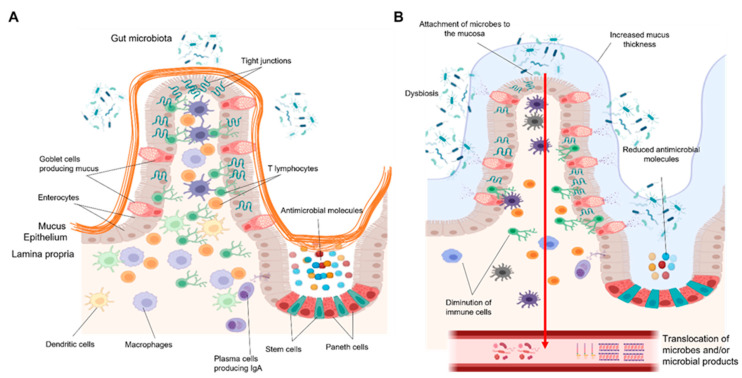
Figure 1.
(A) The small intestinal barrier in healthy conditions. The intestinal barrier is composed of three main layers: the mucus, the epithelium, and the lamina propria. The epithelium, which is overlaid by a thin and discontinuous mucus layer, together with enterocytes and specialized cells constitute a first line of defense. Immune cells in the mucosa further fine-tune the defense mechanisms against pathogens. Macrophages underlying the epithelium regulate immune response by phagocytosis of microbes and production of large amounts of anti-inflammatory cytokines, thus preventing excessive immune responses. Dendritic cells capture, process, and present microbial antigens to different adaptive immune cells. T lymphocytes rapidly act against pathogens by killing infected cells, producing cytokines, and coordinating immune responses. (B) The small intestinal barrier in patients with an alcohol-use disorder. Chronic alcohol consumption is associated with alterations in the composition of the gut microbiota, increased attachment of microbes to the intestinal mucosa, and their translocation into the portal and systemic circulation. This process is enhanced by impairment of various epithelial and immune defense mechanisms. A loose, thickened mucus layer as well as reduced production of antimicrobial molecules and a diminution of macrophages and T lymphocytes all contribute to the failing gut barrier in AUD patients. Figures were created with Biorender.com (14 November 2021).