Figure 4.
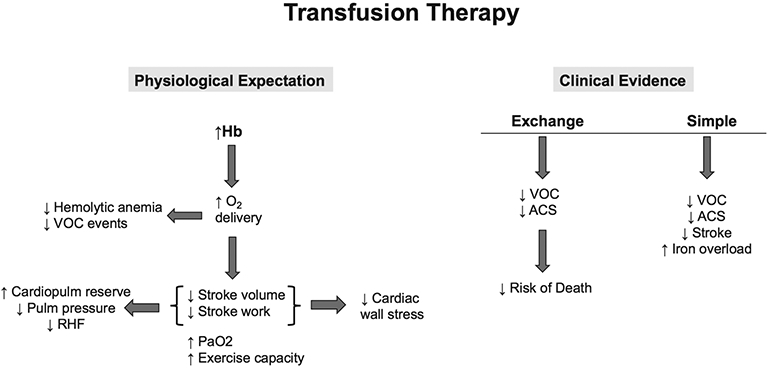
Transfusion therapy for cardiopulmonary disease in adults with SCD. The physiological expectation for transfusion therapy in SCD is that increasing Hb levels will improve oxygen (O2) delivery to tissues, lowering intravascular haemolytic and VOC events. Where the heart is concerned, stroke volume and stroke work are reduced, which decreases cardiac wall stress, increases cardiopulmonary (cardiopulm) reserve, lowers pulmonary (pulm) pressures and reduces risk for RHF. Arterial oxygen tension (PaO2) also increases along with improvement in exercise capacity. The clinical evidence for efficacy of transfusion therapy, however, is limited to observations of decreased VOC and ACS events and subsequently lowered risk of death with exchange transfusion therapy. Simple transfusion therapy, when used prophylactically, appears to decrease VOC, ACS and stroke but may also contribute to iron overload. ACS, acute chest syndrome; Hb, haemoglobin; RHF, right heart failure; VOC, vaso-occlusive; SCD, sickle cell disease.
