FIGURE 1.
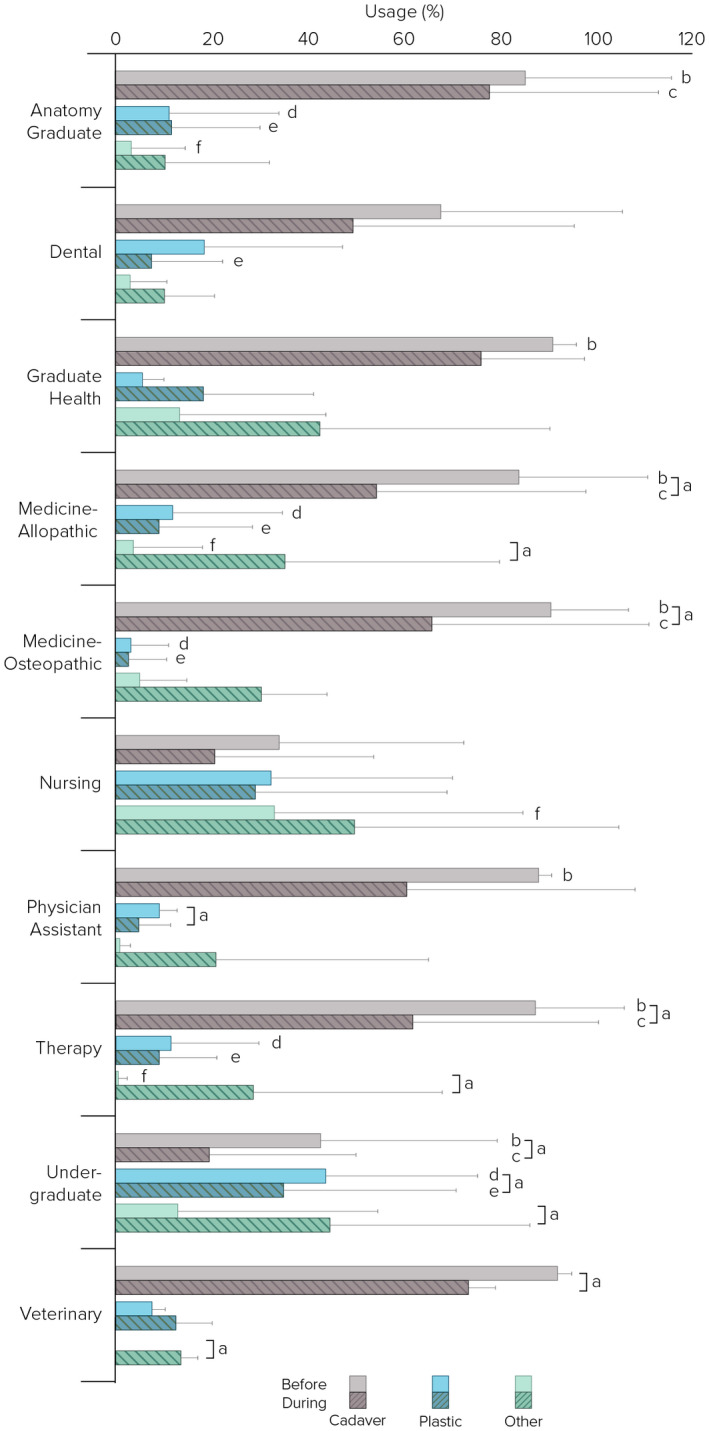
Percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 pandemic (August–December 2020) by academic program (n = 190; anatomy graduate, n = 19; dental, n = 11; graduate health, n = 6; allopathic medicine, n = 71; osteopathic medicine, n = 11; nursing, n = 6; physician assistant, n = 6; therapy, n = 17; undergraduate n = 40; veterinary, n = 3). Cadaver includes dissection and prosection; plastic includes plastic models and plastinated specimens. aPercent time using cadaver, plastic, and “other” were significantly different before and during Covid‐19 (P ≤ 0.045); bPercent time using cadavers was significantly different across programs before Covid‐19 (Kruskal–Wallis test H, P < 0.0001). Dunn's post hoc analysis showed that cadaver usage was significantly less in the undergraduate versus anatomy graduate (P = 0.001), allopathic (P < 0.0001) and osteopathic (P < 0.0001) medicine, physician assistant (P = 0.019), therapy (P < 0.0001), and graduate health (P = 0.047) programs. Similarly, cadaver usage was significantly less in the nursing versus anatomy graduate (P = 0.010), allopathic (P = 0.004) and osteopathic (P = 0.007) medicine, and therapy (P = 0.008) programs; cPercent time using cadavers was significantly different across programs during Covid‐19 (Kruskal–Wallis test H, P < 0.0001). Dunn's analysis showed that cadaver usage was significantly less in the undergraduate versus anatomy graduate (P < 0.0001), allopathic (P = 0.001) osteopathic (P = 0.027) medicine, and therapy (P = 0.016) programs; dPercent time using plastics was significantly different across programs before Covid‐19 (Kruskal–Wallis test H, P < 0.0001). Dunn's analysis showed that plastics usage was significantly greater in the undergraduate versus anatomy graduate (P < 0.0001), allopathic (P < 0.0001) and osteopathic (P < 0.0001) medicine, and therapy (P < 0.0001) programs; ePercent time using plastics was significantly different across programs during Covid‐19 (Kruskal–Wallis test H, P < 0.0001). Dunn's analysis showed that cadaver usage was significantly less in the undergraduate versus anatomy graduate (P = 0.017), dental (P = 0.026), allopathic (P < 0.0001) and osteopathic (P < 0.003) medicine, and therapy (P = 0.010) programs; fPercent time using “other” was significantly different across programs before Covid‐19 (Kruskal–Wallis test H, P = 0.006). Dunn's analysis showed that cadaver usage was significantly greater in the nursing versus anatomy graduate (P = 0.018), allopathic medicine (P = 0.006), and therapy (P = 0.010) programs
