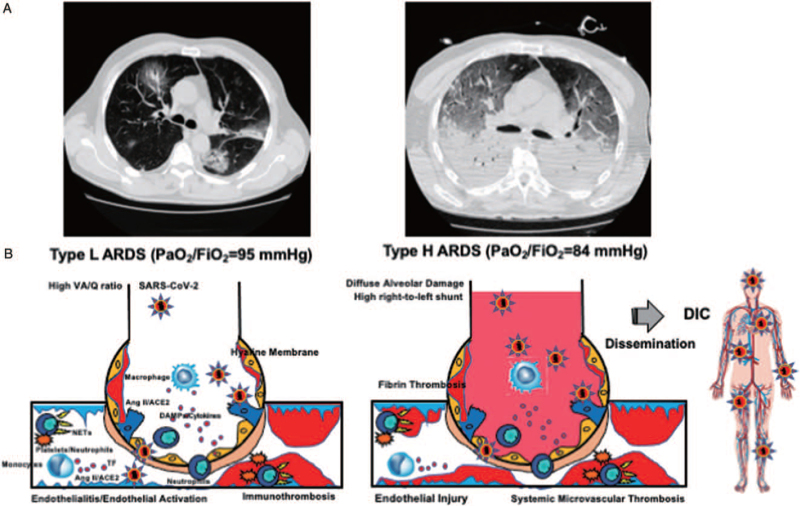
Fig. 1.
Pathomechanisms of COVID-19-associated ARDS. A, Typical CT findings of two phenotypes of COVID-19-associated ARDS. B, SARS-CoV-2 binds to ACE2, leading to its downregulation and increase in Ang II levels, resulting in Ang II-induced coagulopathy. SARS-CoV-2 RNA, which is a pathogen-associated molecular pattern, and damage-associated molecular pattern generated by pyroptosis and necroptosis of virus-infected cells that bind to pattern recognition receptors and induce the expression of inflammatory cytokines and activation of platelets and neutrophils, which results in NETosis-induced coagulopathy. Both coagulopathies activate coagulation and impair the function of anticoagulation factors that are associated with endothelial activation and injury. Fibrinolytic pathways are activated or inhibited based on the balance of SARS-CoV-2-induced fibrin(ogen)olysis and PAI-1-mediated inhibition of fibrinolysis. Type L ARDS represents early phase of COVID-19, which is characterized microvascular immunothrombosis-induced hypoperfusion both in damaged and normal lung alveoli. The main pathomechanism of hypoxemia in type L ARDS is high VA/Q ratio with preserved compliance. Type H ARDS represents the more typical ARDS with hypoxemia, which is caused by diffuse alveolar damage-induced high right-to-left shunt with deteriorated compliance. Type H ARDS, in severe cases, may lead to systemic microvascular thrombosis, also called disseminated intravascular coagulation, as a result of dysregulated immunothrombosis disseminating to the whole body. ACE2 indicates angiotensin-converting enzyme 2; Ang II, angiotensin II; ARDS, acute respiratory distress syndrome; COVID19, coronavirus disease 2019; DAMPs, damage-associated molecular pattern; DIC, disseminated intravascular coagulation; NETs, neutrophil extracellular traps; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TF, tissue factor; VA/Q, ventilation/perfusion. A, Adapted from (8) with modification (Creative Commons Attribution-NonCommercial 4.0 International License).