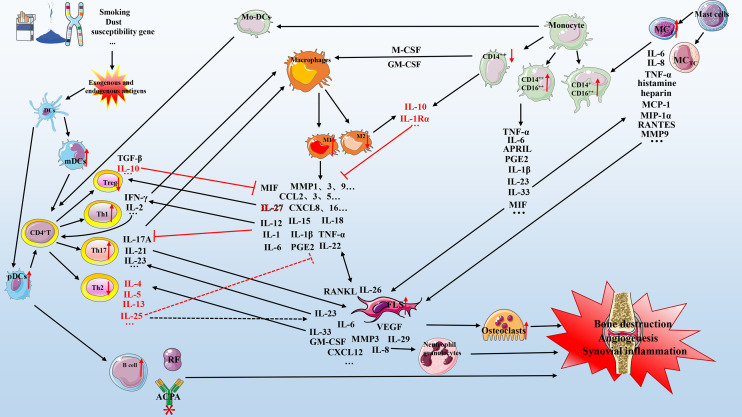
Figure 1.
Mechanism of cell-cytokine interaction in RA. Various factors (e.g., smoking, dust, genetic factors, and microorganisms) lead to the production of exogenous and endogenous antigens. Antigen-presenting cells (primarily dendritic cells) present exogenous and endogenous antigens to CD4+ T cells that differentiate into T cells with different functions, including Th1, Th2, and Th17. These cells cooperate with mast cells, macrophages, and monocytes to secrete multiple pro-inflammatory mediators that act on FLSs and osteoclasts, which in turn can secrete various biological mediators to aggravate the circulation. The anti-inflammatory mechanism (red represents anti-inflammatory mediators) is active but insufficient to inhibit the pro-inflammatory process (black represents pro-inflammatory mediators). Briefly, the interaction of various cell subgroups and cell mediators forms a complex network that promotes the development of RA, including bone destruction, angiogenesis, and synovial inflammation. DC, dendritic cells; IL, interleukin; TNF-α, tumor necrosis factor-α; mDCs, myeloid DCs; pDCs, plasmacytoid DCs; GM-CSF, granulocyte-macrophage colony-stimulating factor; M-CSF, macrophage colony-stimulating factor; CXCL, chemokine CXC ligand; CCL, CC-chemokine ligand; MMP, matrix metalloproteinase; MCP-1, monocyte chemoattractant protein-1; PGE2, prostaglandin E2; APRIL, a proliferation-inducing ligand; RF, rheumatoid factor; ACPA, anti-citrullinated protein antibody; FLS, fibroblast-like synoviocyte; TGF, transforming growth factor; VEGF, vascular endothelial growth factor; MC, mast cell.