|---|---|---|---|
| CompoundB (IARCC) | No. above LODD | Mean | Standard deviation | No. above LOD | Mean | Standard deviation | Mean difference (%) | P-value |
| Benzo(a)anthracene (2B) | 4 | 418 | 254 | 3 | 101 | 42.2 | −75.9 | |
| Benzo(a)pyrene (1) | 4 | 570 | 311 | 4 | 105 | 41.6 | −81.6 | |
| Benzo(b)fluoranthene (2B) | 4 | 720 | 398 | 3 | 101 | 45.5 | −86.0 | |
| Benzo(g,h,i)perylene (3) | 4 | 548 | 323 | 3 | 140 | 42.7 | −74.4 | |
| Benzo(k)fluoranthene (2B) | 4 | 250 | 129 | 0 | 49.5F | 0.0F | −80.2 | |
| Chrysene (2B) | 4 | 540 | 441 | 1 | 76.7 | 31.3 | −85.8 | |
| Dibenzo(a,h)anthracene (2A) | 4 | 2,650 | 1,270 | 4 | 620 | 182 | −76.6 | |
| Fluoranthene (3) | 4 | 1,280 | 668 | 4 | 225 | 61.0 | −82.4 | |
| Indeno(1,2,3-cd)pyrene (2B) | 4 | 560 | 266 | 2 | 95.8 | 40.9 | −82.9 | |
| Phenanthrene (3) | 4 | 220 | 86.9 | 4 | 144 | 124 | −34.8 | |
| Pyrene (3) | 4 | 325 | 292 | 0 | 124F | 30.6F | −61.9 | |
|
| ||||||||
| Total PAHs E | 73% | 8,260 | 4,420 | 50% | 2,030 | 584 | −75.5 | 0.011 |
In calculating summary statistics, non-detectable levels were assigned values by taking the limit of detection divided by the square root of 2.
Anthracene (IARC=3), fluorene (IARC=3), and acenaphthene (IARC=3) were not detected in any hoods. Naphthalene (IARC=2B, 92–200 ng/g) were detected in two single washed hoods.
IARC classification categories: 1= Carcinogenic to humans, 2A=Probably carcinogenic to humans, 2B=Possibly carcinogenic to humans, 3=Not classifiable as to its carcinogenicity to humans(26)
Limit of detection (LOD) for PAHs ranged from 9 – 200 ng/g.
Total PAH summary statistics include PAHs not shown in table (anthracene, fluorene, acenaphthene, and naphthalene).
Mean and STD calculated from assigned values (LOD divided by square root of 2) because all samples were below LOD.
PBDE Contamination on Hoods
Figure 1B shows total PBDE concentrations in unlaundered and routinely laundered hoods by job assignment. In many cases, higher levels of PBDEs were measured in the routinely laundered hoods compared to the unlaundered hoods. For example, the routinely laundered hood for comparison 1 (attack & overhaul job assignment) had PBDE levels over 6 times higher than the unlaundered hood. With the exception of BDE-153, average concentrations were higher in routinely laundered hoods compared to unlaundered hoods for every detectable PBDE congener, and total PBDEs were on average 43% higher in the laundered hoods (supplemental materials, Table S2). For all hoods, BDE-209 was found at an order of magnitude higher concentration than any other PBDE detected.
In the post-hoc testing, the four exposed hoods were found to have higher PBDE concentrations after a single laundering than before (Table 2), but the difference was not statistically significant (mean 99% increase; P = 0.343). BDE-209 was again found at a higher magnitude than any other PBDE detected. Unexposed hoods laundered with exposed hoods also showed a substantial increase in PBDEs after laundering (Figure 2B). For example, PBDE levels in brand new unexposed hoods were below the respective detection limits before laundering, but ranged from 994–1820 ng/g after laundering.
Table 2.
Contamination levels of individual PBDEs in exposed hoods before and after a single laundering (ng/g)A.
| Hoods before laundering (n=4) |
Hoods after laundering (n=4)B |
|||||||
|---|---|---|---|---|---|---|---|---|
| Compound | No. above LODC | Mean | Standard deviation | No. above LOD | Mean | Standard deviation | Mean difference (%) | P-value |
| BDE-47 | 4 | 9.98 | 2.82 | 4 | 42.3 | 7.82 | 324 | |
| BDE-99 | 4 | 21.3 | 3.20 | 4 | 24.8 | 7.34 | 16.5 | |
| BDE-153 | 3 | 7.22 | 5.80 | 3 | 4.00 | 1.51 | −44.6 | |
| BDE-206 | 4 | 22.2 | 14.2 | 4 | 43.9 | 34.8 | 97.5 | |
| BDE-209 | 4 | 1,010 | 952 | 4 | 2,020 | 764 | 99.2 | |
|
| ||||||||
| Total PBDEs D,E | 53% | 1,080 | 957 | 69% | 2,140 | 813 | 98.9 | 0.343 |
In calculating summary statistics, non-detectable levels were assigned values by taking the limit of detection divided by the square root of 2.
Other hoods included in the wash cycle included new, unexposed hoods and hoods used in UL fire attack studies that had total PBDE contamination ranging from 670–12,200 ng/g.
BDE-100 (3.87–8.84 ng/g) detected in 4 single washed hoods and no unlaundered hoods. BDE-183 (7.95–12.3 ng/g) was detected in two single washed hoods and no unlaundered hoods. BDE-85 and BDE-154 were not detected in any hoods.
Limit of detection (LOD) for all PBDEs was 2 ng/g.
Total PBDE summary statistics include PBDEs not shown in table (BDE-85, BDE-100, BDE-154, and BDE-183).
NPBFR Contamination on Hoods
For all job assignment comparisons, NPBFR concentrations were lower (in one case, no substantial difference was noted) in routinely laundered hoods compared to unlaundered hoods (Figure 1C). BTBPE and HBCD were not detected in any laundered or unlaundered hoods. Mean concentrations of individual NPBFRs were lower in routinely laundered hoods than unlaundered hoods (supplemental materials, SIII). TBPH and TBBPA were detected on four unlaundered hoods, but only one laundered hood each. Total NPBFR concentrations were on average 66% lower in laundered hoods than unlaundered hoods.
In contrast, the post-hoc testing showed that NBPFRs were higher on exposed hoods after laundering than before (Table III), though the increase was not significant (mean 240% increase; P = 0.100). DBDPE in particular was much higher in these hoods post laundering (mean 458% increase). NPBFRs were also found in unexposed hoods after laundering (Figure 2C). In addition, the unexposed hoods that had been previously laundered 3 times appeared to retain more of the cross-contamination (by almost an order of magnitude) than the unexposed hoods that had not been previously laundered.
Table 3.
Contamination levels of individual NPBFRs in exposed hoods before and after a single laundering (ng/g)A.
| Hoods before laundering (n=4) |
Hoods after laundering (n=4)B |
|||||||
|---|---|---|---|---|---|---|---|---|
| Compound | No. above LODC | Mean | Standard deviation | No. above LOD | Mean | Standard deviation | Mean difference (%) | P-value |
| TBB | 4 | 34.2 | 25.9 | 4 | 28.4 | 13.7 | 16.9 | |
| TBPH | 3 | 13.9 | 9.48 | 4 | 7.83 | 6.93 | 43.5 | |
| DBDPE | 3 | 93.1 | 60.5 | 4 | 519 | 328 | 458 | |
| TBBPA | 3 | 18.7 | 20.1 | 0 | 1.54F | 0.317F | −91.8 | |
|
| ||||||||
| Total NPBFRs D,E | 41% | 165 | 112 | 38% | 562 | 348 | 240 | 0.100 |
In calculating summary statistics, non-detectable levels were assigned values by taking the limit of detection divided by the square root of 2.
Other hoods included in the wash cycle included new, unexposed hood and hoods used in UL fire attack studies with total NPBFRs ranging from 1360–4860 ng/g.
Not detected in any hoods: BTBPE and HBCD.
Limit of detection for all NPBFRs was 2 ng/g.
Total NPBFR summary statistics include NPBFRs not shown in table (BTBPE and HBCD).
Mean and STD calculated from assigned values (LOD divided by square root of 2) because all samples were below LOD.
OPFR Contamination on Hoods
When comparing contamination levels by job assignment, OPFR levels were generally lower in routinely laundered hoods compared to unlaundered hoods (Figure 1D). Exceptions to this were in comparison 2 (search & overhaul job assignment) and comparison 3 (attack & vent job assignment). TPP was the most abundant OPFR measured on unlaundered hoods (supplemental material). With the exception of TCPP, the individual OPFRs were 50–70% lower in the routinely laundered hoods, and total OPFRs were on average 56% lower in laundered hoods.
In the post-hoc testing, two of the four exposed hoods had higher OPFRs after laundering than before (Figure 2D). However, on average, OPFRs were lower in these hoods after laundering (Table IV), although this difference was not statistically significant (mean 42% decrease; P = 0.469). OPFRs were also detected on unexposed hoods after laundering (101–146 ng/g) despite non-detect values prior to laundering.
Table 4.
Contamination levels of individual OPFRs in exposed hoods before and after a single laundering (ng/g)A.
| Hoods before laundering (n=4) |
Hoods after laundering (n=4)B |
|||||||
|---|---|---|---|---|---|---|---|---|
| Compound | No. above LODC | Mean | Standard deviation | No. above LOD | Mean | Standard deviation | Mean Difference (%) | P-value |
| TCPP | 1 | 2.15 | 1.25 | 0 | 1.54F | 0.317F | −28.4 | |
| TDCPP | 4 | 72.0 | 63.8 | 0 | 1.54F | 0.317F | −97.9 | |
| TCP | 4 | 71.9 | 39.1 | 0 | 1.78F | 0.153F | −97.5 | |
| TPP | 4 | 294 | 259 | 4 | 251 | 93.2 | −14.8 | |
|
| ||||||||
| Total OPFRs D,E | 65% | 442 | 346 | 20% | 257 | 93.2 | −41.9 | 0.469 |
In calculating summary statistics, non-detectable levels were assigned values by taking the limit of detection divided by the square root of 2.
Other hoods included in the wash cycle included new, unexposed hoods and hoods used in Underwriters’ Laboratories fire attack studies with total OPFR contamination ranging from 2640–5130 ng/g.
Not detected in any hoods: TCEP.
Limit of detection for all OPFRs was 2 ng/g.
Total OPFR summary statistics include OPFRs not shown in table (TCEP).
Mean and STD calculated from assigned values (LOD divided by square root of 2) because all samples were below LOD.
DISCUSSION
All unexposed, unlaundered hood samples were non-detect for FRs and PAHs. This suggests all contamination detected in hoods were from exposure to smoke from the live-fire scenarios and/or cross-contamination during laundering, and not present in the hoods from the manufacturing process. Additionally, all unexposed, previously laundered 3 times hood samples were non-detect for FRs and PAHs, suggesting the washing machine and laundry detergent were not a source of contamination.
Routine laundering appeared to reduce PAH contamination in hoods by an average of 81%. When examining hoods before and after a single laundering, we found a similar reduction (76%) that was statistically significant (P = 0.011). Because we assigned a value to each PAH analyte that was below LOD (LOD divided by square root of 2), an 85–90% reduction is the best achievable contamination reduction. These results support our findings from a previous study(10) which found that field decontamination with dish soap, water, and scrubbing was able to reduce PAH surface contamination on turnout gear by 85%. There was some evidence for cross contamination with PAHs in the unexposed hoods post-laundering; however, the levels were near detection limits and may not present a meaningful exposure risk. Interestingly, phenanthrene, which was the only compound with increased concentration on routinely laundered hoods, had the least reduction in the post-hoc testing. Nevertheless, the results show that routine laundering of hoods may be an effective way to reduce PAH contamination on hoods and minimize or prevent secondary exposure.
In contrast to the PAHs, PBDEs do not appear to be effectively removed through laundering. The apparent increase in PBDEs found in routinely laundered hoods vs unlaundered hoods was most likely from cross-contamination (transfer of PBDE contaminants from other hoods that were laundered at the same time). Results of the post-hoc testing support this theory, as PBDE concentrations in exposed hoods were higher on average after laundering than before. In addition, unexposed hoods that were all non-detect before laundering were found to be contaminated with PBDEs after laundering (ranging 994 – 1,820 ng/g). It is important to note that the four additional hoods included in this experiment were heavily contaminated with PBDEs (672–12,200 ng/g) and, as such, likely provided a significant reservoir for cross contamination.
A study conducted by Saini et al. (28) found that over 90% of the PBDEs contaminating polyester samples were not removed through traditional laundering, indicating poor extraction into laundry water. Repeated use of laundry machines could lead to accumulation of contaminants, and in fact, one study detected a variety of PBDEs in dryer lint.(29) Although we did not use a dryer for this study, it is possible that laundering soiled hoods could lead to residual PBDE contamination inside the extractors. Both our results and the findings by Saini et al. (28) appear to suggest that laundering does not efficiently remove PBDEs from certain synthetic fabrics (e.g. Nomex® or polyester). The PBDEs that are extracted into laundry water may then transfer to other items in the washing machine. It is important to note that the chemical properties of the contaminant (e.g., lipophilicity) may play a role in its retention on fabrics. How this contamination translates into firefighters’ exposure to PBDEs from subsequent use of hoods is not well understood and would depend largely on the migration of these compounds from the Nomex fabric to and through the skin.
NPBFR contamination appeared to be reduced by routinely laundering hoods. However, this was not supported by the post-hoc testing results, where exposed hoods had higher concentrations of NPBFRs after laundering. In addition, NPBFR contamination was found on new unexposed hoods after laundering with contaminated hoods, indicating cross contamination with NPBFRs, and this increase in contamination was nearly an order of magnitude greater in the hoods that had been previously laundered 3 times. This may indicate that the softening of the Nomex fabric or change in fiber/fabric surface treatments from repeated laundering allowed the hoods to adsorb more of these specific contaminants from the laundry water. However, we found no visual evidence of changing fiber density using microscopy (supplemental materials).
The conflicting NPBFR results from the two experiments may be due in part to the high contamination levels present in the additional soiled hoods in the post-hoc testing (1360–4860 ng/g). These levels were up to an order of magnitude greater than the contamination levels measured in the exposed hoods before laundering. Of note, the additional soiled hoods contained levels of TBBPA (3.5–46.4 ng/g) that were on par with the exposed hoods (1.39– 52.3 ng/g), and, interestingly, 92% of the TBBPA contamination on the exposed hoods were removed via laundering. These findings indicate that the effectiveness of removing NPBFRs by laundering may depend on the initial contamination levels present in the load of laundry.
Testing of OPFRs provided mixed results. In comparing routinely laundered hoods to unlaundered hoods, some comparisons (by job assignment) showed substantial decreases and others did not. However, total OPFRs on routinely laundered hoods were on average 56% lower than on unlaundered hoods. Similarly, in the post-hoc testing, some exposed hoods were found to have lower OPFR levels after laundering and others did not, but on average, OPFRs decreased by 42%. Importantly, OPFRs were found on all unexposed hoods after laundering, indicating some level of cross contamination. It is worth noting that the additional soiled hoods had OPFR contamination (2650–5130 ng/g) that were up to an order magnitude higher than the levels measured on the exposed hoods before laundering(299–1,030 ng/g).
A recent study found OPFRs were present in laundry wastewater after washing clothes exposed to OPFR dust, suggesting laundering effectively extracts OPFRs from clothes to water.(30) This is to be expected given that OPFRs are relatively hydrophilic compounds with high water solubility (e.g. TCPP 1200 mg/L water solubility).(31) Another study found laundering removes 80% of selected OPFRs from polyester.(28) The results from our study seem to indicate that laundering extracts a large percentage of OPFRs, but that these compounds may be readsorbed by the materials being washed.
This study had a few limitations. First, routinely laundered hoods cannot be directly compared to unlaundered hoods because the amount of contamination present on the two sets of hoods depends largely on the job assignment of firefighters wearing the hoods. We attempted to control for this confounder by running comparisons by similar job assignment pairings. Secondly, in the post-hoc study, we included heavily contaminated hoods from a UL fire attack study. Because these hoods were much more contaminated on average than the other exposed hoods, we may have increased the probability of detecting cross contamination. On the other hand, it would not be uncommon in the fire service to have numerous hoods with varying levels of contamination in the same load of laundry. In addition, because we did not test the UL hoods post laundering, we were not able to quantify the extraction of their contaminants into laundry water and their relative contribution to the cross contamination levels found on the other hoods. Lastly, bulk sampling is susceptible to spatial variability in contamination. It is possible that one area of a hood had more contamination than another area. We tried to minimize this confounder by selecting similar locations of the paired hoods or side-by-side locations for sampling.
CONCLUSIONS
Our hypothesis was that laundering would reduce FR and PAH contamination to normal background or non-detectable levels. Results suggest that the effectiveness of laundering depends largely on the type of chemicals under inspection, as well as the amount of contamination present in the load of laundry. Our study consistently showed that a large percentage of PAHs were removed from hoods during laundering. The results also suggest that the majority of NPBFR and OPFR contamination will be removed via routine laundering. However, routine laundering did not appear to effectively remove PBDE contamination. Moreover, in the post-hoc experiment, when more contaminated hoods were included in the laundry cycle, NPBFRs, OPFRs, and PBDEs were detected on new hoods that had never been used in live fires, providing clear evidence of cross contamination. This cross contamination led to reduced cleaning efficiency and, in some cases, the exposed hoods were more contaminated with FRs after laundering than before.
This study provided some evidence that repeated laundering of the hoods created fabric conditions that were more adsorptive of NPBFRs; however, given the small sample sizes, further research is necessary. While beyond the scope of this paper, the properties of the fabric (e.g., lipophilicity) may also play a role in the retention of certain contaminants and should be investigated. Additional research should also explore the effect that successive laundry cycles, different types of detergent (even alternative cleaning technologies), and hood materials (e.g., PBI®, Lenzing FR®, etc.) have on contamination and cleaning efficiency. Separating firefighter hoods by potential for contamination (i.e., job assignment) and from other clothing and PPE during laundering should reduce the potential for cross contamination. Laundering will remove many contaminants from hoods and should be performed after live-fire responses. However, our study indicates that PBDEs contaminants in particular may be difficult to remove at least with currently prescribed laundry procedures. Understanding how this translates to firefighter exposure is of utmost importance for future studies.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to acknowledge the assistance received with this study. We thank Kenneth Sparks and Donald Booher for processing and submitting all hood samples for analysis and Joseph Fernback for microscopy of the fabric samples. Most of all, we thank the firefighters for participating in the larger study, of which the hood analysis was just one component. This study was approved by the Institutional Review Boards at NIOSH and the University of Illinois. This study was funded through a U.S. Department of Homeland Security, Assistance to Firefighters Grant (EMW-2013-FP-00766, EMW-2013-FP-00644, and EMW-2015-FP-00646). This project was also made possible through a partnership with the CDC Foundation. This study was supported in part by an interagency agreement between NIOSH and the National Institute of Environmental Health Sciences (AES15002) as a collaborative National Toxicology Program research activity. This paper is contribution No.#3786 of the Virginia Institute of Marine Science, College of William & Mary.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC). Mention of any company name or product does not constitute endorsement by NIOSH/CDC.
REFERENCES
- 1.Daniels RD, Bertke S, Dahm M, Yiin JH, Kubale TL, Hales TR, et al. : Exposure–response relationships for select cancer and non-cancer health outcomes in a cohort of US firefighters from San Francisco, Chicago and Philadelphia (1950–2009). Occupational and Environmental Medicine 72(10):699–706 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lemasters GK, Genaidy AM, Succop P, Deddens J, Sobeih T, Barriera-Virut H, et al. : Cancer Risk Among Firefighters: A Review and Meta-analysis of 32 Studies. Journal of Occupational and Environmental Medicine 48(11):1189–1202 (2006). [DOI] [PubMed] [Google Scholar]
- 3.Fent KW, Eisenberg J, Snawder J, Sammons D, Pleil J, and Stiegel M: Systemic Exposure to PAHs and Benzene in Firefighters Suppressing Controlled Structure Fires. The Annals of Occupational Hygiene 58(7):830–845 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cordner A, Rodgers K, Brown P, and Morello-Frosch R: Firefighters and flame retardant activism. New Solutions: A Journal of Environmental and Occupational Health Policy 24(4):511–534 (2015). [DOI] [PubMed] [Google Scholar]
- 5.Brown FR, Whitehead TP, Park JS, Metayer C, and Petreas MX: Levels of non-polybrominated diphenyl ether brominated flame retardants in residential house dust samples and fire station dust samples in California. Environmental Research 135:9–14 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Easter E, Lander D, and Huston T: Risk assessment of soils identified on firefighter turnout gear. Journal of Occupational and Environmental Hygiene 13(9):647–657 (2016). [DOI] [PubMed] [Google Scholar]
- 7.Alexander BM and Baxter CS: Flame-retardant contamination of firefighter personal protective clothing – A potential health risk for firefighters. Journal of Occupational and Environmental Hygiene 13(9):1–26 (2016). [DOI] [PubMed] [Google Scholar]
- 8.Shen B, P Whitehead T, Mcneel S, Brown FR, Dhaliwal J, Das R, et al. : High Levels of Polybrominated Diphenyl Ethers in Vacuum Cleaner Dust from California Fire Stations. Environmental Science & Technology 49(8):4988–4994 (2015). [DOI] [PubMed] [Google Scholar]
- 9.National Fire Protection Association (NFPA). Standard on Protective Ensembles for Structural Fire Fighting and Proximity Fire Fighting (NFPA 1971). [Standard]
- 10.Dreij K, Mattsson Å, Jarvis IW, Lim H, Hurkmans J, Gustafsson J, et al. Cancer Risk Assessment of Airborne PAHs Based on in Vitro Mixture Potency Factors. Environmental Science & Technology 51(15):8805–8814 (2017) [DOI] [PubMed] [Google Scholar]
- 11.Fent KW, Alexander B, Roberts J, Robertson S, Toennis C, Sammons D, et al. : Contamination of firefighter personal protective equipment and skin and the effectiveness of decontamination procedures. Journal of Occupational and Environmental Hygiene 14(10):801–814 (2017). [DOI] [PubMed] [Google Scholar]
- 12.Siddiqi MA, Laessig RH, and Reed KD: Polybrominated Diphenyl Ethers (PBDEs): New Pollutants-Old Diseases. Clinical Medicine & Research 1(4):281–290 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dishaw LV, Powers CM, Ryde IT, Roberts SC, Seidler FJ, Slotkin TA, and Stapleton HM: Is the PentaBDE replacement, tris (1,3-dichloro-2-propyl) phosphate (TDCPP), a developmental neurotoxicant? Studies in PC12 cells. Toxicology and Applied Pharmacology 256(3):281–289 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.House SC (n.d.): “Information on the 16 chemicals added to the Stockholm Convention.” Available at http://chm.pops.int/TheConvention/ThePOPs/TheNewPOPs/tabid/2511/Default.aspx (accessed August 30, 2017).
- 15.Linares V, Bellés M, and Domingo JL: Human exposure to PBDE and critical evaluation of health hazards. Archives of Toxicology 89(3):335–356 (2015) [DOI] [PubMed] [Google Scholar]
- 16.Park J, Voss RW, Mcneel S, Wu N, Guo T, Wang Y, et al. : High Exposure of California Firefighters to Polybrominated Diphenyl Ethers. Environmental Science & Technology 49(5):2948–2958 (2015). [DOI] [PubMed] [Google Scholar]
- 17.Covaci A, Harrad S, Abdallah MA, Ali N, Law RJ, Herzke D, et al. : Novel brominated flame retardants; a review of their analysis, environmental fate, and behavior. Environ. Int. 37: 532–556 (2011). [DOI] [PubMed] [Google Scholar]
- 18.Behl M, Rice JR, Smith MV, Co CA, Bridge MF, Hsieh J, et al. : Editor’s Highlight: Comparative Toxicity of Organophosphate Flame Retardants and Polybrominated Diphenyl Ethers toCaenorhabditiselegans. Toxicological Science 154(2):241–252 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saunders DM, B Hagley E, Hecker M, Mankidy R, and Giesy JP: In Vitro endocrine disruption and TCDD-like effects of three novel brominated flame retardants: TBPH, TBB, and TBCO. Toxicology Letters 223(2):252–259 (2013). [DOI] [PubMed] [Google Scholar]
- 20.Shaw SD, Berger ML, Harris JH, Yun SH, Wu Q, Liao C, et al. : Persistent Organic Pollutants Including Polychlorinated and Polybrominated dibenzo-p-dioxins and Dibenzofurans in Firefighters from Northern California. Chemosphere 91:1386–1394 (2013). [DOI] [PubMed] [Google Scholar]
- 21.Jayatilaka NK, Restrepo P, Williams L, Ospina M, Valentin-Blasini L, and Calafat AM: Quantification of three chlorinated dialkyl phosphates, diphenyl phosphate, 2,3,4,5-tetrabromobenzoic acid, and four other organophosphates in human urine by solid phase extraction-high performance liquid chromatography-tandem mass spectrometry. Analytical and Bioanalytical Chemistry 409(5):1323–1332 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horn GP, Kesler RM, Kerber S, Fent KW, Schroeder TJ, Scott WS, et al. : Thermal response to firefighting activities in residential structure fires: impact of job assignment and suppression tactic. Ergonomics 61(3):404–419(2017). [DOI] [PubMed] [Google Scholar]
- 23.Horn G,Kerber S, Fent KW, Fernhall B and Smith D (n.d.): “Interim Report: Cardiovascular and Chemical Exposure Risks in Modern Firefighting (Rep.).” Available at: https://www.fsi.illinois.edu/documents/research/CardioChemRisksModernFF_InterimReport2016.pdf. (accessed August 24, 2018).
- 24.Zevotek R, Stakes K, and Willi J (2018): “Impact of fire attack utilizing interior and exterior streams on firefighter safety and occupant survival: Full Scale Experiments.” Columbia, MD: Underwriters Laboratory, Firefighter Safety Research Institute. Available at: https://ulfirefightersafety.org/docs/DHS2013_Part_III_Full_Scale.pdf (accessed August 24th, 2018) [Google Scholar]
- 25.“NIOSH manual of analytical methods (4th ed.).” Available at https://www.cdc.gov/niosh/docs/2003-154/pdfs/5506.pdf. (accessed August 24th, 2018).
- 26.La Guardia MJ and Hale RC: Halogenated flame-retardant concentrations in settled dust, respirable and inhalable particulates and polyurethane foam at gymnastic training facilities and residences. Environ. Int. 79:106–114 (2015). [DOI] [PubMed] [Google Scholar]
- 27.“Agents Classified by The IARC Monographs, Volumes 1–119” [Online] Available at http://monographs.iarc.fr/ENG/Classification/ (accessed October 2, 2017).
- 28.Saini A, Thaysen C, Jantunen L, Mcqueen RH, and Diamond ML: From Clothing to Laundry Water: Investigating the Fate of Phthalates, Brominated Flame Retardants, and Organophosphate Esters. Environmental Science & Technology 50(17):9289–9297 (2016). [DOI] [PubMed] [Google Scholar]
- 29.Stapleton HM, Dodder NG, Offenberg JH, M Schantz M, and Wise SA: Polybrominated Diphenyl Ethers in House Dust and Clothes Dryer Lint. Environmental Science & Technology 39(4):925–931 (2005). [DOI] [PubMed] [Google Scholar]
- 30.Schreder ED and Guardia MJ: Flame Retardant Transfers from U.S. Households (Dust and Laundry Wastewater) to the Aquatic Environment. Environmental Science & Technology 48(19):11575–11583 (2014). [DOI] [PubMed] [Google Scholar]
- 31.Cao S, Zeng X, Song H, Li H, Yu Z, Sheng G, and Fu J: Levels and distributions of organophosphate flame retardants and plasticizers in sediment from Taihu Lake, China. Environmental Toxicology and Chemistry 31(7):1478–1484 (2012). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.