Abstract
Objective
The study objective was to identify the top 10 research priorities for expectant parents and caregivers of children up to age 24 months.
Design
A priority setting partnership using a modified James Lind Alliance approach was implemented. First, a core steering committee was formed, consisting of 17 parents, clinicians and community agency representatives. Second, through in-person collaboration with steering committee members, we developed and distributed a survey to identify research priorities across 12 topics. In total, 596 participants consented and 480 completed the survey. Survey responses were grouped and themed into codes during a consensus-building workshop with steering committee members (n=18). Research and practice experts were consulted to provide feedback on which themes had already been researched. An in-person (n=21) workshop was used to establish the top 34 priorities, which were circulated to the broader steering committee (n=25) via an online survey. Finally, the core steering committee members (n=18) met to determine and rank a top 10 (plus 1) list of research priorities.
Setting
This study was conducted in Alberta, Canada.
Participants
Expectant parents and caregivers of children up to age 24 months.
Results
Survey results provided 3232 responses, with 202 unique priorities. After expert feedback and steering committee consensus, a list of 34 priorities was moved forward for final consideration. The final top 10 (plus 1) research priorities included three priorities on mental health/relationships, two priorities on each of access to information, immunity and child development, and one priority on each of sleep, pregnancy/labour and feeding. Selecting 11 instead of 10 priorities was based on steering committee consensus.
Conclusions
The findings will direct future maternal–child research, ensuring it is rooted in parent-identified priorities that represent contemporary needs. To provide meaningful outcomes, research in these priority areas must consider diverse socioeconomic backgrounds and experiences.
Keywords: community child health, primary care, public health
Strengths and limitations of this study.
The study had a large sample size (n=480) for the online survey, comparable to other priority setting partnerships.
Targeted recruitment strategies, including in-person recruitment at community and social service locations and father parenting classes, were used to successfully improve representation of diverse participants.
Although attention was paid to promote genuine participation of diverse stakeholders and reach consensus on the research priorities, there is potential that these priorities were influenced by the steering committee members’ and/or researchers’ inherent and individual biases.
While the partnership approach followed principles of participatory action research and was modelled after other published studies that used a modified James Lind Alliance methodology, this approach has not yet been validated.
By creating a welcoming and family-friendly atmosphere and including alternate engagement strategies, parents were meaningfully engaged throughout the partnership process, resulting in the identification of parent-oriented research priorities, many of which differed from priorities previously established by researchers, funders and industry.
Introduction
Due to the critical and rapid development that occurs within the first 3 years of life, investing in early childhood has an estimated return of 800%.1 Parents of young children have the greatest potential to optimise social and environmental conditions to foster optimal child health outcomes.2 High parental expectations, intensive parenting, and increased access to information have drastically changed parenting experiences over the past 10–15 years.3 The dynamic nature of the contemporary maternal–child and parenting landscape may be inadequately incorporated into existing research priorities and questions. Further, researchers and clinicians often encounter difficulties effectively translating and implementing research on child health and development.4 As the knowledge base for supporting healthy developmental outcomes grows in breadth and scope, effectively prioritising research investment is crucial to maximise impact and minimise research waste.5
Understanding health research priorities of knowledge users, such as parents, clinicians and community agency representatives, is vital to conducting research that is more likely to contribute to meaningful changes in health outcomes.6 Evidence generated without the consideration of the knowledge user will have minimal effect on clinical practice and reduce meaningful outcomes.7 Further, there is growing awareness of the importance of adopting an intersectional lens when conducting health research to adequately address culturally and socio-politically appropriate parenting outcomes.8 Employing an intersectional lens by centring the perspectives of knowledge users will result in evidence and resultant policies that better accounts for their diverse needs.9 Engaging knowledge users in research priority setting initiatives is recognised as an effective and ethical means of prioritising the allocation of limited public research funds.7 Not only does priority setting work promote researcher accountability, but this integrative approach to knowledge translation may also reduce lag time between producing and implementing knowledge,10 while contributing to the development of culturally and socially meaningful outcomes. Moreover, knowledge user involvement in research may enhance engagement with, and uptake of, interventions and services that support early childhood health, resulting in more timely and effective care.
Priority setting partnerships
Patient-oriented research, specifically priority setting partnerships (PSPs), is increasingly identified as an effective method to decrease research waste and develop research outcomes meaningful to knowledge users.7 PSPs bring together knowledge users, including clinicians, researchers and patients or other service users (ie, parents of well children), to identify and prioritise research uncertainties using a systematic and collaborative process.
Involving knowledge users such as parents and caregivers (ie, those who provide direct care for children and who may or may not self-identify as parents, as well as professional caregivers who provide care to families with children) in the foundational development of research through PSPs is a feasible method to produce meaningful outcomes—by creating knowledge important to parents and caregivers, the likelihood of new evidence uptake and shifting healthcare practices is increased. To date, there have been no PSPs focused on identifying community-based research priorities for families of well children from conception to age 24 months. When purposefully employing a participatory action framework, PSPs can use intersectional principles by capturing the perspectives and experiences of traditionally neglected populations.8 9 Therefore, the objective of this study was to engage a diverse group of perspectives in identifying the top 10 research priorities of expectant parents and caregivers of children up to age 24 months.
Methods
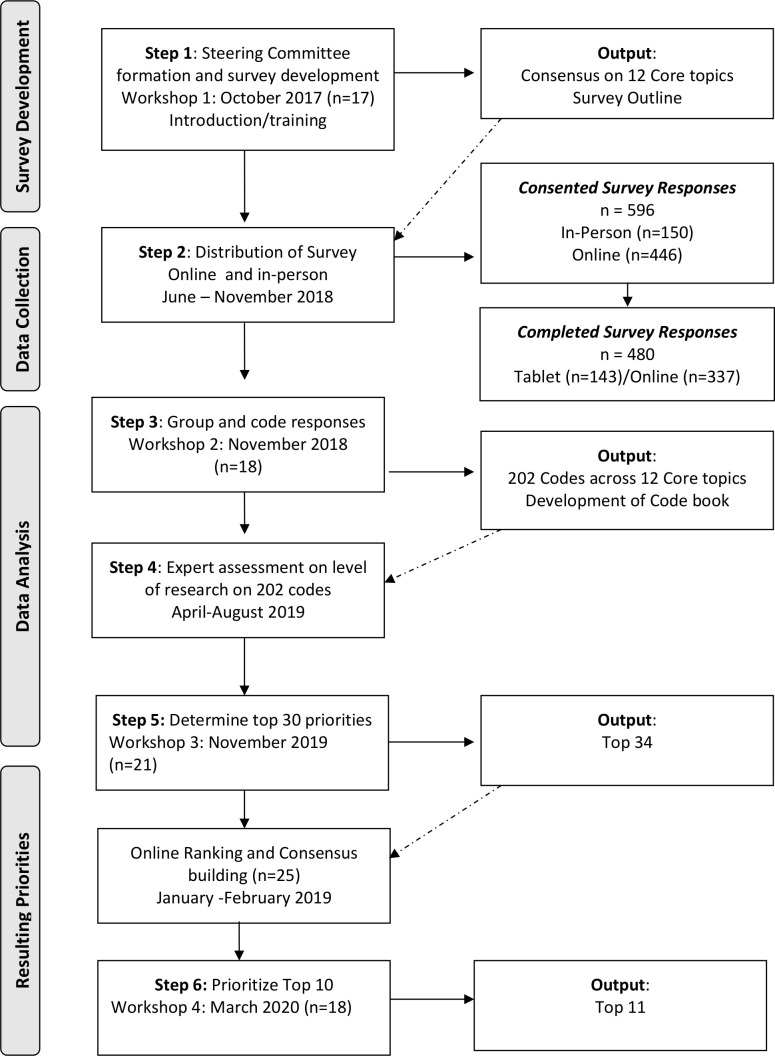
The Family Research Agenda Initiative Setting (FRAISE) project used a modified James Lind Alliance (JLA)11 approach to identify research priorities of knowledge users (eg, parents, clinicians and community agency representatives) within Alberta, a province in Western Canada.12 Many PSPs use the JLA approach6; however, employing an accredited JLA facilitator may be impractical for lower resourced research studies. As such, a modified approach to the JLA method has emerged as a feasible alternative.13 These modifications included facilitation of the initial steering committee workshop by subject matter experts in patient and public engagement and PSPs (ie, external facilitators from the Alberta Strategy for Patient-Oriented Research Support Unit), rather than a JLA advisor. After this initial workshop, the lead authors, who are trained in group facilitation and community engagement, facilitated the remaining in-person workshops using consensus-building and shared decision-making strategies. During the analysis and prioritisation of the potential research priorities, we used collective sensemaking to narrow down and rank the research priorities. Rather than conduct rapid literature reviews to determine the level of evidence available for the research uncertainties, we asked practice and research subject matter experts to rate the availability of evidence on research uncertainties. These rankings were then used by the steering committee members to help them prioritise the top 30 priorities. FRAISE applied a consensus-building and strengths-based approach, modelled after participatory action research and the JLA. JLA PSPs bring together patients or service users with lived experience and/or their carers (eg, family members)and clinicians, which requires sensitivity to varying participant capacities, ongoing effective communication, transparency in decision making and inclusivity of all views.11 The modified JLA process used in the FRAISE project involved a series of iterative steps (figure 1): (1) formation of a steering committee, including parents, clinicians and community agency representatives and online survey development; (2) delivering the survey to gather research uncertainties or questions from parents, clinicians and community agency representatives; (3) grouping responses into codes; (4) consulting with research and practice experts to determine which codes were already well researched, (5) consensus building to determine and rank the top priorities and (6) prioritise and rank top 10 research priorities as directed by the steering committee.
Figure 1.
FRAISE study flow diagram. FRAISE, Family Research Agenda Initiative Setting.
In previous iterations of the JLA, determining priorities of those experiencing social vulnerability was a challenge14; as such, the FRAISE project employed in-person techniques with key community organisations to include responses from respondents with a variety of socioeconomic backgrounds. These techniques included research assistants physically attending programmes and services that provided targeted care to populations who were under-represented in the survey to recruit potential participants. To facilitate participation at these sites, research assistants carried electronic tablets that participants could use to complete the online survey before or after their programming or appointments. Parent steering committee members were given a US$50 honorarium, childcare and meals at each session. We followed the REporting guideline for PRIority SEtting of health research15 for this study. All survey participants provided informed consent.
Steering committee
Between November 2017 and March 2020, we engaged a steering committee comprised of researchers, parents and caregivers (ie, clinicians, community agency representatives). We aimed for 30 steering committee members who mirrored the regional population, including a minimum of 3% who were Indigenous, and 30% who identified as immigrants and/or visible minorities.16 While membership was flexible to accommodate the realities of parenting young children, a core group of steering committee members emerged. The core group included 15 parents, 4 clinicians and 2 community agency representatives. While we did not meet our target for Indigenous representation, we exceeded our aim for a diverse group, with 5 of the 15 parents identifying as a visible minority, 2 parents identifying as fathers and 2 parents identifying as new to Canada. To accommodate the regionality and required flexibility of steering committee members, we provided opportunities for a larger online group of additional steering committee members. These members consisted of parents and caregivers who attended some, but not all workshops in person, as well as healthcare providers from other geographic sites in Alberta, and directors and managerial staff who were unable to attend in-person workshops due to time constraints. The size of this group fluctuated throughout the study timeline, with a maximum of 10 members in addition to the core steering committee. The role of the larger steering committee was to provide online feedback and consultation throughout the priority setting process.
Online survey development to identify research questions
The first consensus building workshop focused on introducing and training the core steering committee, orientating them to FRAISE, and developing the survey instrument. To develop the online survey, members of the core steering committee (n=17) collaboratively identified 12 broad parenting topics of interest. Researchers then developed open-ended survey questions that could elicit potential research questions from families related to each of these 12 topics. The survey was refined by the core steering committee using an iterative process of online and in-person engagement. The final survey was piloted with a small group of parents who were unfamiliar with the FRAISE project. The survey was launched online using Qualtrics XM Survey Software (Qualtrics, Provo, Utah, USA) in May 2018 and promoted via Facebook and Twitter. In-person survey completion sessions were also held at various inner-city community and healthcare agencies to increase the inclusion of under-represented populations, particularly those without reliable internet access and who may be experiencing social vulnerability.
Priority setting workshops and consensus building
Three additional in-person priority setting workshops were hosted with the steering committee to build consensus around survey development, survey response theming, the top 30 list, and the top 10 list (figure 1). Each session was structured using a nominal group technique.17 To analyse survey responses and identify top research priorities, core steering committee members were broken into six groups and provided with survey responses from four of the 12 topic areas. Each author acted as a group facilitator to guide the work and ensure that all voices were heard, but not to direct the content of the discussion. Each group member was provided with research questions from the survey results and given time to silently generate ideas. Then, each group member shared their ideas; the facilitator clarified and recorded them. Following group discussion to clarify ideas and priorities, group members voted and ranked each priority, with the top priorities moved forward to the steering committee for consideration. Consensus building concluded with discussion and agreement on which content to move forward from each session. After each in-person session, this process was repeated, using survey software with the broader online steering committee to develop consensus. In the spirit of true consensus building and PSP, researchers facilitated sessions allowing steering committee members to drive decisions and finalise results.17 As such, modifications were made to the wording of the final top 10 list, resulting in an additional (11th) research priority.13
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, or report writing. All authors had access to study data. The corresponding author, EK, had full access to all data and responsibility for the final decision to submit for publication.
Data analysis
Characteristics of survey participants were calculated using descriptive statistics in Microsoft Excel. Responses from the survey were captured verbatim in each of the 12 topic areas. All individual responses were printed and cut into individual items. In-person steering committee members (n=18) worked together to group responses into themes, within each topic area. Responses from each topic area were analysed by two separate groups to validate theming. Researchers then built the resultant themes (research priorities) into a codebook. Research and practice experts provided feedback on the extent to which each of the 202 codes had been researched. These experts were asked to indicate if each potential research priority was: (1) well researched (systematic reviews and meta-analysis available), (2) somewhat researched (single studies, some inconsistent evidence on topic), (3) not researched (no studies) or (4) unsure. Experts were encouraged to provide comments or feedback on each of the potential priorities. This information, in conjunction with the 202 codes, was provided to the steering committee during a third consensus building workshop (n=21) to develop the top 30 list. Steering committee members were instructed to review and consider expert feedback when building consensus around which of the 30 priorities to move forward. While the frequency that a particular priority was submitted in the online survey was considered important for subsequent prioritisation, steering committee members did not rely solely on these counts to move items forward to the top 30 and top 10 lists. While the original intent was to narrow down the priorities to a top 30 list, at the time of prioritisation, the steering committee reached a consensus that the list should include 34 priorities.
The top 34 list was shared with the broader online steering committee and committee members (n=25) were asked to select and rank their top 10 selections. These results were brought back to the fourth and final consensus building workshop (n=18) to develop the top 10 priorities. The final top 10 (plus 1) list was circulated online for final approval. Steering committee members were also asked to rank the top 10 (plus 1) priorities on their perceived order of importance.
Patient and public involvement statement
The public was engaged via membership in the steering committee after the study and research objectives were conceptualised, and funding was obtained,. Steering committee members designed the survey and participated in data collection via disseminating the survey through their professional and social networks and provided advice on how to increase survey response rates for diverse groups. These members also provided feedback on the survey regarding participant burden and conducted data analysis in collaboration with the researcher team. In addition, steering committee members were sponsored to participate in local, regional and national study dissemination via virtual and in-person child health rounds and conferences as well as manuscript authorship (LC and SD).
Results
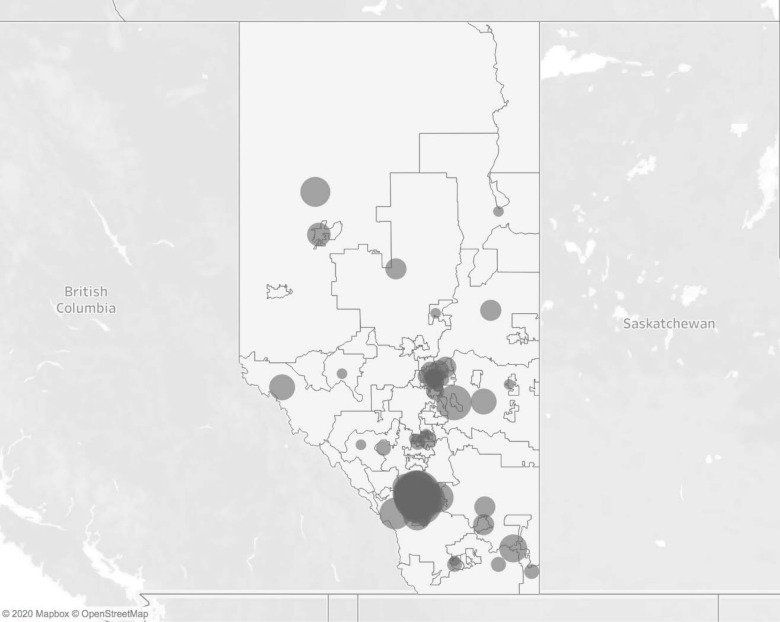
In total, 596 participants consented to participate in the survey, of which 480 completed the survey. Of these, the majority were parents (76.3%; n=130 tablet; n=236 online), 16.0% were clinicians (n=3 tablet; n=74 online), 4.8% were early childhood educators (n=10 tablet; n=13 online), and 2.9% were community agency representatives (n=0 tablet; n=22 online). Most participants were recruited via social media and electronic networks (n=337, 70.2%), with 29.8% (n=143) recruited during targeted in-person sessions where participants were provided with a tablet to record responses. The mean age of all survey respondents was 34.1 years (SD=9.1), with tablet-based respondents having a slightly younger mean age in years (32.1; SD=5.9) than the mean age of online-based respondents (34.8; SD=9.9). For parent participants who were not born in Canada (n=65), the mean number of years in Canada was 10.7 (SD=11.4), with tablet-based respondents having fewer mean years in Canada (M=8.1; SD=9.3) than online-based respondents (M=13.6; SD=13.0). Table 1 describes participant and household characteristics. The socioeconomic and ethnicity distribution of parent participants was comparable to population distributions.16 Participation rates mirrored geographical population densities (figure 2).
Table 1.
FRAISE survey participant characteristics
| All respondents | Total completed (N=480) |
Online survey (n=337) |
Tablet survey (n=143) |
|||
| N | % | n | % | n | % | |
| Employment status | ||||||
| Working for pay, profit, or self-employed | 233 | 48.5 | 182 | 54.0 | 51 | 35.7 |
| Caregiving (including parental or maternity leave) | 183 | 38.1 | 122 | 36.2 | 61 | 42.7 |
| Not working, but looking | 14 | 2.9 | 9 | 2.7 | 5 | 3.5 |
| Going to school, retired, cannot work due to disability or illness or other | 30 | 6.3 | 10 | 3.0 | 20 | 14.0 |
| Completed post-secondary education (eg, certificate or diploma programme, undergraduate/graduate degree) | 404 | 84.2 | 306 | 90.8 | 98 | 68.5 |
| Ethnicity* | ||||||
| Caucasian | 333 | 69.4 | 256 | 76.0 | 77 | 53.8 |
| Chinese | 29 | 6.0 | 14 | 4.2 | 15 | 10.5 |
| South Asian | 14 | 2.9 | 10 | 3.0 | 4 | 2.8 |
| Latin American | 12 | 2.5 | 7 | 2.1 | 5 | 3.5 |
| Indigenous | 25 | 5.2 | 6 | 1.8 | 19 | 13.3 |
| Caribbean | 7 | 1.5 | 6 | 1.8 | 1 | 0.7 |
| Filipino | 6 | 1.3 | 4 | 1.2 | 2 | 1.4 |
| Arab | 5 | 1.0 | 3 | 0.9 | 2 | 1.4 |
| Korean | 4 | 0.8 | 3 | 0.9 | 1 | 0.7 |
| Southeast Asian | 7 | 1.5 | 3 | 0.9 | 4 | 2.8 |
| Japanese | 2 | 0.4 | 2 | 0.6 | 1 | 0.7 |
| African | 8 | 1.7 | 1 | 0.3 | 7 | 4.9 |
| West Asian | 2 | 0.4 | 0 | 0.0 | 2 | 1.4 |
| Other | 14 | 2.9 | 8 | 2.4 | 6 | 4.2 |
| Prefer not to say | 15 | 3.1 | 9 | 2.7 | 6 | 4.2 |
| Clinicians | 77 | 16.0 | 74 | 22.0 | 3 | 2.1 |
| Nurse | 47 | 9.8 | 47 | 13.9 | 0 | – |
| Physician | 7 | 1.5 | 7 | 2.1 | 0 | – |
| Dietician | 3 | 0.6 | 3 | 0.9 | 0 | – |
| Occupational therapist | 3 | 0.6 | 3 | 0.9 | 0 | – |
| Other (midwife, social worker, etc) | 17 | 3.5 | 14 | 4.2 | 3 | 2.1 |
| Community agency representative | 14 | 2.9 | 14 | 4.2 | 0 | – |
| Early childhood educator/care provider (eg, nanny, daycare, preschool) | 23 | 4.8 | 13 | 3.9 | 10 | 7.0 |
| Parent | 366 | 76.3 | 236 | 70.0 | 130 | 90.9 |
| Mother | 292 | 60.8 | 194 | 57.6 | 98 | 68.5 |
| # pregnant | 136 | 28.3 | 85 | 25.2 | 51 | 35.7 |
| Father | 71 | 14.8 | 40 | 11.9 | 31 | 21.7 |
| Other (eg, grandparent, aunt) | 3 | 0.6 | 2 | 0.6 | 1 | 0.7 |
| Parent respondents only (n=366) | ||||||
| Partnered | 305 | 83.3 | 206 | 87.3 | 99 | 76.2 |
| No of households with children | ||||||
| One child in household | 173 | 47.3 | 121 | 51.3 | 52 | 40.0 |
| Two children in household | 74 | 20.2 | 48 | 20.3 | 26 | 20.0 |
| Three children in household | 27 | 7.4 | 15 | 6.4 | 12 | 9.2 |
| 4+ children in household | 13 | 3.6 | 4 | 1.7 | 9 | 6.9 |
| Born in Canada (Yes) | 280 | 76.5 | 190 | 80.5 | 90 | 69.2 |
| English as primary household language | 318 | 86.9 | 206 | 87.3 | 112 | 86.2 |
| Household income (yearly) | ||||||
| Less than US$40 000 | 66 | 18.0 | 17 | 7.2 | 49 | 37.7 |
| US$40 000–US$79 999 | 82 | 22.4 | 64 | 27.1 | 18 | 13.8 |
| US$80 000–US$119 999 | 69 | 18.9 | 54 | 22.9 | 15 | 11.5 |
| US$120 000–US$159 999 | 49 | 13.4 | 34 | 14.4 | 15 | 11.5 |
| More than US$160 000 | 53 | 14.5 | 35 | 14.8 | 18 | 13.8 |
| I don't want to say | 31 | 8.5 | 19 | 8.1 | 12 | 9.2 |
Due to missing data, numbers in this table may not sum to the total number of completed responses.
*Indicates respondents could choose all that apply.
FRAISE, Family Research Agenda Initiative Setting.
Figure 2.
Geographical distribution of responses.
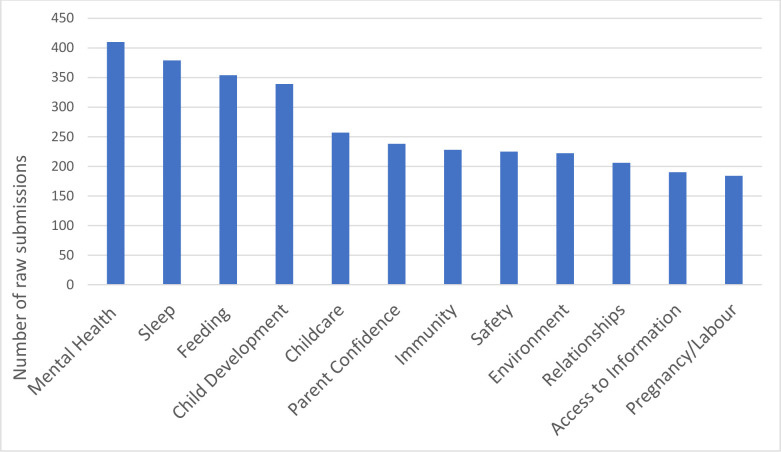
In total, we received 3232 submissions of potential research priorities spread across all 12 topic areas (figure 3). When asked to rank the 12 broad parenting topics of interest, survey participants ranked stress, emotional and mental health; sleep; and infant feeding as the three most important parenting topics. The 3232 suggested priorities obtained via survey responses were coded, themed, and collapsed by the steering committee, resulting in 202 unique priorities (figure 1). Of these 202 priorities, 34 were shortlisted for consideration in the top 10 list (online supplemental table). Steering committee members used this shortlist to build consensus on the final top 10 (plus 1) list of research priorities (table 2).
Figure 3.
Number of raw submissions in each topic area from provincial survey.
Table 2.
Final list and topic areas of the top 10 (plus 1) research priorities from conception to 2 years of age for families in the community
| Rank | Question | Topic area |
| 1 | How can families be supported to develop healthy coping strategies, emotional regulation, and resiliency in both parents and children? | Mental health/relationships |
| 2 | How can families access supportive care and information when things do not go as expected during pregnancy, labour, birth, or postpartum? | Access to information/pregnancy, labour and birth |
| 3 | How can the healthcare system and providers ensure access to prevention and treatment of mental health concerns in a safe and trusting environment? | Mental health |
| 4 | How do families navigate multiple sources of health information and access services tailored to their specific circumstances? | Access to information |
| 5 | What supports and services can be developed at the individual, family, community, and government levels to build emotional/mental well-being, physical health, and healthy relationships? | Mental health/relationships |
| 6 | How can eczema, asthma and allergies be more effectively prevented, assessed and treated? | Immunity |
| 7 | In a constantly changing social and physical environment, how can families increase safety and manage developmentally appropriate risk-taking? | Child development/child safety/environmental risk |
| 8 | How can sleep problems be prevented, assessed, and treated in a culturally appropriate way that is tailored to individual families? | Sleep |
| 9 | How can families be better supported to make informed, family-centred feeding decisions? | Feeding |
| 10 | How can families be better supported to promote healthy child development, recognise milestones and access services for delay? | Child development |
| 11 | With increasing vaccine hesitancy, how can individual, family and population health best be protected? | Immunity |
bmjopen-2020-047919supp001.pdf (45.7KB, pdf)
Discussion
To our knowledge, this is the first attempt to identify community-based research priorities for families of well children from conception to age 24 months. Throughout all steps of the PSP, concerns for mental, social and emotional well-being of parents and children were consistently expressed as priority areas. Comparing the top 10 (plus 1) priorities with the initial 12 survey categories, we found that stress, emotional and mental health were consistently a top concern for families and were identified in three of the top 10 (plus 1) priorities. Additionally, steering committee members repeatedly specified the need for structural health system changes at the individual, family, community and government levels to focus on building emotional/mental well-being, physical health and healthy relationships—taking the onus off individual families to solve problems related to mental and physical wellness and prioritising policy and systems shifts. As such, these research priorities highlight the need to situate individual-focused or family-focused research priorities within the context of complex health and social systems and involve multiple sectors such as government and health boards.
Across themes, the top 10 (plus 1) research priorities reflect the importance of fostering access to information and developing information and services using a culturally sensitive and humble framework. While identified as its own research priority (table 2), concerns about access to information emerged in each topic area. The ubiquitous nature of access to information as a research priority raises a fundamental question about the accessibility of safe, reliable and valid information for young families. Previous research from Canada indicates the majority of parents use the internet to access information about children’s health, but many use unreliable sources of information.18 In contrast, Australian women who are pregnant most often reported discussion with their midwife as an information source, while less than half reported using the internet to access information; group information sessions were the least preferred information sources.19 This contrasts with a report from Devolin et al20 where Albertan parents rated the Internet (55.3%) and drop-in programmes (42.9%) as preferred information sources. With such conflicting evidence, it is unsurprising that researchers and care providers have long struggled with providing safe and reliable information related to child and infant health. Healthcare providers and administrators should collaborate with researchers and parents to critically examine health information provision and consider transformative frameworks to create meaningful and innovative knowledge translation strategies to better communicate evidence.
Several research questions related to physical health emerged as important. For example, parents expressed concerns about how eczema, asthma and allergies could be more effectively prevented, assessed and treated; with this class of inflammatory disorders as one of the most common issues in early childhood, this is unsurprising. The fact that parents shared a strong desire for information about preventing these disorders, suggests this is a research area ripe for future development. Additionally, questions emerged about preventing injury while encouraging appropriate physical development and accessing information about culturally appropriate feeding and sleep. While some research exists in each of these areas, evidence is generally underdeveloped, and information needs to be communicated to parents in culturally appropriate and meaningful ways. Of particular importance given the COVID-19 pandemic, parents were unwilling to leave the final steering committee workshop without including a research priority related to vaccine hesitancy. Diverse opinions emerged around this topic, and it became clear that evidence-based information about vaccines and immunity was a valued priority.
Findings from this PSP complement findings from other paediatric research PSPs that have focused on single issue priority setting, such as premature birth,21 stillbirth,22 chronic pain,23 neurodisabilities24 or learning difficulties.25 Despite the breadth in populations and that most existing PSPs were conducted in the UK, research priorities identified in these partnerships related to access to information, mental and emotional health, and healthy relationships, suggesting that these themes are consistently important to parents.
One notable exception to the general trend of conducting PSPs with specialised populations is a Canadian PSP that developed research priorities for preventative care of children aged 0–5 years.26 Consistent with our top research priority of mental and emotional health in children and their parents, the top research question found by Lavigne et al was ‘What are effective strategies for screening and prevention of mental health problems?’ (p.750).26 Our findings confirm and extend this priority of building mental and emotional wellness in children belonging younger age groups (and during conception) by broadening the focus to include parents and protective factors for resilience. This suggests that parent, clinician and researcher priorities are aligned with the emergence of infant mental health (ages 0–5) as a relational concept, whereby infant mental health is supported by optimising the mental health and resiliency of children’s caregivers (ie, parents and family members).1 Other similarities included: (1) supporting child development by improving identification and services for developmental delays; (2) developing effective interventions, supports and services to improve mental health, physical health (obesity, physical activity) and healthy relationships (social skills); and (3) understanding the impact and support of nutritional and feeding factors. Contrasts with our research priorities and those for children aged 0–5 years included: (1) the impact of daycare attendance on child health, (2) behaviour management in children and (3) appropriate screen time for children. In addition, research priorities in our list that were not found in the list for children aged 0–5 years included: (1) how families can access supportive care and information during unexpected experiences in the perinatal period; (2) access to information; (3) how eczema, asthma and allergies can be more effectively prevented, assessed and treated; (4) injury prevention and appropriate levels of risk and (5) sleep problems in families. It should be noted that differences may represent prioritisation related to different developmental stages and ages (ie, screen time is not recommended for children under age two) and/or slight differences in the prioritisation method. For example, helping families identify appropriate childcare appeared in our top 34 list and aligns with a similar research priority related to the impact of daycare attendance in the 0 to 5 years list.
In a Delphi study of perceived research priorities of clinical staff at an Australian parenting centre, Hauck et al27 determined the top research priorities to be related to short-term and long-term evaluation of the effectiveness of the centre’s programmes on children’s behaviour and stress levels, parental expectations, healthy family relationships, as well as parental use of sleep, settling and feeding strategies. Determining the effectiveness of the centre’s programme in the context of postpartum depression was also an identified priority.27 Although these research priorities were not informed by parental participation and may have limited generalisability to other centres and/or countries, it is notable that issues related to sleep, infant feeding, healthy relationships and parental mental health are captured by both ours and Hauck et al’s27 lists. This is not surprising as a study in our same geographical area suggested that breastfeeding, sleep issues, child development, helping children cope with emotions and understanding child brain development were all in the top 10 (plus 1) parenting topics ranked as somewhat or very important by parents.20
Clinical and research applications
To move forward with these research priorities, it is evident that multiple stakeholders must be engaged, and connections made across a variety of sectors and disciplines. Wording for the top 10 (plus 1) research priorities requested consideration of ‘culturally appropriate’ and ‘safe and trusting environments.’ Our findings highlight the need for an increased emphasis on parenting education and culturally appropriate strategies to support mental health and well-being. Adopting an intersectional lens when conducting research and providing care to pregnant and young families, will better address these considerations and provide meaningful evidence to inform health outcomes. Similar to how parents of diverse groups may have differing or intensified concerns relating to child health issues,28 it is important to recognise that research priorities may differ based on community member’s characteristics, specifically in terms of race, income, access to health services and experiences, including racism. These top 10 (plus 1) priorities were developed using an intersectional framework. Moving forward, research in these priority areas must continue to comprehensively and meaningfully include individuals with diverse socioeconomic backgrounds and experiences.9
The findings from this study should be considered in the context of its strengths and limitations. In terms of strengths, there was a large sample size for the online survey comparable to other PSPs; this created space for a broad representation of stakeholders including clinicians, community agency representatives, parents and ethnically diverse representatives of the study location. Limitations included the inherent and individual biases that self-selected, voluntary researchers and steering community members view the world with, which may reduce the generalisability of the final priority list. Given that the research team was composed entirely of white heterosexual women and although attention was paid to ensure participation of fathers, individuals self-identifying as non-white, and those in non-heterosexual or single parent partnerships, these voices may not have been entirely represented in the final priorities. Additionally, while this research PSP used a process based on a previously reported modified JLA approach,13 these modifications have not been validated against the standardised JLA method. Not employing an accredited JLA facilitator means that the study did not have the rigorous external supervision that other JLA-led studies benefit from. Our modifications (eg, using external group facilitators with expertise in patient and public engagement to establish the steering committee rather than an accredited paid JLA advisor; consulting with experts on the level of evidence, rather than conducting rapid literature reviews on each potential research uncertainty) greatly reduced the cost of the project, thereby increasing feasibility. Additionally, the current approach incorporated principles of participatory action research (eg, engaging with a community who have self-identified in reciprocal relationships, recognition of local knowledge and incorporating processes of colearning to take actions that will improve community member’s well-being), which are widely recognised as critical in facilitating meaningful participant engagement and ensuring that participants’ voices are represented throughout the research process.
Researching these family-driven priorities will reduce the knowledge-to-practice gap and generate opportunities to improve services for families, including innovative delivery models and evidence-based treatment options to enable equitable access to services. Further, involving practitioners in the PSP may enhance the implementation of new evidence-based practice recommendations.29 These outcomes, combined with decreased lag time from research to practice, may result in improved child and family outcomes. As a result of our strong collaborative partnerships and inclusion of policy-makers in each stage of the PSP, the provincial health service has already used this information to streamline and enhance evidence-based information delivery to parents and care providers in the province. By sharing the FRAISE top 10 (plus 1) research priorities, we invite other researchers to ensure their work aligns with principles of patient-oriented research as a foundation for future initiatives targeted at improving outcomes in families with young children.
Supplementary Material
Acknowledgments
We thank the Alberta Strategy for Patient-Oriented Research Support Unit for their expertise, guidance, and support in the developmental stages of this project. Notably, Ping Mason-Lai and Sennait Yohannes were instrumental in helping us develop our steering committee. We are extremely grateful to Puneet Punian and Kristen Jensen who assisted with data collection and management and the coordination of in-person steering committee meetings. Alberta Health Services and the Maternal Newborn Child and Youth Health, Strategic Clinical Network were fundamental in providing access to clinicians and participants. We are grateful for the input and participation from our Community Partners including CUPS Calgary, The Calgary Immigrant Women’s Association and Action Dignity (previously the Ethno-cultural Council of Calgary). Most importantly, we thank the families and members of our steering committee for their time and dedication to the FRAISE study.
Footnotes
Twitter: @mbrockwa, @EKeysElizabeth, @ltomfohr, @karen_benzies
MLB and EK contributed equally.
Contributors: EK and MLB drafted the manuscript, which all authors reviewed, provided feedback, and approved the final version. EK, MLB, KSB, CG and KB designed the study. EK, MLB, KSB, CG, KB and LT-M developed the steering committee workshop content. EK, MLB, KSB, CG, KB, LT-M, SD and LC and the Steering Committee devised the data collection instruments. JW, EK, MLB, KSB and CG were responsible for data collection and database design and management. EK, MLB, KSB, CG, KB, LT-M, JW, SD, LC and the steering committee completed the data analyses. EK is responsible for the overall content as the guarantor.
Funding: This work was supported by The Alberta Children’s Hospital Research Institute and Alberta Innovates.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. The research priorities codebook, containing the raw research priorities responses, is available on reasonable request from the corresponding author.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The Conjoint Health Research Ethics Board at the University of Calgary (REB17-0014) approved this research.
References
- 1.Shonkoff JP. Capitalizing on advances in science to reduce the health consequences of early childhood adversity. JAMA Pediatr 2016;170:1003–7. 10.1001/jamapediatrics.2016.1559 [DOI] [PubMed] [Google Scholar]
- 2.Bronfenbrener U, ed. Making human beings human: bioecological perspectives on human development. Thousand Oaks, CA: Sage, 2005. [Google Scholar]
- 3.Wall G. Mothers’ experiences with intensive parenting and brain development discourse. Womens Stud Int Forum 2010;33:253–63. 10.1016/j.wsif.2010.02.019 [DOI] [Google Scholar]
- 4.Albrecht L, Archibald M, Snelgrove-Clarke E, et al. Systematic review of knowledge translation strategies to promote research uptake in child health settings. J Pediatr Nurs 2016;31:235–54. 10.1016/j.pedn.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 5.Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Obstet Gynecol 2009;114:1341–5. 10.1097/AOG.0b013e3181c3020d [DOI] [PubMed] [Google Scholar]
- 6.Manafò E, Petermann L, Vandall-Walker V, et al. Patient and public engagement in priority setting: a systematic rapid review of the literature. PLoS One 2018;13:e0193579. 10.1371/journal.pone.0193579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chalmers I, Bracken MB, Djulbegovic B, et al. How to increase value and reduce waste when research priorities are set. Lancet 2014;383:156–65. 10.1016/S0140-6736(13)62229-1 [DOI] [PubMed] [Google Scholar]
- 8.Shimmin C, Wittmeier KDM, Lavoie JG, et al. Moving towards a more inclusive patient and public involvement in health research paradigm: the incorporation of a trauma-informed intersectional analysis. BMC Health Serv Res 2017;17:539. 10.1186/s12913-017-2463-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bailey J, Steeves V, Burkell J, et al. Getting at equality: research methods informed by the lessons of intersectionality. Int J Qual Methods 2019;18:1–13. 10.1177/1609406919846753 [DOI] [Google Scholar]
- 10.Mann BS, Manns BJ, Dart A, et al. An assessment of dialysis provider's attitudes towards timing of dialysis initiation in Canada. Can J Kidney Health Dis 2014;1:3. 10.1186/2054-3581-1-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cowan K, Oliver S. The James Lind alliance guidebook, 2010. Available: http://www.jlaguidebook.org/pdfguidebook/guidebook.pdf [Accessed 22 Nov 2016].
- 12.Bright KS, Ginn C, Keys EM, et al. Study protocol: determining research priorities of young Albertan families (The Family Research Agenda Initiative Setting Project-FRAISE)-participatory action research. Front Public Health 2018;6:228. 10.3389/fpubh.2018.00228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Breault LJ, Rittenbach K, Hartle K, et al. The top research questions asked by people with lived depression experience in Alberta: a survey. CMAJ Open 2018;6:E398–405. 10.9778/cmajo.20180034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barnieh L, Jun M, Laupacis A, et al. Determining research priorities through partnership with patients: an overview. Semin Dial 2015;28:141–6. 10.1111/sdi.12325 [DOI] [PubMed] [Google Scholar]
- 15.Tong A, Synnot A, Crowe S, et al. Reporting guideline for priority setting of health research (Reprise). BMC Med Res Methodol 2019;19:243. 10.1186/s12874-019-0889-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Statistics Canada . 2011 national household survey: statistics Canada, 2013. Available: https://www12.statcan.gc.ca/nhs-enm/2011/dp-pd/dt-td/Index-eng.cfm [Accessed 7 Oct 2020].
- 17.Carney O, McIntosh J, Worth A. The use of the nominal group technique in research with community nurses. J Adv Nurs 1996;23:1024–9. 10.1046/j.1365-2648.1996.09623.x [DOI] [PubMed] [Google Scholar]
- 18.Pehora C, Gajaria N, Stoute M, et al. Are parents getting it right? A survey of parents' Internet use for children's health care information. Interact J Med Res 2015;4:e12. 10.2196/ijmr.3790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grimes HA, Forster DA, Newton MS. Sources of information used by women during pregnancy to meet their information needs. Midwifery 2014;30:e26–33. 10.1016/j.midw.2013.10.007 [DOI] [PubMed] [Google Scholar]
- 20.Devolin M, Phelps D, Duhaney T, et al. Information and support needs among parents of young children in a region of Canada: a cross-sectional survey. Public Health Nurs 2013;30:193–201. 10.1111/phn.12002 [DOI] [PubMed] [Google Scholar]
- 21.Duley L, Uhm S, Oliver S, et al. Top 15 UK research priorities for preterm birth. Lancet 2014;383:2041–2. 10.1016/S0140-6736(14)60989-2 [DOI] [PubMed] [Google Scholar]
- 22.Heazell AEP, Whitworth MK, Whitcombe J, et al. Research priorities for stillbirth: process overview and results from UK stillbirth priority setting partnership. Ultrasound Obstet Gynecol 2015;46:641–7. 10.1002/uog.15738 [DOI] [PubMed] [Google Scholar]
- 23.Birnie KA, Dib K, Ouellette C, et al. Partnering for pain: a priority setting partnership to identify patient-oriented research priorities for pediatric chronic pain in Canada. CMAJ Open 2019;7:E654–64. 10.9778/cmajo.20190060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morris C, Simkiss D, Busk M, et al. Setting research priorities to improve the health of children and young people with neurodisability: a British Academy of childhood Disability-James Lind alliance research priority setting partnership. BMJ Open 2015;5:e006233. 10.1136/bmjopen-2014-006233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lim AK, Rhodes S, Cowan K, et al. Joint production of research priorities to improve the lives of those with childhood onset conditions that impair learning: the James Lind Alliance Priority Setting Partnership for 'learning difficulties'. BMJ Open 2019;9:e028780. 10.1136/bmjopen-2018-028780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lavigne M, Birken CS, Maguire JL, et al. Priority setting in paediatric preventive care research. Arch Dis Child 2017;102:748–53. 10.1136/archdischild-2016-312284 [DOI] [PubMed] [Google Scholar]
- 27.Hauck Y, Kelly RG, Fenwick J. Research priorities for parenting and child health: a Delphi study. J Adv Nurs 2007;59:129–39. 10.1111/j.1365-2648.2007.04278.x [DOI] [PubMed] [Google Scholar]
- 28.Garbutt JM, Leege E, Sterkel R, et al. What are parents worried about? health problems and health concerns for children. Clin Pediatr 2012;51:840–7. 10.1177/0009922812455093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mathieson A, Grande G, Luker K. Strategies, facilitators and barriers to implementation of evidence-based practice in community nursing: a systematic mixed-studies review and qualitative synthesis. Prim Health Care Res Dev 2019;20:e6. 10.1017/S1463423618000488 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-047919supp001.pdf (45.7KB, pdf)
Data Availability Statement
Data are available on reasonable request. The research priorities codebook, containing the raw research priorities responses, is available on reasonable request from the corresponding author.