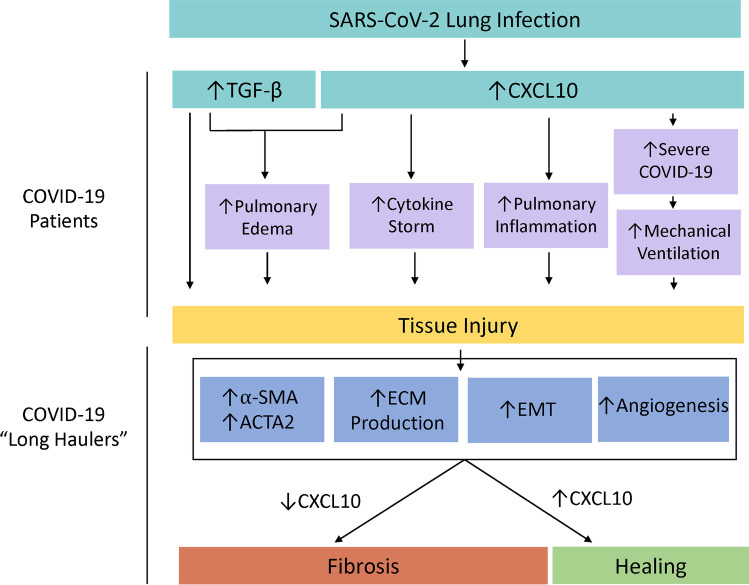
Fig. 3.
A diagram displaying the adherent pathologies and outcomes associated with SARS-CoV-2-induced TGF-β and CXCL10 upregulation in the lung which culminate in tissue injury in COVID-19 patients and subsequently manifests fibrosis in COVID-19 long-haulers which can uniquely be targeted by CXCL10-centric therapeutics. COVID-19-related tissue injury is thought to be twofold and results from both direct upregulation of the pro-fibrotic growth factor, TGF-β, but also from tissue damage initiated by a highly inflammatory state. CXCL10 and TGF-β both enhance pulmonary edema [19, 88•]. CXCL10 plays a critical role by upregulation of the cytokine storm [54, 70] and increasing pulmonary inflammation [86•]. Furthermore, CXCL10 is associated with COVID-19 disease severity which increases the likely need for mechanical ventilation, which leads to pulmonary fibrosis [92]. However, in COVID-19 long-haulers, amplifying the CXCL10-CXCR3 signaling system may in fact benefit patients by inhibiting many pro-fibrotic pathologies expected clinically [130, 131], such as through the upregulation of α-SMA, ACTA2, ECM protein, EMT, and angiogenesis [127, 128]