Abstract
Objective:
To synthesize the growing body of literature about the role of social determinants of health (SDoH) in asthma and asthma disparities.
Data Sources:
A pubmed.gov search was performed to identify published literature on SDoH, asthma, asthma disparities, and race/ethnicity. CDC current asthma statistics were reviewed.
Study Selections:
Relevant articles on SDoH, asthma, asthma disparities, and race/ethnicity were reviewed in detail.
Results:
Black and Latinx Americans have a higher asthma prevalence and greater asthma morbidity than White Americans and also bear a disproportionate burden of SDoH. Inequities in SDoH are rooted in structural racism, population-level injustices that affect the socioeconomic status, physical environment, and health care access/quality of Black and Latinx Americans. There is evidence that racial/ethnic inequities in SDoH, such as socioeconomic status, neighborhood environment, housing, environmental exposures, and health care access/quality, contribute to excess burden of asthma prevalence/incidence, morbidity, exacerbations, and abnormal lung function among certain racial/ethnic populations. Additionally, Black and Latinx communities experience high levels of chronic stress, which may increase asthma risk through direct effects on the immune system and hypothalamic-pituitaryadrenocortical activation. Chronic stress may also mediate the effects of SDoH on asthma.
Conclusion:
Although there is clear evidence linking SDoH to excess asthma risk and implicating SDoH in asthma disparities, the extent to which asthma disparities are explained by inequities in SDoH, and the relative contributions of each of these SDoH to asthma disparities, remain unclear. This knowledge is needed to effectively develop and test systems-level interventions targeting SDoH, with the ultimate goal of meaningfully reducing racial/ethnic asthma disparities.
Keywords: Asthma, Social determinants of health, Asthma disparities, Racial and ethnic disparities, Racism, Structural racism
Introduction
Social determinants of health (SDoH) are defined by the World Health Organization as the “non-medical factors that influence health outcomes,” which can include the “conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.”1 There is a growing appreciation of the substantial impact SDoH, such socioeconomic status, physical environment such as housing and air pollution exposure, and barriers to high quality health care, have on asthma generally, and racial and ethnic asthma disparities in particular.
Asthma affects more than 25 million children and adults living in the United States (US),2 but some racial and ethnic minority populations are disproportionately affected by asthma, and the scientific literature suggests SDoH play an important role in this disparity. In the US, Non-Latinx (NL) Black individuals have a higher prevalence of asthma (10.6%) compared to NL Whites (7.7%), NL Asians (3.8%), and Latinx individuals (6.6%), with the exception of Puerto Rican and Dominican Americans.2–4 Additionally, Black Americans have higher rates of emergency room (ER) visits, hospitalizations, and death due to asthma than White Americans.3 Latinx of Afro-Caribbean descent, e.g., Puerto Ricans and Dominicans have higher asthma prevalence, more frequent asthma exacerbations, and higher rates of ER visits due to asthma than White individuals.4–6 Other Latinx populations have tended to have a lower burden of asthma in the past, but recent data show that asthma prevalence is increasing among Mexican American children and that the rates hospitalization for asthma among Mexican American children are higher than White children and similar to the hospitalization rates for Black children.7 In this review, we focus primarily on the SDoH of Black and Latinx populations as compared with White individuals, as more has been published regarding disparities between these racial and ethnic populations. However, other minority racial and ethnic groups such as Asian Americans, Pacific Islanders, Native Americans, and multiracial Americans also experience inequities, which influence their health, and immigrants may also contend with language and cultural barriers, which can increase their risk for poor health outcomes.8,9 More research is needed to bring to light unique SDoH facing other racial and ethnic minority populations.
Upstream of the differences in SDoH between different racial and ethnic groups in the United States is the historic and ongoing racism which affects the everyday lives of millions of individuals. Structural and individual racism experienced by Black and Latinx Americans influence socioeconomic status, physical environment, and health care access and quality, all of which in turn affect asthma, thereby implicating racism as a cause of asthma prevalence and morbidity. In order to meaningfully shrink racial and ethnic disparities in asthma prevalence, morbidity, and mortality, SDoH must be addressed directly in asthma research, care delivery, and advocacy. The purpose of this paper is to describe how differences in SDoH contribute to asthma disparities in the US (Figure 1).
Figure 1.
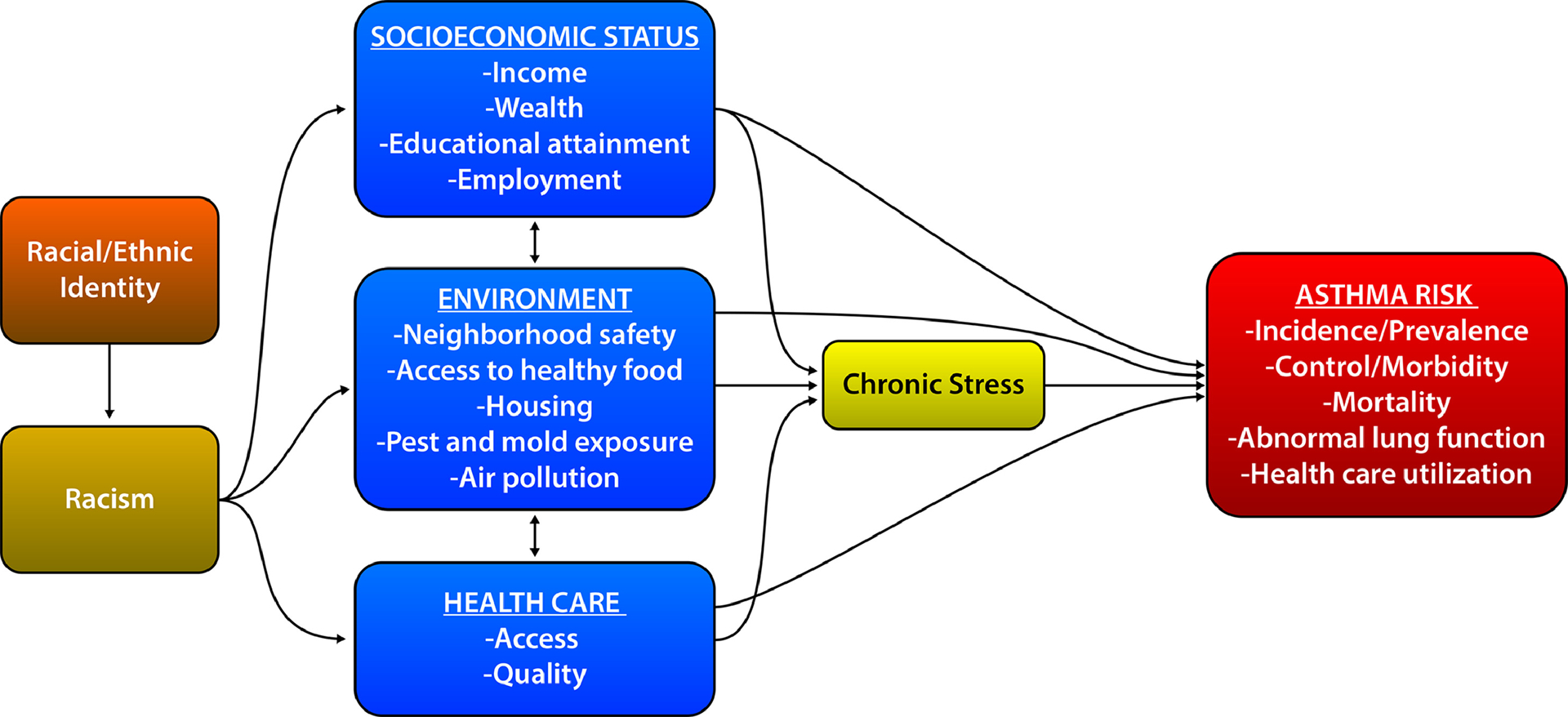
The relationship of racism, SDoH, and asthma risk and disparity in the United States. SDoH, social determinants of health.
Social Determinants of Asthma
Racism
Race and ethnicity are self-identified social constructs. The American Sociological Association defines race as “physical differences that groups and cultures consider socially significant” and ethnicity, such as Hispanic or Latinx ethnicity, as “shared culture, such as language, ancestry, practices, and beliefs.”10 Racism is the prejudicial treatment of individuals and communities based on the belief that one race or ethnic group is superior or inferior to another. Racism structures and affords opportunities and assigns value and worth based on an individual’s self-identified race or ethnicity. Racism occurs at the individual and population level. Structural racism, which is population-level racism, exists in our social, legal, economic, medical, housing, criminal justice, and political systems and unfairly denies opportunity and disadvantages racial and ethnic minority populations.11 In this review we will focus on structural racism and its effects on population-level asthma disparities, however, individual or interpersonal racism can also have negative effects on health.11
There is now a clear recognition that racism has negative effects on health and directly leads to health inequities, and professional societies such as the American College of Physicians, the American Academy of Pediatrics, and the American Medical Association have recently come out with strong statements declaring racism a threat to public health.12–14 A recent review in The Lancet provides evidence for structural racism’s direct effects on health inequalities through discriminatory practices in housing, education, income, employment, environmental exposures, health care, politics, and the legal system.11 The effects of structural racism on health are supported by the fact that racial and ethnic minority populations having overall higher disease prevalence and burden that are not entirely explained by socioeconomic status. For example, Black Americans have a lower life expectancy than White Americans at all income and education levels.15 Racism acts on health through multiple pathways, including socioeconomic status (SES), environment, and health care access and quality, all of which are SDoH risk factors for increased asthma incidence, prevalence, morbidity, and mortality (Figure 1).
Socioeconomic Status
Socioeconomic status is a broad marker of an individual’s, family’s, or community’s social standing. Socioeconomic status affects the ability to access and attain basic needs, such as housing, food, and education, and amass the resources and wealth needed to affect one’s upward mobility in society. Researchers often attempt to capture SES through income, highest educational degree obtained, occupation, type of health insurance, or zip code. However, these markers of SES often fail to capture the entire picture of SDoH, as they do not account for other aspects of SES such as wealth, quality of education, employment benefits, and material hardship. Below we describe income, wealth, education, and employment as SDoH and their roots in structural racism and link to asthma disparities.
Income and Wealth
Low income has been repeatedly linked to increased asthma prevalence, exacerbations, hospitalizations and ICU admission.16–19 Black and Latinx families earn significantly less money than White families,20 with the US Census Bureau reporting in 2018 a median household income of $41,361 for Black families, $51,450 for Latinx families, and $70,642 for White families.21 In addition to higher incomes, White families also have more family wealth or net financial worth, which takes into account all assets including money, property, business ownership, and possessions. In 2019, White families reported a median wealth of $188,200, Black families reported $24,100, and Latinx families reported $36,100.22 Black and Latinx homeownership, the major source of intergenerational wealth, continues to trail White homeownership, with the Black-White homeownership gap increasing over the last 30 years.23 Homeownership inequities today can be traced back to structural racism in the housing sector, including racial covenants dating back to 1910, redlining, discriminatory lending practices and other types of housing discrimination, which still exist today.24,25 Compounding this wealth gap is that homes in primarily Black neighborhoods are devalued compared to homes in neighborhoods with <1% Black residents.26
There is thus strong evidence that the income and wealth gaps between White Americans and racial and ethnic minority populations are rooted in structural racism, and these measures of socioeconomic status as SDoH are strongly linked to asthma. In 2019, the Centers for Disease Control and Prevention (CDC) reported an asthma prevalence of 11.8% for individuals with a family income below 100% of the poverty threshold, 8.5% for those with a family income 100% to <250% of the poverty threshold, 7.3% for those with a family income 250% to <450% of the poverty threshold, and finally 5.9% for those with a family income of ≥450% of the poverty threshold,2 demonstrating a dose response relationship between poverty level and asthma prevalence. Similarly, Keet et. al. found a 7% increase in the odds of prevalent asthma for each one-unit decrease in the household income to poverty ratio.18 Low income also is a risk factor for asthma treatment failure, asthma exacerbations, and ICU admission for asthma.16,17 In one study, adults with a household income of <$50,000 had a 1.6-fold higher rate of asthma treatment failure and 2.0-fold higher rate of asthma exacerbations compared with those with a household income ≥$50,000.16 In a study of characteristics of life-threatening asthma, children living in extreme poverty (household income <$10,000) had 125% higher odds of having a prior ICU admission for asthma.17 Additionally, home ownership is associated with a decreased odds of ER visit for asthma in children,27 highlighting wealth in addition to income as a risk factor for asthma morbidity.
Low income’s link to prevalent asthma and asthma morbidity is likely multifactorial, as low income influences other SDoH such as education, housing, exposure to pests and pollution, and access to food and health care, all of which are risk factors for asthma and asthma morbidity which are addressed below.
Education and Employment
Wealth and property values are also directly linked to education as the main source of funding for public education in the US is property taxes. Educational structural racism is highlighted by the fact that Black and Latinx children are more likely to attend schools in areas with concentrated poverty.28 Data from the National Assessment of Educational Progress analyzed by the Economic Policy Institute showed that in 2017 Black children were five times more likely to attend racially-segregated schools and twice as likely to attend schools in areas of high poverty compared to White children.29 In 2016, researchers at Stanford concluded that attending a school with high numbers of low-income students is the biggest driver of the racial educational achievement gap.30 These continued practices contribute to White children continuing to outperform Black and Latinx children in math and reading in elementary school and middle school31 and lead to higher college graduation rates in Whites (64%) compared to Latinx (54%) and Black Americans (40%).32 Educational inequalities have been linked back to underinvestment in early education and low quality early education,33 which are perpetuated by lower home values and concentrated poverty.
Lower educational attainment contributes to limited health literacy, which directly affects health. The CDC defines individual health literacy as “the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others.”34 In a 2005 systematic review on limited health literacy, low education, low income, and Black race were all associated with limited health literacy.35 A 2019 article on the effect of low health literacy on pediatric health summarized the impact of low health literacy on pediatric asthma, describing how low health literacy leads to decreased asthma understanding and the perceived increased need for asthma medications, the inability to follow an asthma action plan, lower likelihood of being treated by an asthma specialist, poorer asthma control, more missed days of school, and increased ER visits and hospitalizations for asthma.36 In a recent analysis of adults living in Chicago with persistent asthma, low health literacy and low income mediated the association between race/ethnicity and lower quality of life and ER visits due to asthma.37
Connected to both low income and lower educational achievement, racial and ethnic minority populations have reduced employment opportunity, which is reflected clearly in the current US unemployment rates which continue to be higher for Black and Latinx Americans than White Americans.38 Lack of employment benefits, such as paid leave, sick time, and employer health insurance, contributes to health inequities.11 Additionally, educational inequalities continue to perpetuate income inequalities which in turn drive asthma disparities. Taken together, educational structural racism, which keeps Black and Latinx children in segregated schools with concentrated poverty, leads to lower educational achievement and employment opportunities and benefits, which in turn affects health literacy and asthma care, control, acute visits, and quality of life.
Environment
Along with SES, environmental exposures affect asthma risk and are important SDoH. Low-income and racial and ethnic minority families live in neighborhoods with increased exposure to violence, decreased access to healthy food (food deserts), and increased exposure to poor housing, pest infestation, mold, and pollution.
Neighborhood Safety
Low-income and racial and ethnic minority communities experience more exposure to neighborhood violence, which is another manifestation of the effects of structural racism on concentrated poverty and racial segretation.39–41 Children in low-income and disadvantaged communities are frequently exposed to violence, with Black youth having the highest level of exposure to neighborhood violence.42,43 There is evidence that prenatal exposure to neighborhood violence could increase the risk of asthma as a 2014 study out of Boston found that maternal report of increased community violence during pregnancy was associated with increased risk of wheeze at age 2 in the offspring.44 Furthermore, violent neighborhood crime has been associated with increased asthma prevalence and morbidity.45,46 In a study of children with asthma living in Chicago, the annual neighborhood crime rate was associated with increased asthma prevalence, with neighborhoods with a high incidence of violent crime having a 27% increased odds of prevalent neighborhood asthma compared with neighborhoods with low incidence of violent crime, independent of neighborhood race/ethnicity.45 In a separate study of Mexican American children in Chicago, living in a neighborhood with increased property and violent crimes was associated with a child having increased odds of parent-reported wheezing, lifetime asthma, and ER use and hospitalization due to asthma.46 The exact mechanism by which neighborhood violence increases the risk of asthma and asthma morbidity is not clear, but some research suggests that the associations between neighborhood violence and asthma may be mediated by chronic stress.47,48
Access to Affordable, Healthy Food
Multiple inequities also exist for racial and ethnic minority populations when it comes to access and affordability of healthy food. Compared to high-income communities, low-income communities have fewer healthy food options and poorer quality produce49 and low-income Black families are less likely to live in neighborhood with access to affordable healthy food.50 Additionally, healthy food is more expensive and low-income family budgets are not sufficient to afford healthy food, which contributes to racial inequities in optimal nutrition and diet quality.51 In observational studies, healthier foods, such as diets rich in fruits and vegetables, have been associated with fewer asthma symptoms and higher lung fuction.52 Lack of affordable healthy food has also been linked to obesity which is associated with asthma incidence and asthma morbidity.53 Proposed mechanisms for how healthier diets could result in decreased incident asthma and improved asthma morbidity include anti-inflammatory effects, changes in the intestinal microbiome, and reduced risk of obesity.52
Housing and Exposure to Pest, Mold, and Pollution
Poor housing quality and home disrepair have been associated with risk of childhood asthma and asthma morbidity.27,54,55 Structural racism in lending and other housing discrimination, which lead to the aforementioned disparities in home ownership, also result in racial and ethnic minority populations being more likely to live in poor quality housing. A disproportionate number of Black and Latinx families live in housing classified as moderately or severely substandard.56 Additionally, children with asthma living in low-income communities are disproportionately exposed to pest allergens such as mouse and cockroach57–60 since poor housing conditions contribute to pest infestation.61–63 Pest allergen exposure has been repeatedly linked to risk of asthma, asthma prevalence, morbidity and abnormal lung function.59,64–67 Recent data suggests that pest allergen exposure may lead to reduced lung function growth,68 which has implications for future risk of adult lung disease and mortality.69–72 Similarly, poor housing quality and housing disrepair is associated with risk of exposure to mold73 and exposure to mold is associated with childhood wheeze and asthma prevalence as well as asthma morbidity.74–77 Moreover, children in racial and ethnic minority urban communities are also exposed to higher levels of indoor air pollution, which is associated with asthma symptoms.78
Similarly, structural racism has also resulted in inequities in outdoor air pollution exposure, as persons living in poverty, Black residents, and individuals with lower education are more likely to be exposed to higher levels of outdoor air pollution.79–82 An ecological study of eight California cities found higher diesel particle emissions in historically redlined communities.83 These historically redlined communities were also found to have a 2.4 fold increase in age-adjusted ER visits for asthma compared with historically lowest lending risk neighborhoods.83 Outdoor air pollution is associated with incident asthma, asthma morbidity, and lung function decline.52 Although there is a lack of studies that directly estimate the effects of these environmental injustices on disparities in asthma prevalence, morbidity, and lung function, the fact that Black and Latinx individuals are at greater risk of allergen, mold, and pollutant exposures, which are in turn linked to increased asthma prevalence and exacerbations, strongly suggests that the physical environment contributes to racial and ethnic asthma disparities.
Health Care Access and Quality
In addition to inequities in SES and environmental exposures, structural and individual racism results in racial and ethnic minority communities experiencing disparities in asthma health care. Black and Latinx patients are more likely to be uninsured than White patients84 and Black and Latinx families are more likely to live in zip codes with primary care physician shortages,85 limiting their access to asthma health care. Even among individuals with the same military health care insurance, Black and Latinx children were significantly less likely to see a specialist for asthma than White children.86 Similarly, barriers to asthma specialty care and health care access lead to the underuse of asthma biologics in Black and Latinx patients. A 2021 study found patients with public insurance were less like to be prescribed a biologic for asthma treatment.87 Additionally, among patients with public insurance, racial and ethnic minority patients were less likely to be prescribed an asthma biologic compared with White patients.87 Lack of health insurance, access to primary care, and fewer referrals to asthma specialists all result in higher ER utilization for asthma, increased school and work absences, decreased provider consistency, uncontrolled asthma, and overall worse asthma care.88,89
Stress
Inequities in SDoH influence asthma risk and morbidity through multiple mechanisms as discussed above and, furthermore, these SDoH contribute to chronic stress, which may be another mechanism by which SDoH cause asthma disparities. Families living in poverty and racial and ethnic minority populations experience higher levels of stress from many sources including income instability, lower education, fewer assets, barriers to employment, food insecurity, higher rates of incarceration, social disadvantage, and exposure to violence.90 Chronic stress is proposed to have direct effects on asthma through chronic hypothalamic-pituitary-adrenocortical activation, which leads to a decrease in β2 adrenergic and glucocorticoid receptors and, thus, a decreased responsiveness to asthma medication and an increase in asthma symptoms.91 Maternal prenatal stress has been associated with altered and allergic immune responses and incident asthma in the offspring,92,93 with high stress being associated with an increased IL-13 response and a decreased IFN-γ response to allergen/mitogen stimulation in cord blood mononuclear cells,92 providing evidence for stress as a risk factor for a Th2 allergic phenotype. Early life (age <3 years) exposure to environmental stressors and maternal diagnosis of depression and anxiety is also associated with asthma diagnosis.93 High levels of chronic stress in children and adults have been associated with increased asthma exacerbations, decreased asthma control, increased hospitalizations, decreased quality of life, and decreased lung function.47,48,94
Conclusion
Historical and present-day structural racism has resulted in Black and Latinx communities experiencing disproportionate SDoH, including poverty, inequities in education and employment, poor housing quality, greater risk of exposure to pests, mold, and pollution, unequal health care access and quality, and high levels of chronic stress. All of these SDoH are implicated in asthma prevalence/incidence, morbidity, exacerbations, and abnormal lung function, which suggests that they are also likely a major cause of asthma disparities. Importantly, asthma exacerbations are associated with decline in lung function,95,96 which is a risk for adult lung disease and mortality,69–72 suggesting that SDoH that are implicated in exacerbations may adversely affect lung growth. There is also evidence that environmental exposures, including pest allergen and air pollution, impede lung growth, which suggests that the physical environment, and possibly other SDoH, may have far-reaching effects on children, potentially increasing the risk of COPD and even mortality in adulthood. In fact, observational data suggest that intervening on environmental exposures, including pest allergen exposure68 and outdoor air pollution,97 could alter lung function trajectory in childhood and decrease the risk of abnormal lung function in adulthood. Future research should seek to better understand the long-term effects of SDoH, including their role in racial and ethnic disparities in lung health in adulthood.
While these SDoH are known to contribute to asthma risk within racial and ethnic minority populations, there are few, if any, studies that have sought to determine how much they explain differences in asthma burden between racial/ethnic populations, i.e., disparities. Instead, the majority of the literature on these SDoH and their associations with asthma examines their effects on asthma within an ethnic minority population. Understanding the degree to which these SDoH contribute to disparities, and which ones contribute most, is critical for developing and testing systems-level interventions targeting SDoH and structural racism (Table 1), but would require studies designed explicitly for this purpose. Information from such studies would help inform how best to design and target policies aimed at reducing racial and ethnic asthma disparities.
Table 1:
Knowledge gaps in understanding the effects of SDoH on racial and ethnic asthma disparities
| - Degree to which SDoH contribute to racial and ethnic asthma disparities |
| - Which SDoH contribute most to racial and ethnic asthma disparities |
| - Mechanisms by which SDoH cause asthma disparities |
| - What are the most impactful approaches to mitigating economic barriers to asthma care and self-management |
| - Which environmental exposures should be prioritized for targeting to reduce racial and ethnic asthma disparities |
| - What are the most impactful approaches to improving health care access and quality for racial and ethnic minority populations |
| - Which individual-level and systems-level interventions are most effective at reducing racial and ethnic asthma disparities |
Funding source:
Dr. Grant is supported by the American Academy of Allergy, Asthma, and Immunology Foundation Faculty Development Award, the Johns Hopkins University School of Medicine Clinician Scientist Career Development Award, and the University of Wisconsin, Madison/National Institutes of Health (5UH3OD023282). Emily Croce is supported by the National Institute of Nursing Research of the National Institutes of Health (T32NR019035) and a Pediatric Dermatology Research Alliance Research Fellowship. Dr. Matsui is supported by the National Institutes of Health (K24AI114769, R01ES023447, R01ES026170). The content is solely the responsibility of the authors and does not necessarily represent the official views of any of the funding sources.
Abbreviations/Acronyms:
- CDC
Centers for Disease Control and Prevention
- COPD
Chronic obstructive pulmonary disease
- ER
Emergency room
- ICU
Intensive care unit
- IFN-γ
Interferon gamma
- IL-13
Interleukin 13
- NL
Non-Latinx
- SDoH
Social determinants of health
- SES
Socioeconomic status
- Th2
T helper 2
- US
United States
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: none
References
- 1.Social determinants of health. Accessed June 17, 2021. https://www.who.int/westernpacific/health-topics/social-determinants-of-health
- 2.Most Recent National Asthma Data | CDC. Published April 7, 2021. Accessed June 15, 2021. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm
- 3.Moorman JE, Rudd RA, Johnson CA, et al. National surveillance for asthma--United States, 1980–2004. MMWR Surveill Summ. 2007;56(8):1–54. [PubMed] [Google Scholar]
- 4.Rosser FJ, Forno E, Cooper PJ, Celedón JC. Asthma in Hispanics. An 8-Year Update. Am J Respir Crit Care Med. 2014;189(11):1316–1327. doi: 10.1164/rccm.201401-0186PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dumanovsky T, Matte TD. Variation in Adult Asthma Prevalence in Hispanic Subpopulations in New York City. Journal of Asthma. 2007;44(4):297–303. doi: 10.1080/02770900701344140 [DOI] [PubMed] [Google Scholar]
- 6.Patel MM, Quinn JW, Jung KH, et al. Traffic density and stationary sources of air pollution associated with wheeze, asthma, and immunoglobulin E from birth to age 5 years among New York City children. Environmental Research. 2011;111(8):1222–1229. doi: 10.1016/j.envres.2011.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zahran HS. Vital Signs: Asthma in Children — United States, 2001–2016. MMWR Morb Mortal Wkly Rep. 2018;67. doi: 10.15585/mmwr.mm6705e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Misra S, Kwon SC, Abraído-Lanza AF, Chebli P, Trinh-Shevrin C, Yi SS. Structural Racism and Immigrant Health in the United States. Health Educ Behav. 2021;48(3):332–341. doi: 10.1177/10901981211010676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abraído-Lanza AF, Echeverría SE, Flórez KR. Latino Immigrants, Acculturation, and Health: Promising New Directions in Research. Annu Rev Public Health. 2016;37:219–236. doi: 10.1146/annurev-publhealth-032315-021545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Race and Ethnicity. American Sociological Association. Accessed July 8, 2021. https://www.asanet.org/topics/race-and-ethnicity
- 11.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 12.Serchen J, Doherty R, Atiq O, Hilden D. Racism and Health in the United States: A Policy Statement From the American College of Physicians. Annals of Internal Medicine. 2020;173(7):556–557. doi: 10.7326/M20-4195 [DOI] [PubMed] [Google Scholar]
- 13.Trent M, Dooley DG, Dougé J, Health S on A, Pediatrics C on C, Adolescence CO. The Impact of Racism on Child and Adolescent Health. Pediatrics. 2019;144(2). doi: 10.1542/peds.2019-1765 [DOI] [PubMed] [Google Scholar]
- 14.New AMA policy recognizes racism as a public health threat. American Medical Association. Accessed July 8, 2021. https://www.ama-assn.org/press-center/press-releases/new-ama-policy-recognizes-racism-public-health-threat [Google Scholar]
- 15.Williams DR, Lawrence JA, Davis BA. Racism and Health: Evidence and Needed Research. Annu Rev Public Health. 2019;40(1):105–125. doi: 10.1146/annurev-publhealth-040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cardet JC, Louisias M, King TS, et al. Income is an independent risk factor for worse asthma outcomes. Journal of Allergy and Clinical Immunology. 2018;141(2):754–760.e3. doi: 10.1016/j.jaci.2017.04.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bollinger ME, Butz A, Tsoukleris M, Lewis-Land C, Mudd S, Morphew T. Characteristics of inner-city children with life-threatening asthma. Annals of Allergy, Asthma & Immunology. 2019;122(4):381–386. doi: 10.1016/j.anai.2019.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keet CA, McCormack MC, Pollack CE, Peng RD, McGowan E, Matsui EC. Neighborhood poverty, urban residence, race/ethnicity, and asthma: Rethinking the inner-city asthma epidemic. Journal of Allergy and Clinical Immunology. 2015;135(3):655–662. doi: 10.1016/j.jaci.2014.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Litonjua AA, Carey VJ, Weiss ST, Gold DR. Race, socioeconomic factors, and area of residence are associated with asthma prevalence. Pediatric Pulmonology. 1999;28(6):394–401. doi: [DOI] [PubMed] [Google Scholar]
- 20.Bureau UC. Income and Poverty in the United States: 2019. The United States Census Bureau. Accessed June 18, 2021. https://www.census.gov/data/tables/2020/demo/income-poverty/p60-270.html [Google Scholar]
- 21.Real Median Household Income by Race and Hispanic Origin: 1967 to 2018. Accessed July 8, 2021. https://www.census.gov/content/dam/Census/library/visualizations/2019/demo/p60-266/figure2.pdf
- 22.Disparities in Wealth by Race and Ethnicity in the 2019 Survey of Consumer Finances. Accessed June 18, 2021. https://www.federalreserve.gov/econres/notes/feds-notes/disparities-in-wealth-by-race-and-ethnicity-in-the-2019-survey-of-consumer-finances-20200928.htm
- 23.Rebounds in Homeownership Have Not Reduced the Gap for Black Homeowners | Joint Center for Housing Studies. Accessed June 16, 2021. https://www.jchs.harvard.edu/blog/rebounds-in-homeownership-have-not-reduced-the-gap-for-black-homeowners
- 24.BOCK J. “Apartheid, Baltimore Style” City Housing Suit and History of Bias. baltimoresun.com. Accessed June 16, 2021. https://www.baltimoresun.com/news/bs-xpm-1995-02-05-1995036002-story.html
- 25.Lynch EE, Malcoe LH, Laurent SE, Richardson J, Mitchell BC, Meier HCS. The legacy of structural racism: Associations between historic redlining, current mortgage lending, and health. SSM - Population Health. 2021;14:100793. doi: 10.1016/j.ssmph.2021.100793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harshbarger AMP Jonathan Rothwell, and David. The devaluation of assets in Black neighborhoods. Brookings. Published November 27, 2018. Accessed June 18, 2021. https://www.brookings.edu/research/devaluation-of-assets-in-black-neighborhoods/ [Google Scholar]
- 27.Hughes HK, Matsui EC, Tschudy MM, Pollack CE, Keet CA. Pediatric Asthma Health Disparities: Race, Hardship, Housing, and Asthma in a National Survey. Acad Pediatr. 2017;17(2):127–134. doi: 10.1016/j.acap.2016.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.School poverty | National Equity Atlas. Accessed July 9, 2021. https://nationalequityatlas.org/indicators/School_poverty#/
- 29.Schools are still segregated, and black children are paying a price. Economic Policy Institute. Accessed July 9, 2021. https://www.epi.org/publication/schools-are-still-segregated-and-black-children-are-paying-a-price/ [Google Scholar]
- 30.Patterns and Trends in Racial/Ethnic and Socioeconomic Academic Achievement Gaps. Accessed July 9, 2021. https://cepa.stanford.edu/sites/default/files/reardon%20robinson-cimpian%20weathers%20HREFP%20chapter%20april2014.pdf
- 31.de Brey C, Musu L, McFarland J, et al. Status and Trends in the Education of Racial and Ethnic Groups 2018. :228. [Google Scholar]
- 32.Indicator 23: Postsecondary Graduation Rates. Accessed June 18, 2021. https://nces.ed.gov/programs/raceindicators/indicator_red.asp
- 33.Yang J, Qiu M. The impact of education on income inequality and intergenerational mobility. China Economic Review. 2016;37:110–125. doi: 10.1016/j.chieco.2015.12.009 [DOI] [Google Scholar]
- 34.CDC. What is health literacy? Take action. Find out. Centers for Disease Control and Prevention. Published May 19, 2021. Accessed July 30, 2021. https://www.cdc.gov/healthliteracy/learn/index.html
- 35.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The Prevalence of Limited Health Literacy. J Gen Intern Med. 2005;20(2):175–184. doi: 10.1111/j.1525-1497.2005.40245.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morrison AK, Glick A, Yin HS. Health Literacy: Implications for Child Health. Pediatrics in Review. 2019;40(6):263–277. doi: 10.1542/pir.2018-0027 [DOI] [PubMed] [Google Scholar]
- 37.Seibert RG, Winter MR, Cabral HJ, Wolf MS, Curtis LM, Paasche-Orlow MK. Health Literacy and Income Mediate Racial/Ethnic Asthma Disparities. Health Lit Res Pract. 2019;3(1):e9–e18. doi: 10.3928/24748307-20181113-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Unemployment Rates | U.S. Department of Labor. Accessed June 18, 2021. https://www.dol.gov/agencies/wb/data/latest-annual-data/employment-rates
- 39.Lee MR. Concentrated Poverty, Race, and Homicide. The Sociological Quarterly. 2000;41(2):189–206. [Google Scholar]
- 40.Hannon L, DeFina R. Violent Crime in African American and White Neighborhoods: Is Poverty’s Detrimental Effect Race-Specific? Journal of Poverty. 2005;9(3):49–67. doi: 10.1300/J134v09n03_03 [DOI] [Google Scholar]
- 41.Harrell E, Smiley-McDonald H. Household Poverty and Nonfatal Violent Victimization, 2008–2012. Published online 2014:18. [Google Scholar]
- 42.Sheehan K, DiCara JA, LeBailly S, Christoffel KK. Children’s exposure to violence in an urban setting. Arch Pediatr Adolesc Med. 1997;151(5):502–504. doi: 10.1001/archpedi.1997.02170420072012 [DOI] [PubMed] [Google Scholar]
- 43.Browning CR, Calder CA, Ford JL, Boettner B, Smith AL, Haynie D. Understanding Racial Differences in Exposure to Violent Areas: Integrating Survey, Smartphone, and Administrative Data Resources. Ann Am Acad Pol Soc Sci. 2017;669(1):41–62. doi: 10.1177/0002716216678167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chiu Y-HM, Coull BA, Sternthal MJ, et al. Effects of prenatal community violence and ambient air pollution on childhood wheeze in an urban population. J Allergy Clin Immunol. 2014;133(3):713–722.e4. doi: 10.1016/j.jaci.2013.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gupta RS, Zhang X, Springston EE, et al. The association between community crime and childhood asthma prevalence in Chicago. Annals of Allergy, Asthma & Immunology. 2010;104(4):299–306. doi: 10.1016/j.anai.2009.11.047 [DOI] [PubMed] [Google Scholar]
- 46.Eldeirawi K, Kunzweiler C, Rosenberg N, et al. Association of neighborhood crime with asthma and asthma morbidity among Mexican American children in Chicago, Illinois. Annals of Allergy, Asthma & Immunology. 2016;117(5):502–507.e1. doi: 10.1016/j.anai.2016.09.429 [DOI] [PubMed] [Google Scholar]
- 47.Jones BL, Staggs V, Woods-Jaeger B. Chronic stress exposure among young African American children with asthma: Racism is a factor. Annals of Allergy, Asthma & Immunology. 2019;123(5):507–508. doi: 10.1016/j.anai.2019.08.023 [DOI] [PubMed] [Google Scholar]
- 48.Landeo-Gutierrez J, Forno E, Miller GE, Celedón JC. Exposure to Violence, Psychosocial Stress, and Asthma. Am J Respir Crit Care Med. 2020;201(8):917–922. doi: 10.1164/rccm.201905-1073PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Andreyeva T, Blumenthal DM, Schwartz MB, Long MW, Brownell KD. Availability And Prices Of Foods Across Stores And Neighborhoods: The Case Of New Haven, Connecticut. Health Affairs. 2008;27(5):1381–1388. doi: 10.1377/hlthaff.27.5.1381 [DOI] [PubMed] [Google Scholar]
- 50.Bower KM, Thorpe RJ, Rohde C, Gaskin DJ. The Intersection of Neighborhood Racial Segregation, Poverty, and Urbanicity and its Impact on Food Store Availability in the United States. Prev Med. 2014;58:33–39. doi: 10.1016/j.ypmed.2013.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643–660. doi: 10.1093/nutrit/nuv027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grant T, Brigham EP, McCormack MC. Childhood Origins of Adult Lung Disease as Opportunities for Prevention. J Allergy Clin Immunol Pract. 2020;8(3):849–858. doi: 10.1016/j.jaip.2020.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Khalid F, Holguin F. A review of obesity and asthma across the life span. J Asthma. 2018;55(12):1286–1300. doi: 10.1080/02770903.2018.1424187 [DOI] [PubMed] [Google Scholar]
- 54.Holt EW, Theall KP, Rabito FA. Individual, Housing, and Neighborhood Correlates of Asthma among Young Urban Children. J Urban Health. 2013;90(1):116–129. doi: 10.1007/s11524-012-9709-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Northridge J, Ramirez OF, Stingone JA, Claudio L. The Role of Housing Type and Housing Quality in Urban Children with Asthma. J Urban Health. 2010;87(2):211–224. doi: 10.1007/s11524-009-9404-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jacobs DE. Environmental Health Disparities in Housing. Am J Public Health. 2011;101(Suppl 1):S115–S122. doi: 10.2105/AJPH.2010.300058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ahluwalia SK, Peng RD, Breysse PN, et al. Mouse allergen is the major allergen of public health relevance in Baltimore City. J Allergy Clin Immunol. 2013;132(4):830–835.e2. doi: 10.1016/j.jaci.2013.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rabito FA, Carlson J, Holt EW, Iqbal S, James MA. Cockroach exposure independent of sensitization status and association with hospitalizations for asthma in inner-city children. Annals of Allergy, Asthma & Immunology. 2011;106(2):103–109. doi: 10.1016/j.anai.2010.10.013 [DOI] [PubMed] [Google Scholar]
- 59.Rosenstreich DL, Slavin RG, Lynn H. The Role of Cockroach Allergy and Exposure to Cockroach Allergen in Causing Morbidity among Inner-City Children with Asthma. The New England Journal of Medicine. Published online 1997:8. [DOI] [PubMed] [Google Scholar]
- 60.Gruchalla RS, Pongracic J, Plaut M, et al. Inner City Asthma Study: Relationships among sensitivity, allergen exposure, and asthma morbidity. Journal of Allergy and Clinical Immunology. 2005;115(3):478–485. doi: 10.1016/j.jaci.2004.12.006 [DOI] [PubMed] [Google Scholar]
- 61.Rauh VA, Chew GR, Garfinkel RS. Deteriorated housing contributes to high cockroach allergen levels in inner-city households. Environ Health Perspect. 2002;110(Suppl 2):323–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Peters JL, Levy JI, Rogers CA, Burge HA, Spengler JD. Determinants of Allergen Concentrations in Apartments of Asthmatic Children Living in Public Housing. J Urban Health. 2007;84(2):185–197. doi: 10.1007/s11524-006-9146-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chew GL, Perzanowski MS, Miller RL, et al. Distribution and determinants of mouse allergen exposure in low-income New York City apartments. Environ Health Perspect. 2003;111(10):1348–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rhee H, Love T, Harrington D, Grape A. Common allergies in urban adolescents and their relationships with asthma control and healthcare utilization. Allergy Asthma Clin Immunol. 2018;14. doi: 10.1186/s13223-018-0260-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.O’Connor GT, Lynch SV, Bloomberg GR, et al. Early-life home environment and the risk of developing asthma among inner-city children. J Allergy Clin Immunol. 2018;141(4):1468–1475. doi: 10.1016/j.jaci.2017.06.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Langley SJ, Goldthorpe S, Craven M, Morris J, Woodcock A, Custovic A. Exposure and sensitization to indoor allergens: Association with lung function, bronchial reactivity, and exhaled nitric oxide measures in asthma. Journal of Allergy and Clinical Immunology. 2003;112(2):362–368. doi: 10.1067/mai.2003.1654 [DOI] [PubMed] [Google Scholar]
- 67.Matsui EC, Eggleston PA, Buckley TJ, et al. Household mouse allergen exposure and asthma morbidity in inner-city preschool children. Annals of Allergy, Asthma & Immunology. 2006;97(4):514–520. doi: 10.1016/S1081-1206(10)60943-X [DOI] [PubMed] [Google Scholar]
- 68.Grant T, Phipatanakul W, Perzanowski M, et al. Reduction in mouse allergen exposure is associated with greater lung function growth. Journal of Allergy and Clinical Immunology. 2020;145(2):646–653.e1. doi: 10.1016/j.jaci.2019.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grol MH, Gerritsen J, Vonk JM, et al. Risk Factors for Growth and Decline of Lung Function in Asthmatic Individuals up to Age 42 years. Am J Respir Crit Care Med. 1999;160(6):1830–1837. doi: 10.1164/ajrccm.160.6.9812100 [DOI] [PubMed] [Google Scholar]
- 70.Limb SL, Brown KC, Wood RA, et al. Irreversible lung function deficits in young adults with a history of childhood asthma. J Allergy Clin Immunol. 2005;116(6):1213–1219. doi: 10.1016/j.jaci.2005.09.024 [DOI] [PubMed] [Google Scholar]
- 71.McGeachie MJ, Yates KP, Zhou X, et al. Patterns of Growth and Decline in Lung Function in Persistent Childhood Asthma. N Engl J Med. 2016;374(19):1842–1852. doi: 10.1056/NEJMoa1513737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sin DD, Wu L, Man SFP. The relationship between reduced lung function and cardiovascular mortality: a population-based study and a systematic review of the literature. Chest. 2005;127(6):1952–1959. doi: 10.1378/chest.127.6.1952 [DOI] [PubMed] [Google Scholar]
- 73.Hood E Dwelling Disparities: How Poor Housing Leads to Poor Health. Environ Health Perspect. 2005;113(5):A310–A317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shorter C, Crane J, Pierse N, et al. Indoor visible mold and mold odor are associated with new-onset childhood wheeze in a dose-dependent manner. Indoor Air. 2018;28(1):6–15. doi: 10.1111/ina.12413 [DOI] [PubMed] [Google Scholar]
- 75.Karvonen AM, Hyvärinen A, Korppi M, et al. Moisture Damage and Asthma: A Birth Cohort Study. Pediatrics. 2015;135(3):e598–e606. doi: 10.1542/peds.2014-1239 [DOI] [PubMed] [Google Scholar]
- 76.Mendell MJ, Mirer AG, Cheung K, Tong M, Douwes J. Respiratory and Allergic Health Effects of Dampness, Mold, and Dampness-Related Agents: A Review of the Epidemiologic Evidence. Environ Health Perspect. 2011;119(6):748–756. doi: 10.1289/ehp.1002410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ahluwalia SK, Matsui EC. Indoor Environmental Interventions for Furry Pet Allergens, Pest Allergens, and Mold: Looking to the Future. J Allergy Clin Immunol Pract. 2018;6(1):9–19. doi: 10.1016/j.jaip.2017.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Matsui EC. Environmental exposures and asthma morbidity in children living in urban neighborhoods. Allergy. 2014;69(5):553–558. doi: 10.1111/all.12361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Disparities in the Impact of Air Pollution. Accessed June 19, 2021. /clean-air/outdoors/who-is-at-risk/disparities
- 80.Kioumourtzoglou M-A, Schwartz J, James P, Dominici F, Zanobetti A. PM2.5 and mortality in 207 US cities: Modification by temperature and city characteristics. Epidemiology. 2016;27(2):221–227. doi: 10.1097/EDE.0000000000000422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tessum CW, Paolella DA, Chambliss SE, Apte JS, Hill JD, Marshall JD. PM2.5 polluters disproportionately and systemically affect people of color in the United States. Science Advances. 2021;7(18):eabf4491. doi: 10.1126/sciadv.abf4491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.O’Neill MS, Jerrett M, Kawachi I, et al. Health, wealth, and air pollution: advancing theory and methods. Environ Health Perspect. 2003;111(16):1861–1870. doi: 10.1289/ehp.6334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nardone A, Casey JA, Morello-Frosch R, Mujahid M, Balmes JR, Thakur N. Associations between historical residential redlining and current age-adjusted rates of emergency department visits due to asthma across eight cities in California: an ecological study. The Lancet Planetary Health. 2020;4(1):e24–e31. doi: 10.1016/S2542-5196(19)30241-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Berchick ER, Barnett JC, Upton RD. Health Insurance Coverage in the United States: 2018. :44. [Google Scholar]
- 85.Gaskin DJ, Dinwiddie GY, Chan KS, McCleary RR. Residential Segregation and the Availability of Primary Care Physicians. Health Serv Res. 2012;47(6):2353–2376. doi: 10.1111/j.1475-6773.2012.01417.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Stewart KA, Higgins PC, McLaughlin CG, Williams TV, Granger E, Croghan TW. Differences in prevalence, treatment, and outcomes of asthma among a diverse population of children with equal access to care: findings from a study in the military health system. Arch Pediatr Adolesc Med. 2010;164(8):720–726. doi: 10.1001/archpediatrics.2010.100 [DOI] [PubMed] [Google Scholar]
- 87.Akenroye AT, Heyward J, Keet C, Alexander GC. Lower Use of Biologics for the Treatment of Asthma in Publicly Insured Individuals. J Allergy Clin Immunol Pract. Published online February 6, 2021:S2213–2198(21)00169–0. doi: 10.1016/j.jaip.2021.01.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rand CS, Butz AM, Kolodner K, Huss K, Eggleston P, Malveaux F. Emergency department visits by urban African American children with asthma. Journal of Allergy and Clinical Immunology. 2000;105(1):83–90. doi: 10.1016/S0091-6749(00)90182-9 [DOI] [PubMed] [Google Scholar]
- 89.Cremer NM, Baptist AP. Race and Asthma Outcomes in Older Adults: Results from the National Asthma Survey. The Journal of Allergy and Clinical Immunology: In Practice. 2020;8(4):1294–1301.e7. doi: 10.1016/j.jaip.2019.12.014 [DOI] [PubMed] [Google Scholar]
- 90.Stress and Health Disparities: Contexts, Mechanisms, and Interventions Among Racial/Ethnic Minority and Low Socioeconomic Status Populations: (500202018-001). Published online 2017. doi: 10.1037/e500202018-001 [DOI]
- 91.Landeo-Gutierrez J, Celedón JC. Chronic stress and asthma in adolescents. Annals of Allergy, Asthma & Immunology. 2020;125(4):393–398. doi: 10.1016/j.anai.2020.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wright RJ, Visness CM, Calatroni A, et al. Prenatal Maternal Stress and Cord Blood Innate and Adaptive Cytokine Responses in an Inner-City Cohort. Am J Respir Crit Care Med. 2010;182(1):25–33. doi: 10.1164/rccm.200904-0637OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rosa M, Lee A, Wright R. Evidence establishing a link between prenatal and early-life stress and asthma development. Current Opinion in Allergy and Clinical Immunology. 2018;18:1. doi: 10.1097/ACI.0000000000000421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Oland AA, Booster GD, Bender BG. Psychological and lifestyle risk factors for asthma exacerbations and morbidity in children. World Allergy Organ J. 2017;10(1). doi: 10.1186/s40413-017-0169-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Calhoun WJ, Haselkorn T, Miller DP, Omachi TA. Asthma exacerbations and lung function in patients with severe or difficult-to-treat asthma. Journal of Allergy and Clinical Immunology. 2015;136(4):1125–1127.e4. doi: 10.1016/j.jaci.2015.05.014 [DOI] [PubMed] [Google Scholar]
- 96.Bai TR, Vonk JM, Postma DS, Boezen HM. Severe exacerbations predict excess lung function decline in asthma. European Respiratory Journal. 2007;30(3):452–456. doi: 10.1183/09031936.00165106 [DOI] [PubMed] [Google Scholar]
- 97.Gauderman WJ, Urman R, Avol E, et al. Association of Improved Air Quality with Lung Development in Children. New England Journal of Medicine. 2015;372(10):905–913. [DOI] [PMC free article] [PubMed] [Google Scholar]


