Abstract
Aim
Nationwide lockdowns and social restrictions during the COVID‐19 pandemic have reduced childhood infections. We assessed how many items of systemic antibiotics and asthma medicines were dispensed to children aged 0−12 years in Finland before and during the pandemic and analysed the reimbursement costs.
Methods
The data came from the national Finnish register of reimbursable prescriptions, which is maintained by the country's Social Insurance Institution. It included all prescriptions for antibiotics and asthma medicines dispensed to children aged 0−12 years in 2019 and 2020. Prescription rates per 1000 children were calculated for each quarter and compared using rate ratios and 95% confidence intervals (95% CI).
Results
Overall dispensing for antibiotics decreased by 55.3% and was most prominent for macrolides for children aged 0−5 years (59.6%, 95% CI 60.9%−58.2%). Asthma medicines decreased by 19.8%, and the most prominent reduction was in short‐acting beta‐agonists for children aged 0−5 years (35.2%, 95% CI 36.1%−34.2%). These reduced reimbursement costs by 3.4 million Euros from 2019 to 2020.
Conclusion
This nationwide study showed that the number of antibiotics and asthma medicines decreased by 59.6% and 19.8% respectively from 2019 to 2020, generating a cost saving of 3.4 million Euros.
Keywords: antibiotics, asthma medication, childhood infections, pandemic, reimbursement costs
Abbreviations
- COVID‐19
Coronavirus disease of 2019
- WHO
World Health Organization
- 95% CI
95% confidence intervals
Key notes.
COVID‐19 restrictions have decreased childhood infections, and we compared how many systemic antibiotics and asthma medicines were dispensed in Finland in 2019 and 2020.
Antibiotics decreased by 55.3%, and the changes were most prominent for macrolides for children aged 0−5 years and asthma medicines decreased by 19.8% and were highest for short‐acting beta‐agonists for children aged 0−5 years.
These reduced reimbursement costs by 3.4 million Euros from 2019 to 2020.
1. INTRODUCTION
The World Health Organization (WHO) declared COVID‐19 a global pandemic on 11 March 2020, and this triggered a range of restrictive measures, from social distancing to full lockdowns. Finland went into lockdown on 16 March, schools were closed, and travel and social distancing restrictions were put in place. Face masks were not required. These restrictions were relaxed during the summer, and schools opened on 14 May, but face mask recommendations came into force for people aged 15 years plus in August when rates started to rise. The second wave restrictions in the autumn were mainly aimed at adults and based on regional infection rates (Appendix S1).
Several studies have shown that the restrictive measures during the first wave of COVID‐19 in spring 2020 reduced the rates of other infections, such as respiratory infections, acute otitis media and gastroenteritis. 1 , 2 , 3 , 4 , 5 The overall number of emergency visits and hospitalisations due to respiratory infectious diseases decreased globally in children. 2 , 6 , 7 , 8 The same was true for asthma, 9 , 10 , 11 and this effect seemed to last after lockdowns in autumn 2020. 11 In addition, asthma control appeared to improve in about 20%–30% of children during spring 2020, based on an Italian study and a global survey of practitioners. 12 , 13
The number of antibiotics that were prescribed and dispensed fell during the spring 2020 lockdown in northern Italy, which had a higher number of COVID‐19 cases than Finland and longer restrictions. 14 , 15 Gagliotti et al. studied prescriptions that were dispensed to the general Italian population from March to May 2020 and reimbursed by a regional health authority in northern Italy. They found that systemic antibiotics decreased during lockdown, and systemic antibacterial medication showed a remarkable reduction in children when they compared the data to the same period in 2018 and 2019. 14 Torretta et al. remotely followed 102 children who were prone to otitis media and were managed by a tertiary outpatient clinic in Milan, Italy, using telemedicine. They found that there was a significant reduction in systemic antibiotic treatments when they compared the lockdown period of February to April 2020 to the same period in 2019. 15
The aim of this study was to evaluate whether reduced infection rates were reflected by a decline in the number of systemic antibiotics and asthma medicines dispensed to children aged 0–12 in Finland in 2020. We also compared the number of primary care visits in children in 2020 to those in 2019. Finally, we examined what impact any changes in dispensing levels had on reimbursement rates.
2. MATERIALS AND METHODS
2.1. Materials
We collected the data for this retrospective register study from nationwide open‐access registers. All Finnish children are eligible to receive free public health care, and their parents can receive partial or full reimbursement on any prescriptions that are dispensed. This reimbursement is discounted from the price of the medicines when the items are dispensed in the pharmacy, and the pharmacy then claims back the discount from the Social Insurance Institution of Finland. The information on medical drug use was collected from the register of reimbursed prescription medicines, which is maintained by the institution. 16 The open‐access data were provided in quarters. The data included the number of prescriptions for antibiotics and asthma medicine that were dispensed for children aged 0–12 years in 2019 and 2020 and subsequently reimbursed. The data covered prescriptions from primary, secondary, tertiary and private care institutions. The age groups were based on the design of the register. Systemic antibiotics included all antibacterial medications for systemic use with an Anatomical Therapeutic Chemical code of J01. Asthma medicines included all medicines used for obstructive airway diseases with a code of R03. The grouping of the systemic antibiotics and asthma medicines is provided in Appendix S2.
We collected the number of primary care visits by children from the Care Register maintained by the Finnish Institute for Health and Welfare. 17 This register data had some limitations, due to low reporting quality, but it have been estimated to cover more than 60% of such visits. 18 We gathered data for primary care visits from 2019 to 2020 for children aged 0–14 years, as this was the age range used in the register. This differed from the 0 to 12 years used in the register of reimbursed prescription medicines and the Care Register. The overall population of children in each age group in 2019 and 2020 was collected from Statistics Finland and used as nominators in the analysis. 19 Local ethical committee approval was not needed, due to the open‐access register‐based study design and because the data were collected without the need for any identifying information. The original data used in this study are available on request.
2.2. Methods
We calculated prescription (dispensed medicines from pharmacy) rates from reimbursed medicines per 1000 children and the changes between 2019 and 2020 with 95% confidence intervals (95% CI). Furthermore, we conducted age‐ stratified analyses for children aged 0–5 and 6–12 years. These age groups were based on openly available register data. We have presented the primary care visit data for children aged 0–14 years as a 14 days rolling average, in order to estimate the trends in visit rates and to minimise the daily variations between weeks with lower visit rates during weekends and holidays.
Trimethoprim and sulfadiazine were excluded from the analyses because there was a change in the reimbursement status for these medicines in 2020, and this meant that it was not possible to compare the data between the two years. We conducted all analyses using SPSS, version 27.0 (IBM Corp).
2.3. Restrictions
The year 2020 was divided into four quarters due to the use of group‐level register data. The first quarter from 1 January to 31 March included the time before the pandemic and the beginning of the lockdown from 16 March, when schools closed. The second quarter from 1 April to 30 June included the lockdown and the relaxation of the first restrictions from 14 May, when schools opened again. The third quarter from 1 July to 30 September included the relaxed restrictions during the summer and the beginning of the regional restrictions from September. The fourth quarter included the regional restrictions for the rest of the year. A more precise description of the implemented restrictions is provided in Appendix S1.
3. RESULTS
3.1. Antibiotics
The data comprised 331,857 dispensed prescriptions for courses of antibiotics. Of these, 69.1% were dispensed in 2019 and 30.9% in 2020. The total reimbursable expenses were 1,956,154 Euros in 2020 and 4,295,412 Euros in 2019, which was a saving of 2.3 million Euros (54.5%). The most common antibiotic in 2019–2020 was amoxicillin, which accounted for 55.4% of the antibiotics dispensed. Less than a third of these (30.1%) were dispensed in 2020. The number of dispensed prescriptions for all antibiotics fell by 55.3% in 2020. The biggest decrease was for macrolides (59.2%), and the smallest was for cephalosporins (31.7%).
Dispensed antibiotics per 1000 children aged 0–5 years decreased by 55.9% (95% CI 56.3%–55.5%) in 2020 (Table 1), and the highest reduction was for macrolides (59.6%, 95% CI 60.9%–58.2%). In children aged 6–12 years, the overall antibiotic dispensing rate reduced by 51.9% in 2020 (95% CI 52.4%–51.3%) and dispensed prescriptions for amoxicillin decreased the most, by 57.6% (95% CI 58.4%–56.8%).
TABLE 1.
Antibiotics dispensed per 1000 children in 2019 and 2020 in Finland
| 0–5 years | 6–12 years | |||||||
|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | Change | 95% CI | 2019 | 2020 | Change | 95% CI | |
| All antibiotics | 444.9 | 196.1 | −55.9% | −56.3% to −55.5% | 205.5 | 98.9 | −51.9% | −52.4% to −51.3% |
| Amoxicillin | 289.8 | 129.8 | −55.2% | −55.7% to −54.7% | 85.7 | 36.4 | −57.6% | −58.4% to −56.8% |
| Amoxicillin +clavulanic acid | 112.5 | 48.7 | −56.7% | −57.5% to −55.8% | 28.3 | 13.1 | −53.7% | −55.2% to −52.2% |
| Cephalosporins | 1.3 | 0.6 | −50.9% | −58.7% to −41.6% | 34.8 | 24.0 | −31.0% | −32.7% to −29.2% |
| Macrolides | 39.4 | 15.9 | −59.6% | −60.9% to −58.2% | 20.1 | 8.8 | −56.5% | −58.1% to −54.8% |
| Other | 2.0 | 1.0 | −47.3% | −54.0% to −39.6% | 36.7 | 16.7 | −54.5% | −55.7% to −53.2% |
95% CI; 95% confidence intervals.
Furthermore, the number of dispensed prescriptions in 2020 was lowest in the second quarter in all antibiotic groups, with the exception of the group for other antibiotics (Figure 1). The overall decrease in the second quarter was 84.4% compared with the same quarter in 2019. The number of dispensed prescriptions slightly increased in the third quarter in all antibiotic groups, but decreased again in the fourth quarter for amoxicillin, cephalosporins and other antibiotics (Figure 1).
FIGURE 1.
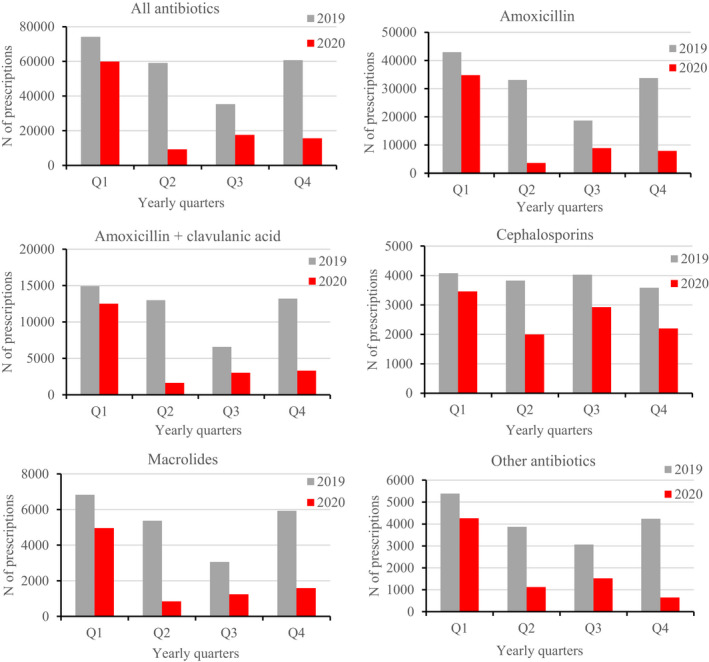
Number of dispensed antibiotic items for children aged 0–12 years in 2019 and 2020 in Finland
3.2. Asthma medicines
A total of 337,911 asthma medicine items were dispensed in 2019–2020: 55.5% in 2019 and 44.5% in 2020. Total reimbursable expenses in 2020 were 2,948,815 Euros and 3,830,713 Euros in 2019, which was a saving of 0.88 million Euros (23.0%). Overall, the number of dispensed asthma medicines decreased in 2020, except for the group of other asthma medicines, which was higher than in 2019. The most commonly dispensed medicines were short‐acting beta‐agonists, which accounted for 46.2% of the asthma medicine items. Of those, 42.1% were dispensed in 2020. The number of asthma medicine prescriptions dispensed decreased by 19.8% in 2020 and the number of short‐acting beta‐agonist prescriptions dispensed reduced the most, by 27.3%.
The number of asthma medicine prescriptions dispensed per 1,000 children decreased by 28.8% (95% CI 29.6%–28.1%) for children aged between 0 and 5 years and decreased by 10.4% (95% CI 11.2%–9.6%) for children aged between 6 and 12 years (Table 2). The number of dispensed short‐acting beta‐agonist prescriptions decreased most for children aged between 0 and 5 years (35.2%, 95% CI 36.1%–34.2%) and for children aged between and −12 years (16.6%, 95% CI 17.7%–15.4%).
TABLE 2.
Asthma medicine items dispensed per 1000 children in 2019 and 2020 in Finland
| 0–5 years | 6–12 years | |||||||
|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | Change | 95% CI | 2019 | 2020 | Change | 95% CI | |
| All asthma medicines | 264.1 | 188.0 | −28.8% | −29.6% to −28.1% | 240.4 | 215.3 | −10.4% | −11.2% to −9.6% |
| Short‐acting beta‐agonists | 147.0 | 95.3 | −35.2% | −36.1% to −34.2% | 101.8 | 84.9 | −16.6% | −17.7% to −15.4% |
| Inhaled corticosteroids | 80.3 | 63.7 | −20.6% | −22.1% to −19.1% | 78.8 | 72.5 | −7.9% | −9.3% to −6.5% |
| Inhaled corticosteroids+long‐acting beta‐agonists | 15.8 | 14.3 | −9.6% | −13.2% to −5.8% | 36.9 | 38.3 | 3.7% | 1.5% to 6.0% |
| Montelukast | 20.7 | 14.3 | −30.9% | −33.5% to −28.2% | 22.5 | 18.9 | −15.7% | −18.1% to −13.2% |
| Other | 0.3 | 0.4 | 23.1% | −5.5% to 60.4% | 0.4 | 0.6 | 36.1% | 12.7% to 64.4% |
95% CI; 95% confidence intervals.
In the first quarter of 2020, the number of asthma medicine prescriptions that were dispensed was 19.6% higher than in 2019 (Figure 2). In the second quarter, the number of dispensed prescriptions was at its lowest in all other groups, except for Montelukast in 2020. The overall decrease in the second quarter was 49.9%. After quarter one, the number of prescriptions that were dispensed mainly remained lower in 2020 than in 2019.
FIGURE 2.
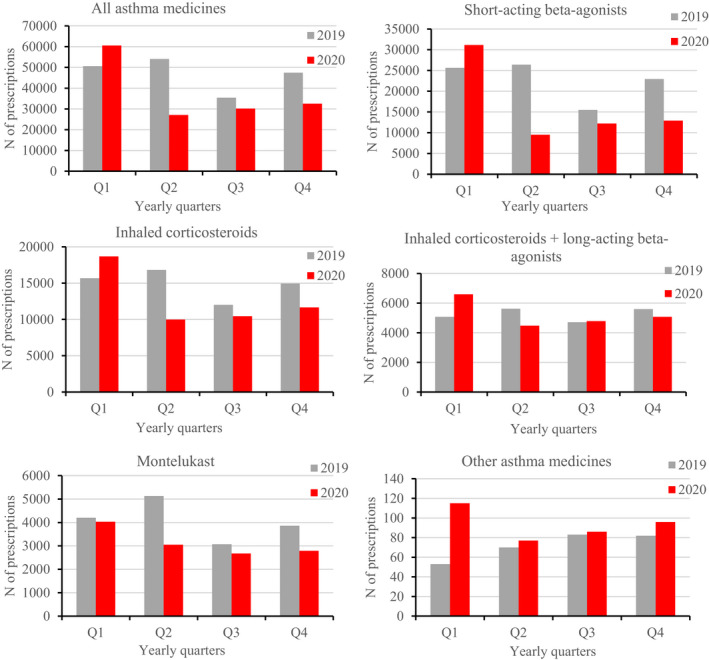
Number of dispensed asthma medicine items for children aged 0–12 years in 2019 and 2020 in Finland
The total savings in reimbursement costs for systemic antibiotics and asthma medication in Finland for children aged 0–12 was 3.4 million Euros in 2020.
3.3. Primary care visits
Children aged 0–14 years made 7,909,388 primary care visits in 2019–2020: 48.0% were in 2020 and 52.0% were in 2019. In 2020, the number of visits decreased below the 2019 level in the second quarter, but were higher than 2019 during the third and fourth quarters (Figure 3).
FIGURE 3.
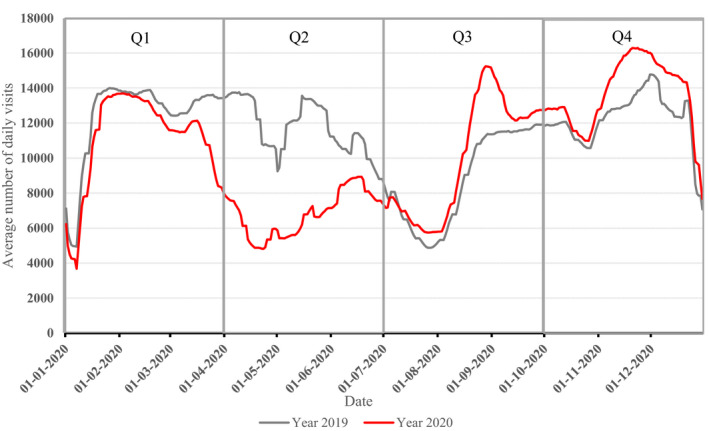
Nationwide 14 days rolling mean visit rate for children aged 0–14 years in primary health care from 2019 to 2020 in Finland
4. DISCUSSION
Our results demonstrate that the first lockdown reduced the dispensing rates for systemic antibiotics and most of the asthma medicines available for Finnish children aged 0–12 years. These reductions lasted for the rest of 2020 and led to major savings in reimbursement costs in 2020, of 3.4 million Euros. Due to the lockdown and the reorganisation of healthcare resources, the number of primary care visits temporarily decreased below the 2019 level from March to June 2020, but recovered from August onwards and were then higher in 2020 than in 2019.
The use of antibiotics has become an increasingly important topic since the onset of the pandemic, as antimicrobial resistance has increased due to the overuse of antibiotics in patients with COVID‐19. 20 , 21 The lower number of all systemic antibiotics that were dispensed in Finland in our study indicates that this overuse was unlikely to be due to children aged 0–12 years. Moreover, the greatest reduction was seen in macrolides, which are indicated for atypical pneumonia and pertussis, but are sometimes used for other respiratory infections. 22
In addition to common side effects, such as diarrhoea and rashes, antibiotics may also cause long‐term harm for children. It has been suggested that changes in the microbiome due to using antibiotics during childhood have been associated with increased risks of asthma, 23 , 24 obesity 25 , 26 and appendicitis. 27 As every course of antibiotics also increases the risk of antimicrobial resistance, reducing the use of systemic antibiotics can be seen as a positive effect of lockdown and social restrictions due to COVID‐19.
Our study demonstrated that the number of asthma medicine prescriptions that were dispensed was higher in early 2020 than in 2019. An Italian study reported that parents or family paediatricians were more likely to spontaneously modify children's asthma maintenance therapy in the spring 2020 than the same period in 2019. 12 The children who increased their use of asthma medicines in March 2020 had poorer asthma control than in March 2019. 12 Also, during the first wave of the pandemic, it was thought that people with moderate‐to‐severe asthma might face a higher risk of severe COVID‐19 disease, 28 and this may have increased the use of asthma medicines. Thus, the increase in the first quarter in our study may have been due to worse asthma control and the fear of severe COVID‐19 disease in early 2020. Overall, the most prominent reduction since the lockdown was in short‐acting beta‐agonists. These are used to treat acute symptoms, typically dyspnoea or wheezing, and the decrease in their use suggests that there were lower rates of asthma exacerbations and wheezing episodes in 2020 after the start of the first lockdown.
The decline in the number of dispensed medicines might have been due to the impaired capacity of primary care resources during the pandemic, rather than a real reduced need for the medicines. Secondary and tertiary care capacity remained unchanged for children during the pandemic. However, to assess this, we included primary care visit rates and found an increase in the number of visits since August 2020. Despite this, the number of dispensed items still remained lower than in the previous year. These findings suggest that the decreased number of antibiotics was due to reduced infection rates, rather than a lack of primary healthcare resources. The incidence of COVID‐19 decreased rapidly in May 2020, bringing Finland's first wave to an end, 29 and primary care visits returned to normal levels in June 2020. The restrictions were less strict during the second wave in autumn 2020, but the number of systemic antibiotics and asthma medicines remained lower than in the previous year.
4.1. Strengths and limitations
One of the strengths of this study was that the nationwide register of reimbursable prescription medicines contained all the medicines that were dispensed by pharmacies. All Finnish citizens have equal access to health care. Medicine costs are partly covered, depending on the reimbursement status of the medicine, and citizens do not need private health insurance to gain these discounts. In addition, all prescriptions that are dispensed are recorded in the register independently of the patient's insurance status or whether they were prescribed by the primary, secondary, tertiary or private sectors.
A limitation of this study was that we analysed prescriptions that were dispensed by Finnish pharmacies. We were not able to determine the indications for the prescriptions, whether there were medicines that were prescribed but not dispensed or whether the prescribed medication was used. In addition, the open‐access register did not contain information on the duration of the antibiotic treatment prescribed. The data for this study were gathered from open‐access registers due to their prompt availability and the fact that daily data will not be available until the end of the year.
5. CONCLUSION
Lockdowns and social restrictions during the first and second waves of COVID‐19 in Finland led to significant reductions in antibiotics and asthma medicines dispensed to children aged 0–12 years. In turn, this led to large reductions in reimbursement rates. The reductions in dispensing were not due to insufficient primary care resources.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
Supporting information
Appendix S1
Appendix S2
Haapanen M, Renko M, Artama M, Kuitunen I. Systemic antibiotics and asthma medicines dispensed to 0−12 year olds significantly decreased during the COVID‐19 pandemic in 2020. Acta Paediatr.2022;111:376–382. 10.1111/apa.16144
Funding information
No external funding
REFERENCES
- 1. Hatoun J, Correa ET, Donahue SMA, Vernacchio L. Social distancing for COVID‐19 and diagnoses of other infectious diseases in children. Pediatrics. 2020;146(4):e2020006460. [DOI] [PubMed] [Google Scholar]
- 2. Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen‐Kosma T, Renko M. Effect of social distancing due to the COVID‐19 pandemic on the incidence of viral respiratory tract infections in children in Finland during early 2020. Pediatr Infect Dis J. 2020;39(12):e423‐e427. [DOI] [PubMed] [Google Scholar]
- 3. Sullivan SG, Carlson S, Cheng AC, et al. Where has all the influenza gone? The impact of COVID‐19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill. 2020;25(47):2001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Angoulvant F, Ouldali N, Yang DD, et al. Coronavirus disease 2019 pandemic: Impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections‐a time series analysis. Clin Infect Dis. 2021;72(2):319‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Haapanen M, Renko M, Artama M, Kuitunen I. The impact of the lockdown and the re‐opening of schools and day cares on the epidemiology of SARS‐CoV‐2 and other respiratory infections in children – a nationwide register study in Finland. EClinicalMedicine. 2021;34:100807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kuitunen I, Haapanen M, Artama M, Renko M. Closing Finnish schools and day care centres had a greater impact on primary care than secondary care emergency department visits. Acta Paediatr. 2020;110(3):937‐938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nascimento MS, Baggio DM, Fascina LP, do Prado C. Impact of social isolation due to COVID‐19 on the seasonality of pediatric respiratory diseases. PLoS One. 2020;15(12):e0243694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nolen LD, Seeman S, Bruden D, et al. Impact of social distancing and travel restrictions on non‐COVID‐19 respiratory hospital admissions in young children in rural Alaska. Clin Infect Dis. 2020;72(12):2196‐2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bover‐Bauza C, Rosselló Gomila MA, Díaz Pérez D, et al. The impact of the SARS‐CoV‐2 pandemic on the emergency department and management of the pediatric asthmatic patient. J Asthma Allergy. 2021;14:101‐108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Krivec U, Kofol Seliger A, Tursic J. COVID‐19 lockdown dropped the rate of paediatric asthma admissions. Arch Dis Child. 2020;105(8):809‐810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sheehan WJ, Patel SJ, Margolis RHF, et al. Pediatric asthma exacerbations during the COVID‐19 pandemic: absence of the typical fall seasonal spike in Washington. DC. J Allergy Clin Immunol Pract. 2021;9(5):2073‐2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ferraro VA, Zamunaro A, Spaggiari S, Di Riso D, Zanconato S, Carraro S. Pediatric asthma control during the COVID‐19 pandemic. Immun Inflamm Dis. 2021;9(2):561‐568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Papadopoulos NG, Custovic A, Deschildre A, et al. Impact of COVID‐19 on pediatric asthma: practice adjustments and disease burden. J Allergy Clin Immunol Pract. 2020;8(8):2592‐2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gagliotti C, Buttazzi R, Ricchizzi E, Di Mario S, Tedeschi S, Moro ML. Community use of antibiotics during the COVID‐19 lockdown. Inf Dis (Lond). 2021;53(2):142‐144. [DOI] [PubMed] [Google Scholar]
- 15. Torretta S, Capaccio P, Coro I, et al. Incidental lowering of otitis‐media complaints in otitis‐prone children during COVID‐19 pandemic: not all evil comes to hurt. Eur J Pediatr. 2021;180(2):649‐652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Statistical database Kelasto . [Official website of statistical database of Kela]. https://www.kela.fi/web/en/statistical‐database‐kelasto_contents. Accessed Mar 26, 2021.
- 17. Primary health care outpatient care notification (AvoHILMO) (in Finnish) [Official website of the Finnish institute for health and welfare (THL)]. https://thl.fi/fi/tilastot‐ja‐data/ohjeet‐tietojen‐toimittamiseen/perusterveydenhuollon‐avohoidon‐hoitoilmoitus‐avohilmo. Accessed Apr 12, 2021.
- 18. Outpatient care in primary health care (in Finnish) [Official website of the Finnish institute for health and welfare (THL)]. https://thl.fi/fi/tilastot‐ja‐data/aineistot‐ja‐palvelut/tilastojen‐laatu‐ja‐periaatteet/laatuselosteet/perusterveydenhuolto. Accessed May 16, 2021.
- 19. Statistics Finland’s online service . [Official website of the statistics Finland]. http://pxnet2.stat.fi/PXWeb/pxweb/en/StatFin/Accessed. Accessed Jan 17, 2021.
- 20. Nieuwlaat R, Mbuagbaw L, Mertz D, et al. Coronavirus disease 2019 and antimicrobial resistance: parallel and interacting health emergencies. Clin Infect Dis. 2021;72(9):1657‐1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lai C, Chen S, Ko W, Hsueh P. Increased antimicrobial resistance during the COVID‐19 pandemic. Int J Antimicrob Agents. 2021;57(4):106324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bradley JS, Byington CL, Shah SS, et al. Executive summary: the management of community‐acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the pediatric infectious diseases society and the infectious diseases society of America. Clin Infect Dis. 2011;53(7):617‐630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Donovan BM, Abreo A, Ding T, et al. Dose, timing, and type of infant antibiotic use and the risk of childhood asthma. Clin Infect Dis. 2020;70(8):1658‐1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Patrick DM, Sbihi H, Dai DLY, et al. Decreasing antibiotic use, the gut microbiota, and asthma incidence in children: evidence from population‐based and prospective cohort studies. Lancet Respir Med. 2020;8(11):1094‐1105. [DOI] [PubMed] [Google Scholar]
- 25. Bailey LC, Forrest CB, Zhang P, Richards TM, Livshits A, DeRusso PA. Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr. 2014;168(11):1063‐1069. [DOI] [PubMed] [Google Scholar]
- 26. Aghaali M, Hashemi‐Nazari SS. Association between early antibiotic exposure and risk of childhood weight gain and obesity: a systematic review and meta‐analysis. J Pediatr Endocrinol Metab. 2019;32(5):439‐445. [DOI] [PubMed] [Google Scholar]
- 27. Antonsen J, Hansen S, Morgen CS, Jess T, Jorgensen LN, Allin KH. Antibiotics during childhood and development of appendicitis—a nationwide cohort study. Aliment Pharmacol Ther. 2021;53(1):87‐93. [DOI] [PubMed] [Google Scholar]
- 28. Coronavirus disease 2019 (COVID‐19) . [Official website of the Centers for disease control and prevention]. https://www.cdc.gov/coronavirus/2019‐ncov/need‐extra‐precautions/asthma.html. Accessed May 6, 2021
- 29. Coronavirus Research Center . [Official website of the john hopkins university & medicine]. https://coronavirus.jhu.edu/region. Accessed 23 May, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Appendix S2


