This cohort study evaluates the predictive utility of adding former smoking status, pack-years smoked, and years since quitting to the American College of Cardiology/American Heart Association 2013 pooled cohort equations for more accurate atherosclerotic cardiovascular disease risk prediction.
Key Points
Question
Does modification of the 2013 pooled cohort equations to include former smoking status, pack-years, and years since quitting smoking improve atherosclerotic cardiovascular disease (ASCVD) risk prediction?
Findings
In this cohort study of 3908 individuals, including these smoking variables in the 2013 pooled cohort equations improves ASCVD risk prediction in White individuals. Overall, 14% of men and 15% of women who developed ASCVD were reclassified into higher risk groups compared with the base model; this would translate to the correct reclassification of ASCVD risk in nearly 3 million individuals in the US.
Meaning
If results are replicated in cohorts of race and ethnicity groups other than non-Hispanic White, these factors could be considered for inclusion in clinical ASCVD risk prediction tools.
Abstract
Importance
Former heavy smokers (ie, those with ≥20 pack-years of smoking) may have higher atherosclerotic cardiovascular disease (ASCVD) risk than never smokers for up to 16 years after smoking cessation. However, the 2013 pooled cohort equations (PCE) do not account for pack-years of smoking and only consider current vs noncurrent smoking status without distinguishing former smokers from never smokers.
Objective
To assess the predictive utility of smoking history when added to the PCE using data from 18 400 person examinations among Framingham offspring participants.
Design, Setting, and Participants
This is a retrospective analysis of prospectively collected data from the Framingham Heart Study, a community-based cohort. Framingham Heart Study offspring cohort participants attending their first examination (1971-1975) who were followed-up through December 2016 were included.
Exposures
Self-reported current/former/never smoking status, pack-years smoked, and years since quitting.
Main Outcomes and Measures
Incident ASCVD (myocardial infarction, fatal/nonfatal ischemic stroke, coronary heart disease death).
Results
Of 3908 patients, there were 358 and 197 events among 1895 men and 2013 women, respectively, with a mean (SD) age of 55 (9.5) years. Ever smoking prevalence was high (6474 men [77%] and 7760 women [78%]), as were median pack-years (men: 39; women: 32 overall person examinations). Four sex-specific ASCVD risk prediction models were built using pooled-repeated Cox proportional hazards regression. The PCEs were was fit in this sample with continuous predictors on their natural scale (ie, not logarithmically transformed) as well as polynomials accounting for nonlinearity and then cumulatively adjusted for former smoking, pack-years, and years since quitting. Models were compared via change in C statistic, continuous net reclassification improvement (NRI[>0]), and relative integrated discrimination improvement (rIDI). Including former smoking status, pack-years, and years since quitting had significant but modest NRI(>0) and rIDI values compared with the PCE with continuous variables on their natural scale in both sexes (men: NRI[>0] = 0.23; rIDI = 0.19; women: NRI[>0] = 0.34, rIDI = 0.11; change in C statistic = 0.01 for both).
Conclusions and Relevance
Former smoking, pack-years, and years since quitting significantly improved ASCVD risk prediction in this sample. The Framingham Heart Study offspring cohort is largely composed of non-Hispanic White participants of European ancestry. If results are validated in cohorts of race and ethnicity groups other than White, these variables could be considered for inclusion in future ASCVD risk prediction models.
Introduction
The cornerstone of atherosclerotic cardiovascular disease (ASCVD) prevention is assessing risk prior to an event and implementing lifestyle and drug interventions accordingly; the current criterion standard risk assessment tool is the ASCVD Risk Estimator Plus.1,2 This calculator considers former smokers, for the first 5 years after cessation, to be at excess ASCVD risk compared with never smokers and does not incorporate pack-years smoked. However, we recently demonstrated that excess ASCVD risk among former heavy (≥20 pack-years) smokers vs never smokers can remain for up to 16 years postcessation.3 Thus, years since quitting (YSQ) and pack-years smoked may play an important role in ASCVD risk estimation.
The ASCVD Risk Estimator Plus is based on the 2013 American College of Cardiology/American Heart Association Guideline on the Assessment of Cardiovascular Risk and its corresponding sex- and race-specific pooled cohort equations (2013 PCE) for estimation of 10-year ASCVD risk.4 The 2013 PCE were developed to expand on prior cardiovascular disease risk prediction equations5,6,7 in a racially and geographically diverse sample.4 Although up to 25% of ASCVD deaths are attributable to cigarette smoking,8,9 former smoking status, pack-years smoked, and YSQ were not considered for inclusion owing to lack of available data in all cohorts used to develop the 2013 PCE. There are currently more than 55 million individuals in the US who have quit smoking10; this number grows as smoking cessation increases.11 Furthermore, the 2015 National Health Interview Survey estimates that 29% of former and 33% of current smokers have accumulated at least 20 pack-years smoked.12 Because ASCVD risk increases with greater pack-years smoked and decreases with sustained cessation,3 ASCVD risk may be misestimated in individuals who have ever smoked heavily.
In this context, we fit a series of ASCVD risk prediction models using Framingham Heart Study (FHS) data. By assessing a variety of model fit metrics spanning goodness of fit, discrimination, calibration, and reclassification, we evaluated the predictive utility of adding former smoking status, pack-years smoked, and YSQ to the 2013 PCE for more accurate ASCVD risk prediction.
Methods
Study Sample
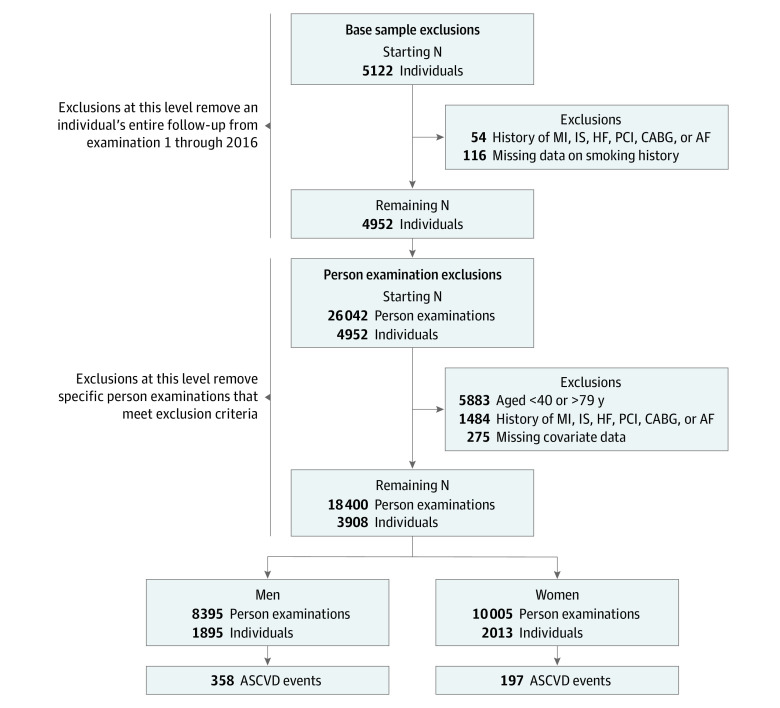
This investigation included more than 40 years of data on FHS offspring13 cohort participants attending their first (1971-1975) examination cycle with at least 1 subsequent contact with study staff. Participants presented for quadrennial examination cycles beginning in 1979 (up to 8 examination cycles in this analysis). Each person examination and the ensuing 10 years served as an independent ASCVD risk prediction window, yielding up to 8 data records per individual (eFigure 1 in the Supplement).
The analysis data set was constructed in 2 phases. First, we excluded participants from the base sample if, at examination 1, they had a history of myocardial infarction (MI), ischemic stroke (IS), heart failure (HF), coronary artery bypass graft (CABG), percutaneous coronary intervention (PCI), or atrial fibrillation (AF) or were missing data that would prevent us from quantifying lifetime smoking history. In the second phase of data set construction, we applied exclusion criteria at the person examination level since these served as individual baselines for 10-year ASCVD risk prediction. Person examinations were excluded for the following reasons: age younger than 40 years or older than 79 years; history of MI, IS, HF, CABG, PCI, or AF; or missing data on predictors. Following exclusions, our final sample for analysis contained 18 400 person examinations on 3908 individuals (Figure). This study was approved by institutional review boards at Boston University Medical Center, Vanderbilt University Medical Center, and University of Kentucky; FHS participants provided written informed consent.
Figure. Sample Flow Diagram.
Construction of the analysis data set from the starting sample. AF indicates atrial fibrillation; ASCVD, atherosclerotic cardiovascular disease; CABG, coronary artery bypass graft; HF, heart failure; IS, ischemic stroke; MI, myocardial infarction, PCI, percutaneous coronary intervention.
Outcome
FHS participants are under continuous surveillance for development of ASCVD events. In this investigation, participants were surveilled until December 31, 2016, for development of ASCVD events including MI, fatal or nonfatal IS, and coronary heart disease death. For suspected ASCVD events, medical records were obtained with permission; events were adjudicated by 3 physicians as previously detailed.3,14,15,16
ASCVD Risk Factor Definitions
Our risk factor definitions were the same as those in the sex-specific 2013 PCE4 models (age, total cholesterol, high-density lipoprotein [HDL] cholesterol, systolic blood pressure [SBP], antihypertensive use, current smoking status, and diabetes). Statin therapy was not included in the development of the 2013 PCE, so we did not include it either to facilitate direct comparison. Further risk factor definitions are provided in the eMethods in the Supplement.
Quantification of Smoking Status and Intensity
At baseline examination, participants were categorized as current, former, or never smokers based on their responses to questions regarding current and prior smoking habits. From responses given for age at which the participant starting smoking, usual cigarettes smoked per day in the past, age at quitting (former smokers), and current number of cigarettes smoked per day (current smokers), we calculated ever smokers’ pack-years and former smokers’ YSQ. For this analysis, our smoking measures included 3-level (current/former/never) smoking status, pack-years, and YSQ. Additional details are provided in the eMethods in the Supplement.
Statistical Analysis
Summary statistics were stratified by sex; within sex, statistics were pooled over all person examinations. We calculated means and standard deviations for normally distributed variables and medians along with the interquartile range for variables with skewed distributions. Counts and percentages were calculated for categorical variables.
We performed a series of sex-specific pooled repeated Cox proportional hazards regressions to predict ASCVD incidence.17,18 In all models, the Huber-White sandwich covariance estimator19,20 was used to account for correlation among repeated observations in the same individuals with overlapping follow-up intervals; this methodology is consistent with prior investigations of overlapping follow-up intervals.21
We first fit sex-specific models, which were similar to the 2013 PCE but with 3 changes: (1) inclusion of continuous variables on their natural scale (ie, not logarithmically transformed); (2) up to third-order polynomials on continuous variables (and their interactions) to account for nonlinearity; and (3) adjustment for antihypertensive use and measured SBP rather than including separate terms for treated/untreated SBP. Reasons for these alterations, as well as the polynomial terms on continuous variables, are provided in the eMethods in the Supplement. This reference model included age, total cholesterol, HDL cholesterol, SBP, antihypertensive use, current smoking status, and diabetes status as risk factors; total cholesterol, HDL cholesterol, and current smoking status interacted with age and antihypertensive use interacted with SBP. Subsequent models cumulatively adjusted for former smoking status, pack-years smoked, and YSQ; each of these smoking variables interacted with age.
To determine whether former smoking status, pack-years smoked, and/or YSQ should be added to the 2013 PCE, we evaluated whether these variables possess incremental value and clinical utility.22 We assessed incremental value via change in Harrell C statistic23 and continuous net reclassification improvement (NRI[>0]).24,25,26,27 In the setting of risk prediction, clinical utility of a variable refers to its ability to sufficiently move an individual across the risk spectrum when added to a model22; we quantified clinical utility using the relative integrated discrimination improvement (rIDI).27 rIDI is considered clinically meaningful when it is larger than 1/p where p is the number of degrees of freedom in the reference model.27 Since our reference model included 23 degrees of freedom, an rIDI more than 0.043 was considered clinically meaningful. Statistical significance of all 3 metrics was evaluated via bootstrapped 95% CIs. Since models must be well calibrated to assess NRI(>0) and rIDI, we also calculated the D’Agostino and Nam extension of the Hosmer-Lemeshow calibration test.28
To visually assess risk reclassification, we created reclassification plots for each model under consideration. To be thorough in our assessment of former smoking status, pack-years, and YSQ, we evaluated goodness of fit via likelihood ratio and Nagelkerke R2.29,30
Secondary analyses examined the predictive ability of smoking variables compared with other ASCVD risk factors included in the PCE. In these analyses, we fit 4 models in each sex: 1 for each group of risk factors (lipids [total and HDL cholesterol], blood pressure [SBP and antihypertensive use], diabetes [indicator of fasting plasma glucose >126 mg/dL (to convert to millimoles per liter, multiply by 0.0555) or usage of antidiabetic medications], and smoking [3-level smoking status, pack-years, and YSQ]); each model also included age and any interactions with age included in our final model. The predictive ability was quantified by Harrell C statistic and Nagelkerke R2.
Exploratory analyses compared risk category classification under the 2013 PCE vs our final model (model with 2013 PCE variables plus former smoking, pack-years, and YSQ) in events and nonevents separately within each sex. Categories were defined as low, borderline, intermediate, and high using the same cutoffs described above to maintain consistency with the 2013 PCE1,4 and also by deciles of risk to provide more detailed results. We then used the number of current and former US smokers10,31 in conjunction with the proportion of ever smokers with 20 or more pack-years estimated by the National Health Interview Survey12 and our reclassification results to estimate the number of US heavy ever smokers who would be correctly reclassified under our final model compared with the 2013 PCE.
Finally, we performed a preliminary validation analysis to determine whether our results would replicate in a contemporary sample with lower smoking prevalence. Using the same inclusion/exclusion criteria as the derivation sample, we pooled data from the first (2002-2005) and second (2008-2011) examinations of the FHS generation 3 cohort32 with that from the ninth examination of the FHS offspring cohort (2011-2014). All models were refit in this validation sample to determine whether model form, rather than the estimated effect sizes, improved ASCVD risk prediction.
Approximately 1% of person examinations were missing covariate data. Since the proportion of missingness was small, we assumed that values were missing completely at random. Under this assumption, a complete case analysis would not bias our results. A 2-sided P value less than .05 was considered statistically significant. All analyses were performed in SAS statistical software version 9.4 (SAS Institute). Analysis took place from October 2019 to September 2021.
Results
We analyzed data from 18 400 person examinations on 3908 individuals (8395 person examinations on 1895 men [48.5%] and 10 005 person examinations on 2013 women [51.5%]). Most characteristics were similar between men and women (Table 1). Nearly a quarter of the sample were never smokers, but more men were former smokers (3790 [45%]) than women (3573 [36%]). Correspondingly, a larger proportion of women than men were current smokers (4187 women [42%] and 2684 men [32%]). However, men who had ever smoked tended to smoke more heavily than their female counterparts (Table 1).
Table 1. Sample Characteristics by Sex Over All Person Examinations.
| Characteristic | Men (n = 8395) | Women (n = 10 005) |
|---|---|---|
| Age, mean (SD), y | 54.8 (9.4) | 55.5 (9.6) |
| Systolic blood pressure, mean (SD), mm Hg | 129.0 (16.8) | 125.5 (18.6) |
| Antihypertensive medication, No. (%) | 1864 (22.2) | 2068 (20.7) |
| Diabetes, No. (%) | 643 (7.7) | 495 (5.0) |
| Cholesterol, mean (SD), mg/dL | ||
| Total | 206.1 (38.4) | 211.2 (38.9) |
| HDL | 44.7 (12.8) | 58.4 (16.4) |
| Lipid-lowering medication use, No. (%) | 752 (9.0) | 834 (8.3) |
| Smoking status, No. (%) | ||
| Current | 2684 (32.0) | 4187 (41.9) |
| Former | 3790 (45.2) | 3573 (35.7) |
| Never | 1921 (22.9) | 2245 (22.4) |
| Cigarettes/d, median (IQR)a | 20.0 (20.0-30.0) | 20.0 (10.0-30.0) |
| Cumulative pack-years, median (IQR) | ||
| Current | 39.1 (27.2-55.3) | 32.0 (19.2-46.6) |
| Former | 22.0 (10.0-37.5) | 11.0 (4.4-23.4) |
| Years since quitting, median (IQR)b | 16.1 (8.5-25.4) | 15.5 (8.1-24.5) |
Abbreviation: HDL, high-density lipoprotein.
SI conversion factor: To convert cholesterol to millimoles per liter, multiply by 0.0259.
Among current smokers only.
Among former smokers only.
Throughout a total of 169 484 person-years, 555 incident ASCVD events occurred: 358 (64.5%) in men and 197 (35.5%) in women. Results of the model fitting procedure in men and women are displayed in Table 2. All models were well calibrated (Table 2; eFigures 2-5 in the Supplement).
Table 2. Model Summaries.
| Model No. | Description | −2 Log likelihood | df | Δdf | LR χ2 | P value for LR | R2, % | Calibration χ2 | P value for calibration | C statistic | Δ Harrell c (95% CI) | NRI(>0) (95% CI) | Relative IDI (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | |||||||||||||
| 1 | Model with 2013 PCE variablesa | 6110.53 | 23 | NA | NA | NA | 6.77 | 6.97 | .07 | 0.7538 | NA | NA | NA |
| 2 | Model 1 + former smoking | 6101.89 | 26 | 3 | 8.64 | .02 | 6.96 | 3.62 | .31 | 0.7559 | 0.002 (−0.002 to 0.006) | 0.145 (0.042 to 0.254) | 0.047 (0.021 to 0.075) |
| 3 | Model 2 + pack-years | 6086.75 | 31 | 8 | 23.78 | .002 | 7.27 | 2.72 | .44 | 0.7596 | 0.006 (0.001 to 0.011) | 0.259 (0.156 to 0.358) | 0.175 (0.092 to 0.271) |
| 4 | Model 3 + YSQ | 6084.36 | 36 | 13 | 26.17 | .02 | 7.32 | 3.03 | .39 | 0.7604 | 0.007 (0.001 to 0.120) | 0.233 (0.132 to 0.332) | 0.191 (0.096 to 0.295) |
| Women | |||||||||||||
| 1 | Model with 2013 PCE variablesa | 3326.30 | 23 | NA | NA | NA | 9.31 | 2.93 | .40 | 0.8123 | NA | NA | NA |
| 2 | Model 1 + former smoking | 3323.39 | 26 | 3 | 2.91 | .16 | 9.41 | 2.20 | .53 | 0.8133 | 0.001 (−0.002 to 0.004) | 0.163 (0.020 to 0.303) | 0.026 (−0.001 to 0.053) |
| 3 | Model 2 + pack-years | 3310.79 | 31 | 8 | 15.51 | .02 | 9.80 | 5.74 | .13 | 0.8179 | 0.006 (−0.003 to 0.014) | 0.287 (0.148 to 0.424) | 0.098 (0.046 to 0.165) |
| 4 | Model 3 + YSQ | 3306.88 | 36 | 13 | 19.42 | .11 | 9.92 | 3.07 | .38 | 0.8195 | 0.007 (−0.002 to 0.017) | 0.340 (0.204 to 0.478) | 0.112 (0.052 to 0.185) |
Abbreviations: IDI, integrated discrimination improvement; LR, likelihood ratio; NA, not applicable; NRI(>0), continuous net reclassification improvement; PCE, pooled cohort equations; YSQ, years since quitting smoking.
This is the reference for models 2-4 when calculating the likelihood ratio test, Δ Harrell C statistic, NRI(>0), and relative IDI.
Model Fitting in Men
We began by fitting the reference model with 2013 PCE variables and then added an indicator of former smoking status. This change improved goodness of fit (likelihood ratio and R2) and clinical utility (rIDI), but NRI(>0) was small, and change in Harrell C statistic was not statistically significant. Further adjustment for pack-years proved significant on all metrics, producing a clinically meaningful rIDI and a moderate NRI(>0). Addition of YSQ was also significant on all metrics (Table 2).
Overall, the model with 2013 PCE variables with additional adjustment for former smoking, pack-years, and YSQ (our final model) was the best fit to the data, featuring the highest likelihood, R2, and Harrell C statistic; moderate NRI(>0); and a statistically significant and clinically meaningful rIDI. Compared with the reference model with 2013 PCE variables, change in predicted probability of 10-year ASCVD incidence was greatest on addition of all 3 smoking variables as shown in eFigure 6 in the Supplement.
Model Fitting in Women
Model fitting in women progressed as in men (Table 2). Adding an indicator of former smoking status did not improve model fit. Addition of pack-years smoked improved goodness of fit, produced a moderate NRI(>0) and a clinically meaningful rIDI but did not improve the C statistic. When YSQ was added, the likelihood ratio test and change in Harrell C statistic were not significant, but R2 increased, the NRI(>0) was moderate, and rIDI was both statistically significant and clinically meaningful (Table 2). Compared with the reference model with 2013 PCE variables, change in predicted probability of 10-year ASCVD incidence was greatest on addition of all 3 smoking variables, but the change was less pronounced than in men (eFigure 7 in the Supplement).
Secondary Analyses: Predictive Ability of Smoking Variables Compared With Other Risk Factors
In men and women, models that included age, smoking variables, and their interactions produced the highest Harrell C statistic and Nagelkerke R2 compared with models with age and lipids, blood pressure, or diabetes alone (Table 3).
Table 3. Comparison of Atherosclerotic Cardiovascular Disease Risk Factors.
| Risk factora | Men | Women | ||
|---|---|---|---|---|
| C statistic | R2, % | C statistic | R2, % | |
| Lipids (total and HDL cholesterol) | 0.6718 | 3.12 | 0.7578 | 6.37 |
| Blood pressure (SBP and antihypertensive use) | 0.6622 | 2.70 | 0.7663 | 6.56 |
| Diabetes (indicator of FPG >126 mg/dL, medication use) | 0.6470 | 2.58 | 0.7411 | 5.84 |
| Smoking (3-level status, pack-years, years since quitting) | 0.7111 | 4.78 | 0.7794 | 7.38 |
Abbreviations: HDL, high-density lipoprotein; FPG, fasting plasma glucose; SBP, systolic blood pressure.
Each risk factor was included in a model alone with age and any relevant interactions with age as they are currently included in our final model.
Exploratory Analyses: Reclassification Tables
The majority of individuals remained in the same risk category under the PCE and our final model (Table 4). Among men, similar proportions of nonevents were correctly reclassified at lower risk (570 [7.1%]) and incorrectly reclassified as higher risk (485 [6.0%]) under our final model compared with the PCE (Table 4). However, 14% of men (n = 50) who experienced ASCVD events within 10 years were classified as higher risk under our final model compared with the PCE while only 6.7% (n = 24) were incorrectly reclassified into a lower-risk category (Table 4). Although the proportion of women who were reclassified under our final model compared with the PCE was different than in men, the trend was similar (Table 4). Reclassification results in individuals who ever heavily smoked were similar to those of the full sample (eTables 1 and 2 in the Supplement). Using the number of former and current US smokers10,31 and the proportion of these ever smokers with at least 20 pack-years from the 2015 National Health Interview Survey,12 we estimate that approximately 3 million individuals in the US with 20 or more pack-years smoked would be correctly reclassified under models capturing details of smoking exposure compared with the 2013 PCE.
Table 4. Reclassification of Risk Under 2013 PCE vs Final Model With Former Smoking Status, Pack-Years, and Years Since Quittinga.
| Variable | Noneventsb | Eventsc | ||||||
|---|---|---|---|---|---|---|---|---|
| <5% | 5%-7.49% | 7.5%-19.9% | ≥20% | <5% | 5%-7.49% | 7.5%-19.9% | ≥20% | |
| 2013 PCEd | ||||||||
| Men | ||||||||
| <5% | 5245e | 178f | 4f | 0f | 105e | 10g | 3g | 0g |
| 5%-7.49% | 320g | 713e | 238f | 2f | 6f | 39e | 22g | 0g |
| 7.5%-19.9% | 30g | 181g | 958e | 63f | 2f | 14f | 124e | 15g |
| ≥20% | 4g | 3g | 32g | 58f | 0f | 0f | 2f | 16e |
| Women | ||||||||
| <5% | 8708e | 146f | 31f | 0f | 97e | 6g | 5g | 0g |
| 5%-7.49% | 167g | 174e | 82f | 2f | 7f | 11e | 13g | 0g |
| 7.5%-19.9% | 9g | 86g | 312e | 25f | 0f | 4f | 40e | 7g |
| ≥20% | 0g | 0g | 19g | 39e | 0f | 0f | 1f | 6e |
Abbreviation: PCE, pooled cohort equations.
Predicted risk under 2013 PCE in rows; predicted risk under final model (model 4) in columns.
Fifty men and 31 women did not experience atherosclerotic cardiovascular disease (ASCVD) and were correctly reclassified into a lower category. Twenty-four men and 12 women did not experience ASCVD and were incorrectly classified into a higher-risk category. Two hundred eighty-four men and 154 women did not experience ASCVD and were not reclassified.
Five hundred seventy men and 281 women did not experience ASCVD and were correctly reclassified into a lower category. Four hundred eighty-five men and 286 women did not experience ASCVD and were incorrectly classified into a higher-risk category. Six thousand nine hundred seventy-four men and 9233 women did not experience ASCVD and were not reclassified.
2013 PCE with baseline hazard and coefficients re-estimated in the current sample for fair model comparison. Otherwise, results would appear artificially favorable since the model with 2013 PCE variables plus 3-level smoking status, pack-years, and years since quitting was developed entirely in this sample and would necessarily outperform the 2013 PCE, which were developed in an external sample.
No reclassification.
Movement in the incorrect direction (higher risk for nonevents, lower risk for events).
Movement in the correct direction (lower risk for nonevents, higher risk for events).
Validation Results
Our validation sample included 1905 men (44.4%; 2715 person examinations, 91 incident ASCVDs) and 2388 women (55.6%; 3318 person examinations, 47 incident ASCVDs). In this sample, 2159 (50%) were never smokers, 1615 (38%) were former smokers, and 519 (12%) were current smokers at their baseline examination. For men, results were similar to those observed in the derivation cohort: the Nagelkerke R2 improved, C statistic increased (although not significantly), NRI(>0) was moderate, and rIDI was clinically meaningful when adding former smoking status, pack-years, and YSQ to the reference model with 2013 PCE variables (eTable 3 in the Supplement). In women, results roughly followed a similar pattern as men, but the estimates had wide confidence intervals yielding only a clinically meaningful rIDI (eTable 3 in the Supplement).
Discussion
Inclusion of former smoking status, pack-years, and YSQ improved ASCVD risk prediction over the reference model with 2013 PCE variables. Specifically, adding these variables produced moderate NRI(>0) values of 0.23 and 0.34 in men and women, respectively, and clinically meaningful rIDI values of 0.19 and 0.11 in men and women, respectively. Furthermore, when included in a model with age, smoking variables produced a higher Harrell C statistic and Nagelkerke R2 than lipids, blood pressure, or diabetes, and their inclusion could correctly reclassify the ASCVD risk of as many as 3 million individuals in the US who have ever heavily smoked.
To our knowledge, this is the first investigation to demonstrate that pack-years and YSQ improve ASCVD risk prediction vs current tools. These findings are consistent with earlier work demonstrating that cardiovascular disease risk of those who formerly heavily smoked (>20 pack-years) compared with those who never smoked remains significantly elevated beyond 5 years after smoking cessation.3 These findings also build on the work by Lloyd-Jones et al,1,2 which distinguished risk between former and never smokers during the first 5 years of cessation.2 Here, we extended the time for which former smokers are at elevated risk compared with never smokers and incorporated pack-years. The inclusion of both pack-years smoked and YSQ in ASCVD risk estimation is necessary because they contribute different information: pack-years distinguish risk among ever smokers, while former smokers’ YSQ quantifies the amount of ASCVD risk attributable to smoking remaining at a given assessment. Results from our preliminary validation analysis demonstrate consistency of our findings in men in a contemporary cohort; this was not the case among women, but our final model contained many predictors and few events, so this model was likely underpowered and overfit.
These findings have important implications for patients and health care professionals. As of 2018, there were 55 million former smokers and 34.2 million current smokers in the United States.10,31 Our prior work demonstrates that those who ever heavily smoked carry excess ASCVD risk that is not currently captured with quantitative risk assessment tools, which only consider current and noncurrent smoking status.3 Reclassification tables in the current analysis show that including more comprehensive smoking history in risk estimation could correctly reclassify ASCVD risk for nearly 3 million individuals in the US with 20 or more pack-years smoked compared with the 2013 PCE. On an individual level, more accurate risk prediction may motivate smokers to quit smoking or encourage former smokers to discuss additional ways to lower their ASCVD risk with their health care professional. For clinicians, creating a more accurate risk prediction tool may identify high-risk patients requiring additional attention such as monitoring, or even early detection for ASCVD, akin to lung cancer screening in high-risk current and former smokers.33
Strengths and Limitations
The current investigation possesses several strengths, including FHS offspring cohort data, which spans 45 years. Furthermore, FHS participants are under continuous surveillance for ASCVD development, allowing near-complete event ascertainment. The regular assessment of these individuals enabled us to update smoking status, pack-years, and YSQ throughout follow-up to accurately reflect the added value of these predictors on ASCVD risk prediction. Finally, rather than relying on 1 method, we assessed various facets of model prediction including goodness of fit, discrimination, and calibration.
Although the data source is a strength of this investigation, the FHS offspring cohort is community-based and smoking patterns (notably the high proportion of current smokers) and sociodemographics of participants may not reflect those of the US population. However, our results remained consistent among men in a contemporary cohort in which more than 50% of participants were never smokers and 11% were current smokers. Furthermore, evidence suggests that while the design and composition of cigarettes (eg, ventilated filters, higher levels of tobacco-specific nitrosamines in smoke) have changed over time, and prevalence of smoking has decreased, the effect of smoking on cardiovascular health outcomes has remained relatively stable.8 In addition, FHS offspring cohort participants are almost exclusively middle class White individuals of European ancestry (>99% non-Hispanic White), limiting generalizability. However, cigarette smoking is more prevalent and cessation rates are lower in low socioeconomic groups compared with higher ones34,35,36; current ASCVD risk assessment tools also tend to underestimate risk in these individuals.37,38 Thus, including pack-years smoked in ASCVD risk calculators may help minimize this underestimation. For these reasons, future research should validate these findings in a large, contemporary, and sociodemographically diverse sample. Finally, our model expansions did not markedly increase the C statistic. However, comparison of 2 C statistics via change in Harrell C statistic is a low-power procedure when many observations are censored.39
Conclusions
In the FHS offspring cohort, including former smoking status, pack-years smoked, and YSQ improved ASCVD risk prediction, 15% of women and 14% of men who experienced ASCVD events in our sample were classified into a higher-risk group under our model compared with the 2013 PCE. Furthermore, smoking variables discriminated ASCVD risk better than lipids, blood pressure, or diabetes. The number of former smokers is growing, and such individuals remain at excess ASCVD risk compared with never smokers for up to 16 years after quitting. If validated in individuals of other races and ethnicities and socioeconomic groups, modification of the PCEs to include these variables could mitigate underestimation of risk among current and former smokers.
eMethods.
eFigure 1. Timeline for FHS Offspring Examinations
eFigure 2. Calibration Plots in Men: Observed Probability (y-axis) vs. Predicted Probability (x-axis)
eFigure 3. Calibration Plots in Women: Observed Probability (y-axis) vs. Predicted Probability (x-axis)
eFigure 4. Observed vs. Predicted Plots in Men by Deciles: Observed Probability (y-axis) vs. Predicted Probability (x-axis)
eFigure 5. Observed vs. Predicted Plots in Women by Deciles: Observed Probability (y-axis) vs. Predicted Probability (x-axis)
eFigure 6. Predicted Probability of ASCVD in Men: Models with Additional Smoking Data (y-axis) vs. Reference Model with 2013 PCE Variables (x-axis)
eFigure 7. Predicted Probability of ASCVD in Women: Models with Additional Smoking Data (y-axis) vs. Reference Model with 2013 PCE Variables (x-axis)
eTable 1. Reclassification of Risk in Heavy Ever Smoking (>20 Pack-Years) Men
eTable 2. Reclassification of Risk in Heavy Ever Smoking (>20 Pack-Years) Women
eTable 3. Validation Sample Model Results
References
- 1.Lloyd-Jones DM, Huffman MD, Karmali KN, et al. Estimating longitudinal risks and benefits from cardiovascular preventive therapies among medicare patients: the Million Hearts Longitudinal ASCVD Risk Assessment Tool: a special report from the American Heart Association and American College of Cardiology. Circulation. 2017;135(13):e793-e813. doi: 10.1161/CIR.0000000000000467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American College of Cardiology. ASCVD risk estimator plus. Accessed March 10, 2020. https://tools.acc.org/ASCVD-Risk-Estimator-Plus/#!/calculate/estimate/
- 3.Duncan MS, Freiberg MS, Greevy RA Jr, Kundu S, Vasan RS, Tindle HA. Association of smoking cessation with subsequent risk of cardiovascular disease. JAMA. 2019;322(7):642-650. doi: 10.1001/jama.2019.10298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guideline. J Am Coll Cardiol. 2014;63(25 pt B):2935-2959. doi: 10.1016/j.jacc.2013.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson KM, Odell PM, Wilson PWF, Kannel WB. Cardiovascular disease risk profiles. Am Heart J. 1991;121(1 pt 2):293-298. doi: 10.1016/0002-8703(91)90861-B [DOI] [PubMed] [Google Scholar]
- 6.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) . Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106(25):3143-3421. doi: 10.1161/circ.106.25.3143 [DOI] [PubMed] [Google Scholar]
- 7.D’Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743-753. doi: 10.1161/CIRCULATIONAHA.107.699579 [DOI] [PubMed] [Google Scholar]
- 8.Navar AM, Peterson ED, Wojdyla D, et al. Temporal changes in the association between modifiable risk factors and coronary heart disease incidence. JAMA. 2016;316(19):2041-2043. doi: 10.1001/jama.2016.13614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Centers for Disease Control and Prevention; 2014. [PubMed] [Google Scholar]
- 10.Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults: United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(45):1013-1019. doi: 10.15585/mmwr.mm6845a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jamal A, Phillips E, Gentzke AS, et al. Current cigarette smoking among adults: United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(2):53-59. doi: 10.15585/mmwr.mm6702a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Landy R, Cheung LC, Berg CD, Chaturvedi AK, Robbins HA, Katki HA. Contemporary implications of US Preventive Services Task Force and risk-based guidelines for lung cancer screening eligibility in the United States. Ann Intern Med. 2019;171(5):384-386. doi: 10.7326/M18-3617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families: the Framingham offspring study. Am J Epidemiol. 1979;110(3):281-290. doi: 10.1093/oxfordjournals.aje.a112813 [DOI] [PubMed] [Google Scholar]
- 14.Tsao CW, Vasan RS. Cohort profile: the Framingham Heart Study (FHS): overview of milestones in cardiovascular epidemiology. Int J Epidemiol. 2015;44(6):1800-1813. doi: 10.1093/ije/dyv337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lloyd-Jones DM, Martin DO, Larson MG, Levy D. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med. 1998;129(12):1020-1026. doi: 10.7326/0003-4819-129-12-199812150-00005 [DOI] [PubMed] [Google Scholar]
- 16.Fox CS, Evans JC, Larson MG, et al. A comparison of death certificate out-of-hospital coronary heart disease death with physician-adjudicated sudden cardiac death. Am J Cardiol. 2005;95(7):856-859. doi: 10.1016/j.amjcard.2004.12.011 [DOI] [PubMed] [Google Scholar]
- 17.Ngwa JS, Cabral HJ, Cheng DM, et al. A comparison of time dependent Cox regression, pooled logistic regression and cross sectional pooling with simulations and an application to the Framingham Heart Study. BMC Med Res Methodol. 2016;16(1):148. doi: 10.1186/s12874-016-0248-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.D’Agostino RB, Lee M-L, Belanger AJ, Cupples LA, Anderson K, Kannel WB. Relation of pooled logistic regression to time dependent Cox regression analysis: the Framingham Heart Study. Stat Med. 1990;9(12):1501-1515. doi: 10.1002/sim.4780091214 [DOI] [PubMed] [Google Scholar]
- 19.Wei LJ, Lin DY, Weissfeld L. Regression analysis of multivariate incomplete failure time data by modeling marginal distributions. J Am Stat Assoc. 1989;84(408):1065-1073. doi: 10.1080/01621459.1989.10478873 [DOI] [Google Scholar]
- 20.Feng Z, McLerran D, Grizzle J. A comparison of statistical methods for clustered data analysis with Gaussian error. Stat Med. 1996;15(16):1793-1806. doi: [DOI] [PubMed] [Google Scholar]
- 21.Griffin MP, O’Shea TM, Bissonette EA, Harrell FE Jr, Lake DE, Moorman JR. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr Res. 2003;53(6):920-926. doi: 10.1203/01.PDR.0000064904.05313.D2 [DOI] [PubMed] [Google Scholar]
- 22.Hlatky MA, Greenland P, Arnett DK, et al. ; American Heart Association Expert Panel on Subclinical Atherosclerotic Diseases and Emerging Risk Factors and the Stroke Council . Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119(17):2408-2416. doi: 10.1161/CIRCULATIONAHA.109.192278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harrell FE. The PHGLM procedure. In: SUGI Supplemental Library Guide. 5th ed. SAS Institute; 1986. [Google Scholar]
- 24.Steyerberg EW, Vickers AJ, Cook NR, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21(1):128-138. doi: 10.1097/EDE.0b013e3181c30fb2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pencina MJ, D’Agostino RB, Vasan RS. Statistical methods for assessment of added usefulness of new biomarkers. Clin Chem Lab Med. 2010;48(12):1703-1711. doi: 10.1515/CCLM.2010.340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157-172. doi: 10.1002/sim.2929 [DOI] [PubMed] [Google Scholar]
- 27.Pencina MJ, D’Agostino RB, Pencina KM, Janssens AC, Greenland P, Greenland P. Interpreting incremental value of markers added to risk prediction models. Am J Epidemiol. 2012;176(6):473-481. doi: 10.1093/aje/kws207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.D’Agostino RB, Nam BH. Evaluation of the performance of survival analysis models: discrimination and calibration measures. Handbook Stat. 2004;23:1-25. [Google Scholar]
- 29.Maddala G. Limited-Dependent and Qualitative Variables in Econometrics. Cambridge University Press; 1983. doi: 10.1017/CBO9780511810176 [DOI] [Google Scholar]
- 30.Nagelkerke NJD. A note on a general definition of the coefficient of determination. Biometrika. 1993:78(3);691-692. doi: 10.1093/biomet/78.3.691 [DOI] [Google Scholar]
- 31.Smoking Cessation: A Report of the Surgeon General. US Department of Health and Human Services; 2020. Accessed June 9, 2020. https://www.hhs.gov/sites/default/files/2020-cessation-sgr-full-report.pdf [PubMed]
- 32.Splansky GL, Corey D, Yang Q, et al. The Third generation cohort of the National Heart, Lung, and Blood Institute’s Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol. 2007;165(11):1328-1335. doi: 10.1093/aje/kwm021 [DOI] [PubMed] [Google Scholar]
- 33.Centers for Medicare & Medicaid Services . Screening for lung cancer with low dose computed tomography (LDCT). Accessed November 3, 2021. https://www.cms.gov/medicare-coverage-database/view/ncacal-decision-memo.aspx?proposed=N&NCAId=274
- 34.Laaksonen M, Rahkonen O, Karvonen S, Lahelma E. Socioeconomic status and smoking: analysing inequalities with multiple indicators. Eur J Public Health. 2005;15(3):262-369. doi: 10.1093/eurpub/cki115 [DOI] [PubMed] [Google Scholar]
- 35.Garrett BE, Martell BN, Caraballo RS, King BA. Socioeconomic differences in cigarette smoking among sociodemographic groups. Prev Chronic Dis. 2019;16(6):E74. doi: 10.5888/pcd16.180553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. 2012;1248:107-123. doi: 10.1111/j.1749-6632.2011.06202.x [DOI] [PubMed] [Google Scholar]
- 37.Colantonio LD, Richman JS, Carson AP, et al. Performance of the atherosclerotic cardiovascular disease pooled cohort risk equations by social deprivation status. J Am Heart Assoc. 2017;6(3):e005676. doi: 10.1161/JAHA.117.005676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dalton JE, Perzynski AT, Zidar DA, et al. Accuracy of cardiovascular risk prediction varies by neighborhood socioeconomic position: a retrospective cohort study. Ann Intern Med. 2017;167(7):456-464. doi: 10.7326/M16-2543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kang L, Chen W, Petrick NA, Gallas BD. Comparing two correlated C indices with right-censored survival outcome: a one-shot nonparametric approach. Stat Med. 2015;34(4):685-703. doi: 10.1002/sim.6370 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eFigure 1. Timeline for FHS Offspring Examinations
eFigure 2. Calibration Plots in Men: Observed Probability (y-axis) vs. Predicted Probability (x-axis)
eFigure 3. Calibration Plots in Women: Observed Probability (y-axis) vs. Predicted Probability (x-axis)
eFigure 4. Observed vs. Predicted Plots in Men by Deciles: Observed Probability (y-axis) vs. Predicted Probability (x-axis)
eFigure 5. Observed vs. Predicted Plots in Women by Deciles: Observed Probability (y-axis) vs. Predicted Probability (x-axis)
eFigure 6. Predicted Probability of ASCVD in Men: Models with Additional Smoking Data (y-axis) vs. Reference Model with 2013 PCE Variables (x-axis)
eFigure 7. Predicted Probability of ASCVD in Women: Models with Additional Smoking Data (y-axis) vs. Reference Model with 2013 PCE Variables (x-axis)
eTable 1. Reclassification of Risk in Heavy Ever Smoking (>20 Pack-Years) Men
eTable 2. Reclassification of Risk in Heavy Ever Smoking (>20 Pack-Years) Women
eTable 3. Validation Sample Model Results