IN RESPONSE:
Dr. Spence provides an insightful comment on our finding that accepted standards for cardiovascular risk assessment underestimate risk for persons in disadvantaged neighborhoods. The explanation offered is that certain behavioral risk exposures (for example, passive smoking and unhealthy diet) are simply more common in disadvantaged neighborhoods, are difficult to accurately assess, and may be largely responsible for the discrepancy in observed versus estimated risk. We contend that the disparities observed in outcomes are too extreme to simply be the result of the distribution of such risk factors. If passive smoking were to explain the difference in observed versus expected cardiovascular risk in patients from disadvantaged neighborhoods, then a counter-factual argument could be made that risk is more accurately measured among smokers from these neighborhoods. To examine this relationship, we conducted a supplemental analysis of smokers from our original sample, who presumably would not be affected by passive smoking.
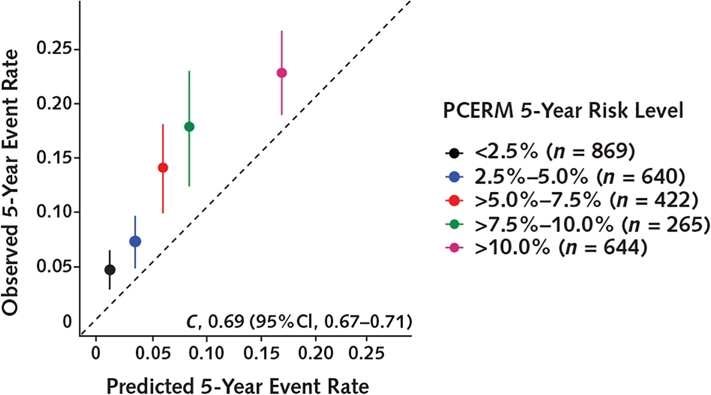
The Figure shows the calibration of the Pooled Cohort Equations Risk Model for the subpopulation of 2867 patients who were smokers and resided in the top 25% most disadvantaged neighborhoods. Results are consistent with the overall prior published results-cardiovascular risk remains grossly underestimated. These results support the idea that traditional risk factors alone are insufficient to explain contextual disparities in risk and that risk is fundamentally influenced by neighborhood disadvantage and other related environmental exposures.
Figure.
Prognostic accuracy of the PCERM among smokers in the top 25% most disadvantaged neighborhoods.
C = concordance index; PCERM = Pooled Cohort Equations Risk Model.
Considerable existing research supports this claim (1). Air particulate has been linked to the onset and progression of cardiovascular disease (2), and evidence indicates a causal effect of unemployment and other social factors leading to myocardial infarction (3). However, much remains to be learned about how a wide range of social, behavioral, and environmental constructs-including availability of healthy food, physical environments conducive to exercise, air quality, chronic stress, violence, racism, and unemployment-might influence risk for cardiovascular events. Until these underlying mechanisms are better understood, we contend that use of neighborhood disadvantage as a surrogate risk indicator seems reasonable.
Footnotes
Disclosures: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M16-2543.
Contributor Information
Adam T. Perzynski, MetroHealth System, Cleveland, Ohio.
Michael B. Rothberg, Cleveland Clinic, Cleveland, Ohio.
Neal V. Dawson, Case Western Reserve University, Cleveland, Ohio.
Claudia J. Coulton, Case Western Reserve University, Cleveland, Ohio.
Jarrod E. Dalton, Cleveland Clinic, Cleveland, Ohio.
References
- 1.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav 2010;51 Suppl:S28–40. 10.1177/0022146510383498 [DOI] [PubMed] [Google Scholar]
- 2.Du Y, Xu X, Chu M, Guo Y, Wang J. Air particulate matter and cardiovascular disease: the epidemiological, biomedical and clinical evidence. J Thorac Dis. 2016;8:E8–19. 10.3978/j.issn.2072-1439.2015.11.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, et al. ; American Heart Association Council on Quality of Care and Outcomes Research, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, and Stroke Council. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–98. 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]