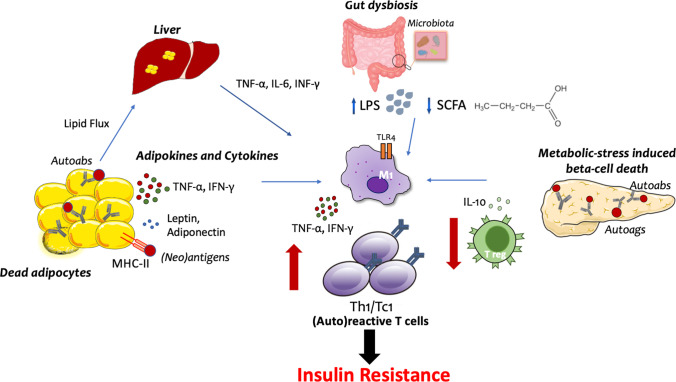
Figure 1.
Potential mechanisms of engagement of autoreactive T cells in insulin resistance. Schematic view of the proposed mechanisms involved in the generation of autoreactive T cells in the context of insulin resistance: (i) In the visceral fat, accumulation of fat depot induces adipocyte death and release of pro-inflammatory soluble hormones and cytokines. This is accompanied by the upregulation of MHC-II on adipocytes which turn into antigen-presenting cells; (ii) Intestinal dysbiosis, by promoting translocation of lipopolysaccharide (LPS) and bacteria metabolites in the systemic circulation, induces autoreactive immune responses in the gut as well as in other tissues; (iii) In the pancreas, metabolic-stress and inflammation induce beta cell death with the generation of conventional and neo-antigens; (iv) Local and systemic inflammation is fostered by the excessive accumulation of lipids in the liver. All these pathways lead to TLR-4-mediated activation of tissue resident macrophages, enhanced presentation of autoantigens, and consequent development of (auto)reactive T cells with a type 1 T helper (Th1) or cytotoxic T cell (Tc1) phenotype. This is accompanied by the reduction of regulatory T cell subsets and cytokines, such as Treg and IL-10, which contribute to the development of resistance to the insulin action in insulin-sensitive tissues. Autoags: autoantigens; Autoabs: autoantibodies