Abstract
Early diagnosis of AKI and preventive measures can likely decrease the severity of the injury and improve patient outcomes. Current hemodynamic monitoring variables, including BP, heart and respiratory rates, temperature, and oxygenation status, have been used to identify patients at high risk for AKI. Despite the widespread use of such variables, their ability to accurately and timely detect patients who are high risk has been questioned. Therefore, there is a critical need to develop and validate tools that can measure new and more kidney-specific hemodynamic and laboratory variables, potentially assisting with AKI risk stratification, implementing appropriate and timely preventive measures, and hopefully improved outcomes. The new ultrasonography techniques provide novel insights into kidney hemodynamics and potential management and/or therapeutic targets. Contrast-enhanced ultrasonography; Doppler flow patterns of hepatic veins, portal vein, and intrakidney veins; and ultrasound elastography are among approaches that may provide such information, particularly related to vascular changes in AKI, venous volume excess or congestion, and fluid tolerance. This review summarizes the current state of these techniques and their relevance to kidney hemodynamic management.
Keywords: acute kidney injury and ICU nephrology, acute kidney injury, AKI, hemodynamics, intravenous fluids, IVF, kidney congestion, POCU, ultrasound, volume overload, volume tolerance
Introduction
Managing hypotension in patients who are critically ill has traditionally focused on sustaining cardiac output via intravenous fluids or vasopressors (1). Administering intravenous fluids to patients with distributive or hypovolemic shock is a widely adopted treatment strategy (2). Rapid administration of crystalloids for patients who are hypotensive is a cornerstone of the Surviving Sepsis Campaign 1-hour bundle (3). The Surviving Sepsis Campaign also suggests using volume responsiveness (VR) as a guide to administering fluids. VR is defined as a stroke volume increase of >10% in response to intravenous fluid challenges (4). However, there is a growing concern that these guidelines which recommend fluid administration are not supported by substantial evidence (5). Using VR may lead to over-resuscitation, resulting in iatrogenic volume overload. Although fluid therapy is lifesaving for appropriate indications, it could also be associated with significant adverse effects (6–8). The kidney is one of the organs frequently affected by volume overload. Indeed, kidney congestion is considered one of the primary etiologies of decreased GFRs (9,10).
From a physiologic perspective, fluid administration leads to an increase in right and left atrial pressures. Perfusion depends on the pressure gradient between the artery and vein supplying an organ, as do filtration and plasma resorption across the capillary bed. Increased venous pressure reduces the pressure gradient and, thus, decreases blood supply. At the same time, it causes increased interstitial fluid. Edema occurs when there is a mismatch between plasma filtration at the capillary arteriolar side and resorption at the venule side. When this mismatch exceeds lymphatic drainage, edema occurs (Figure 1). Further elevations in venous pressure from ongoing volume loading cause more edema formation, which increases interstitial pressure. Eventually, interstitial pressure exceeds arteriolar inflow. This effect is more prominent in encapsulated organs, such as the kidneys (11), where increased venous pressure increases interstitial pressure, leading to organ dysfunction and AKI (11,12).
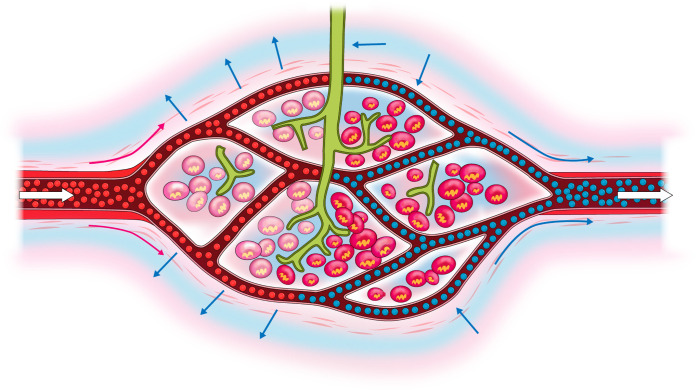
Figure 1.
Fluid movement balance across capillary wall and edema formation from increased venous pressure. White arrows indicate blood movement direction, short blue arrows indicate fluid movement across the capillary wall, and long red and blue arrows indicate direction of movement of oxygenated (red arrows) and deoxygenated (blue arrows) blood. Green vessels represent lymphatics.
Patients in shock are particularly susceptible to kidney edema formation. Low oncotic pressure from disease and crystalloid boluses contribute to the filtration/resorption mismatch. Systemic vasopressors increase arterial and venous vascular tone, leading to increased filtration (higher mean arteriolar pressure) and decreased resorption (higher mean venule pressure), increasing the risk of organ edema.
When the shock is associated with respiratory failure, positive pressure ventilation results in right-sided venous congestion. Flow into the right atrium from the inferior vena cava (IVC) and superior vena cava depends on the pressure gradient between the mean circulatory filling pressure (MCFP) and right atrial pressure (RAP). The MCFP is the pressure in the extrathoracic IVC and superior vena cava and reflects the venous pressure at the end organ. The RAP is lower than the MCFP to allow blood flow into the thorax. Positive pressure ventilation increases thoracic pressure and, thus, RAP and central venous pressure (CVP) increase without an increase in MCFP. This effect would lead to a decline in the pressure gradient, causing decreased venous return. When initially placed on positive pressure ventilation, many patients become acutely hypotensive and require fluid boluses to increase the MCFP. Among patients on mechanical ventilation who need increased mean airway pressure to manage progressive respiratory failure, fluid boluses may be needed to protect the MCFP and facilitate venous return. In turn, the increased MCFP could increase the kidney venous pressure and may further worsen kidney congestion.
The sequelae of elevated left atrial pressure are relatively easy to assess clinically. It often leads to pulmonary edema, which results in hypoxia and is frequently detected on plain x-rays or oxygenation indicators like partial pressure of oxygen/fraction of inspired oxygen (PaO2/FIO2). In contrast, identifying an increase in RAP is more challenging (12). CVP monitors and pulmonary artery catheters assess RAP. Still, they are invasive, confounded by positive pressure ventilation, and have not improved outcomes despite years of study (13,14). Point-of-care ultrasonography (POCUS) is helpful in this area, because increasing pressure in the right atrium from venous excess or congestion leads to distinct changes in Doppler venous return flow patterns. Doppler flow patterns of hepatic veins (HVs), portal veins (PVs), and intrakidney veins (iKVs) are noninvasive and can identify early stages of right-sided venous congestion (15). Indeed, abnormal waveforms are associated with AKI in patients after cardiac surgery (16,17) and may help predict early AKI in the general intensive-care-unit population (12).
In addition to Doppler flow patterns, other ultrasonography techniques are suggested to delineate the kidney hemodynamics, including contrast-enhanced ultrasonography (CEUS) (18) and ultrasound elastography (USE) (19).
In this review article, we present POCUS techniques to assess kidney hemodynamics and describe their clinical implications.
Ultrasound Terminology
The ultrasound examination is usually performed in three consecutive phases (20). The first step is a grayscale two-dimensional image of the organ of interest. This mode is called the brightness mode or B-mode. B-modes are followed by the color Doppler to produce a colored representation of blood flow dynamics. Finally, a small portion of the vessel is selected, and a spectral Doppler waveform is obtained for a more focused assessment of the blood flow rates. Doppler is an eponym named after the Austrian physicist who first described the “Doppler effect” in the 19th century (21). Pulsed wave Doppler, the main form of Doppler ultrasound described in this article, is based on sending pulsed signals, allowing sampling at a specific location by the cursor.
IVC
The IVC is a compliant, tear-shaped vessel. IVC size and shape fluctuate with variations in CVP and intravascular volume (22,23). Several factors may affect the IVC size. Under normal physiologic conditions, IVC diameter decreases and venous return increases during inspiration due to negative intrathoracic pressure and positive intra-abdominal pressure. This relationship is reversed in positive pressure mechanical ventilation (24). IVC diameter also decreases during ventricular systole in patients who are spontaneously breathing. Moreover, the patients’ position alters the IVC diameter. However, measuring IVC in the supine position is now recommended in the American Society of Echocardiography Guidelines (25).
The IVC diameter assessment is usually considered a noninvasive tool to measure CVP (22). Measuring CVP was described several decades ago (20) and has since become a standard method to assess volume status and guidance for intravenous fluid therapy. However, many subsequent studies indicate a poor association between CVP and blood volume and the inability of CVP and/or its changes to predict the hemodynamic response to a fluid challenge (2,26). Hence, relying on CVP for fluid management should not be the only deciding factor. However, IVC diameter and IVC variability may be helpful as a marker of the right ventricular (RV) function in some clinical circumstances, such as acute RV failure (26).
The IVC is best examined using a subcostal view with a longitudinal section (24). The diameter is best measured in M-mode (or motion mode) coupled to the two-dimensional image, just upstream of the HV entry or approximately 1–2 cm caudal to the cavoatrial junction. Measurements are most accurate when the M-mode tracing is perpendicular to the IVC (27).
The IVC diameter variation through the respiratory cycle can be quantified by measuring the IVC collapsibility index (IVCCI). The operator measures the maximum (IVCmax) and minimum IVC diameters (IVCmin) during the respiratory cycle. IVCCI is then calculated as (IVCmax−IVCmin)/IVCmax. In a patient who is spontaneously breathing, an IVC diameter of <2 cm correlates with CVP of <10 cmH2O (28). An IVC diameter of >2 cm and IVCCI of <50% indicates a CVP of >10 cmH2O (29). It is important to note that IVCCI has not been validated in patients with respiratory failure requiring positive pressure mechanical ventilation.
Of note, there is controversy around the utility of IVC measurements in patients who are mechanically ventilated (30), especially those who have undergone abdominal surgery or severe respiratory failure requiring high mean airway pressure ventilation. In this situation, the IVC diameter and collapsibility changes may reflect the positive pressure ventilation rather than CVP. Therefore, many intensivists no longer use this method of assessment as a measure of volume status. It is also worth noting that studies investigating the utility of IVC measurements use a wide variety of measurements and different percentages as the threshold for collapsibility. In addition, each study has used a different comparator to assess the validity of IVC measurements in determining fluid responsiveness.
Although IVC measurements can estimate CVP and its variability, they are not strong predictors of fluid responsiveness. A meta-analysis examined 19 studies looking at the relationship between CVP and its variability and a change in cardiac performance after a fluid challenge. The pooled correlation coefficient between baseline CVP and change in the cardiac index was 0.18. The pooled area under the receiver operating characteristic curve was 0.56. The pooled correlation between CVP variability and change in the cardiac index was 0.11 (26).
Stroke volume variation (SVV) is a better predictor of fluid responsiveness when compared with IVC variation in patients who are critically ill. A meta-analysis of clinical trials investigated the diagnostic value of SVV in predicting fluid responsiveness. A total of 568 patients from 23 studies were included. Baseline SVV was correlated to fluid responsiveness with a pooled correlation coefficient of 0.718 and pooled area under the receiver operating characteristic curve of 0.84 (31). Although POCUS can quantify SVV, the discussion of this technique is beyond the scope of the article.
Liver Doppler Waveforms
The hepatic arteries, HVs, and PVs are the principal vascular bundles of the liver. The changes in blood flow patterns in HVs and PVs are important in volume overload and tolerance assessment. Each one of these vessels has a distinctive “signature” waveform appearance.
HV
The HV can be examined using a phased array probe. The middle HV is identified from a midsubcostal (Figure 2) or lateral view. Hepatic venous waveforms are obtained via applying pulsed wave Doppler at about 2–4 cm from its junction to the IVC.
Figure 2.
Ultrasound probe placement location to acquire hepatic and portal vein images. IVC, inferior vena cava.
The hepatic venous waveform reflects the pressure changes in the right atrium during the cardiac cycle. Unlike hepatic venous flow that correlates with the RAP changes and is pulsatile, the portal flow is continuous and reflects visceral venous pressure. The HV Doppler evaluates how blood flows into the right atrium, so—theoretically—it is not confounded by positive pressure ventilation.
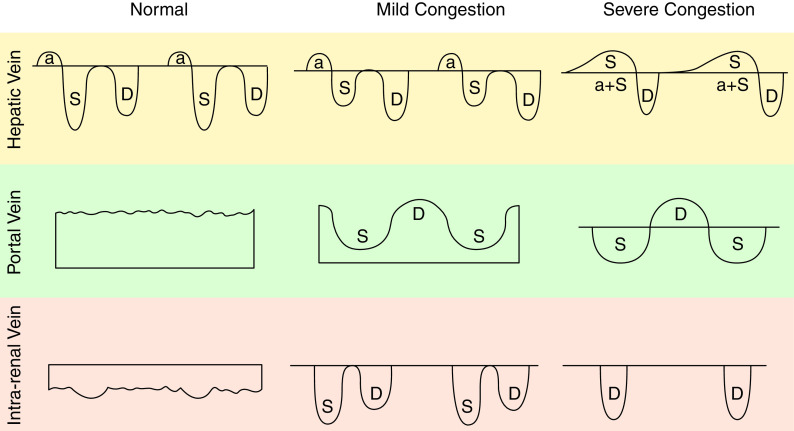
Typically, the HV waveform has one primary retrograde wave, i.e., flow directed toward the transducer and appears above the baseline, along with two major antegrade waves, i.e., flow directed away from the transducer and appears below the baseline. The retrograde wave (“a”) peaks corresponding with atrial contraction at the end of the diastole. The antegrade systolic (S) wave corresponds with peak negative pressure generated by the tricuspid valve annulus downward motion in early systole. The antegrade diastolic (D) wave relates to RV filling in early diastole. In between the S and D waves, there is sometimes a v wave with a peak that marks the transition between systole and diastole, and it corresponds with the tricuspid valve opening. The v wave is rarely seen in HV Doppler.
The HV S and D waveforms remain antegrade when the RAP is not elevated, indicating the HV blood flow toward the right atrium during the cardiac cycle. The S wave is normally larger than the D wave because the antegrade flow is more prominent during systole.
In mild venous congestion, the S wave becomes smaller than the D wave due to increased RAP. In severe venous congestion, the S wave turns to retrograde (flow directed toward the transducer) or fuses with the “a” wave to become a sizable retrograde wave (above the baseline). These changes are illustrated in (Figure 3).
Figure 3.
Normal and abnormal venous waveforms in hepatic, portal and intrarenal veins. a, atrial contraction; S, systolic flow; D, diastolic flow.
Abnormal hepatic waveforms were shown to predict adverse kidney outcomes in a prospective study in adult patients admitted to the ICU. S to D reversal in HV flow had an odds ratio of 4.0 (95% CI, 1.4 to 11.2) for an increase in the likelihood of a significant kidney event (12).
PV
PV images are obtained in the supine position using a phased array transducer placed in midcosta (Figure 2) or a right posterior-axillary coronal view between the ninth and eleventh intercostal space (32). PV walls are echogenic (white) that differentiate them from the HVs. The PV flow is mono- or biphasic. Because the PV blood flow velocity is low (i.e., 10–30 cm/s), the velocity gate should be adjusted to a lower range (i.e., 20–40 cm/s) to acquire appropriate images. Typically, the monophasic to biphasic PV waveforms are completely retrograde (flow directed toward the transducer) and have small variations throughout the cardiac cycle. Respiratory variation is often observed.
The waveforms are consistently biphasic with increased “pulsatility” due to a systolic flow reduction in mild congestion. In severe liver congestion, the flow completely disappears during systole. In more severe cases, the flow can even reverse to antegrade (flow directed away from the transducer), giving the waveform a “to-and-fro” pattern (Figure 3).
Measuring the PV pulsatility index ([maximum flow velocity−minimum flow velocity]/maximum flow velocity) quantifies the flow variation through the cardiac cycle, hence, liver congestion. An index of >30% is highly suggestive of liver congestion and is associated with a higher incidence of adverse kidney outcomes (odds ratio, 2.2; 95% CI, 1.3 to 3.6) (33). When measured pre- or postoperatively, PV pulsatility is associated with a higher AKI incidence after cardiac surgery (16,17). PV pulsatility is also a measure of portal hypertension and can be found in patients with end stage liver disease. In these patients, it may not represent elevated RAP.
Kidney Doppler Waveforms
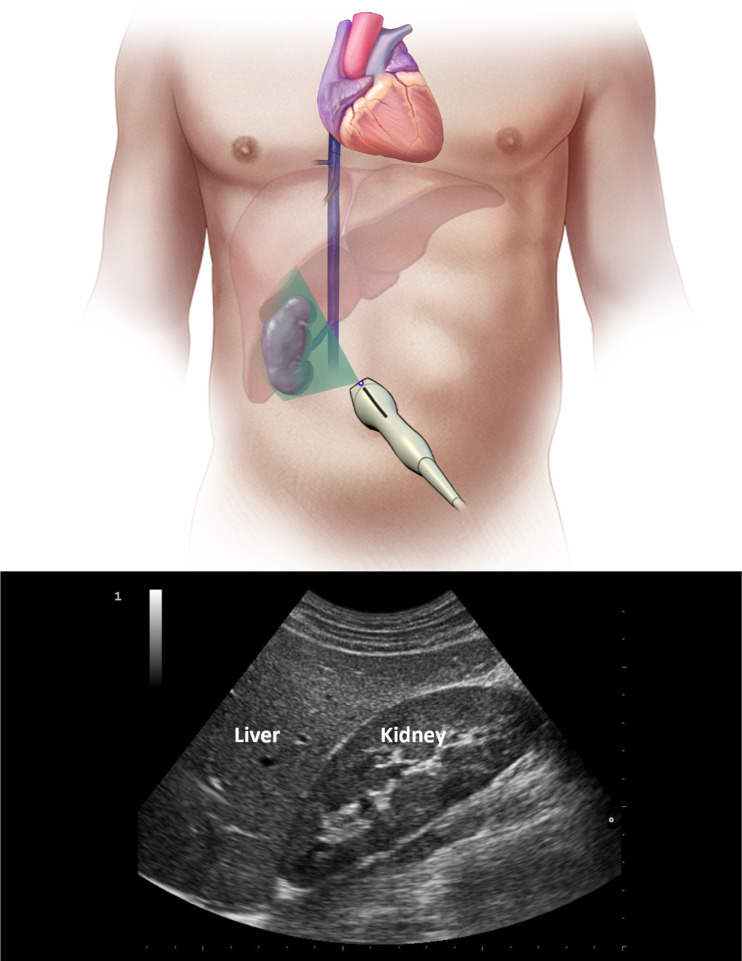
Intrakidney Doppler ultrasonography images can be obtained in supine (Figure 4) or lateral decubitus positions. The color Doppler velocity range should be set to approximately 16 cm/s (15). The color Doppler images can locate the interlobar vessels. Because the interlobar arteries and veins run in proximity to one another, pulse wave Doppler of the interlobar arteries and veins can be recorded simultaneously. This approach can more easily detect the venous waveform systolic and diastolic phases, even if electrocardiogram leads are not available. Normally, the iKV waveform is continuous and antegrade (flow directed away from the transducer). This reflects blood flow from the iKV toward the IVC in both systole and diastole.
Figure 4.
Ultrasound probe placement location to obtain kidney Doppler waveforms.
In mild venous congestion, the flow pattern is biphasic with visible S and D waveforms (Figure 3). As venous congestion increases, the S waveform size decreases. In severe venous congestion, the S waveform completely disappears, giving the waveform a monophasic pattern. In a study by Iida et al. (15), death and unplanned admission for heart failure were progressively higher when the waveform patterns changed from continuous to biphasic and monophasic patterns.
One method to quantify the discrepancy between systolic and diastolic iKV flow is calculating the kidney venous impedance index as (maximum flow velocity−minimum flow velocity)/maximum flow velocity. Venous impedance index has been shown to correlate with the expansion and removal of intravascular fluids among patients with heart failure with preserved (0.2 pre–volume expansion to 0.7 post–volume expansion) or reduced (0.4 pre–volume expansion to 0.7 post–volume expansion) ejection fraction (34).
The Venous Excess Ultrasound Score
The venous excess ultrasound score (VExUS) grading system was developed to combine a qualitative assessment of venous Doppler examination of the HV, PV, iKV, and IVC diameter into grading the severity of venous congestion (35). The Doppler flow patterns are rated as normal, mildly abnormal, or severely abnormal (Figure 5). The IVC diameter is converted to a binary variable with 2 cm as the cutoff. This information was combined into a grading scheme.
Figure 5.

Doppler flow patterns for assessment of venous excess ultrasound score (VExUS). RAP, right atrial pressure.
In patients post–cardiac surgery, VExUS was used to predict AKI (35). The authors evaluated several grading schemes, and the VExUS C scheme, grade 3, which is defined by the presence of severe flow abnormalities in at least two vascular beds along with dilated IVC of >2 cm, was most strongly associated with subsequent AKI (hazard ratio, 3.69; 95% CI, 1.5 to 8.24; P=0.001). The association remained significant after adjusting for baseline risk factors of AKI and the need for vasopressor/inotropic support (hazard ratio, 2.82; 95% CI, 1.21 to 6.55; P=0.02). It is worth noting that although IVC dilation alone had poor predictive performance for AKI, its inclusion within the VExUS grading system resulted in a slight increase in the VExUS specificity (35). Also, one should keep in mind that patients undergoing cardiac surgery are a specific subset of patients with critical illness. Thus, some of these metrics may be different in a general ICU population. Table 1 describes two cases in which ultrasonography examination of hemodynamics delineated clinical findings that led to improved care.
Table 1.
Case prototypes
| Case | POCUS Findings |
| A 75-year-old female is hospitalized after undergoing elective cholecystectomy. Her surgery was complicated by bowel perforation. She is now in atrial fibrillation with RVR with borderline BP. She has a net fluid balance of 6 L since admission and bilateral pleural effusions on her chest x-ray. She requires 4 L of oxygen via nasal cannula. Her kidney function is normal. The team wants to assess for intravascular volume overload and the need for diuresis. Her hepatic, portal, and intrakidney vein Doppler patterns are shown in Figure 7. She has an IVC diameter of 2.1 cm with minimal variation during the respiratory cycle. | In this case, the patient had clinical evidence of volume overload. However, her borderline BP posed concerns about whether she was intravascularly depleted. The hepatic waveform pattern shows an inversion of the S wave, indicating severe congestion. It is worth noting that the “a” waves are usually absent when the patient is in atrial fibrillation. The portal waveform pattern shows mild pulsatility with the cardiac cycle, and the intrakidney waveform patterns look normal. On the basis of these findings and the IVC diameter, the patient was deemed to have venous congestion and was treated with diuresis. She remained hemodynamically stable with the diuresis (Figure 7). |
| A 54-year-old female is hospitalized in the ICU after a gastrectomy. She has a complicated postoperative course, including prolonged mechanical ventilation, hypotension, and kidney failure. She has a net fluid balance of 12 L since admission. She remains hypotensive on vasopressors. She was deemed “volume-responsive”—the team questions additional administration of IVF. | Despite volume responsiveness, the patient has clear evidence of volume congestion. The hepatic Doppler waveform looks slightly abnormal, with the S wave being smaller than the D wave. However, the portal waveform is abnormal with significant pulsatility, and the intrakidney waveform is abnormal, showing discontinuous S and D waves. In this case, we suggested titrating up vasopressors and maintaining volume status if end-organ hypoperfusion is the concern. However, if pulmonary edema is the concern, then we suggested careful removal of volume (Figures 8). |
POCUS, point-of-care ultrasonography; RVR, rapid ventricular rate; IVC, inferior vena cava; ICU, intensive care unit; IVF, intravenous fluids; S, systolic flow; D, diastolic flow.
Assessment of Left and Right Ventricle Function
A complete description of echocardiographic techniques is beyond the scope of this article. However, a focused echocardiographic examination is frequently performed in patients who are critically ill to determine “overall global function of the heart” and rule out acute conditions that can cause hypotension, such as large pericardial effusions or pneumothorax (36,37). The examination could be used to clarify the extent of left and right ventricle contraction or the presence of decompensated heart failure, pulmonary hypertension, or pulmonary embolism. The basic views for echocardiography are as follows: (1) The parasternal long-axis view is obtained by placing the probe between the third and fourth ribs left of the sternum (Figure 6A). The indicator points to the patient’s right shoulder. An ideal image includes the left atrium, mitral valve, left ventricle, aortic valve, aortic root, and right ventricle. The apex of the left ventricle will often be outside of the image. (2) The parasternal short-axis view is acquired after obtaining the parasternal long-axis view after the probe is rotated 90° clockwise to point to the patient’s left shoulder. The image captured will usually be at the level of the midventricle or papillary muscles. The levels captured as the operator tilts the transducer toward the apex and then toward the base include the aortic valve level, mitral valve level, papillary muscle level, and apical level (Figure 6B). (3) The apical four-chamber view is obtained by placing the probe at the point of maximum cardiac impulse, preferably with the patient in the left lateral decubitus position (Figure 6C). The indicator is pointed between the patient’s left shoulder and 3 o’clock. The probe is lifted upwards to allow a good view of the four chambers, and by lifting the probe more, the operator can open up the left ventricle outflow tract and aortic valve, obtaining an apical five-chamber view.
Figure 6.
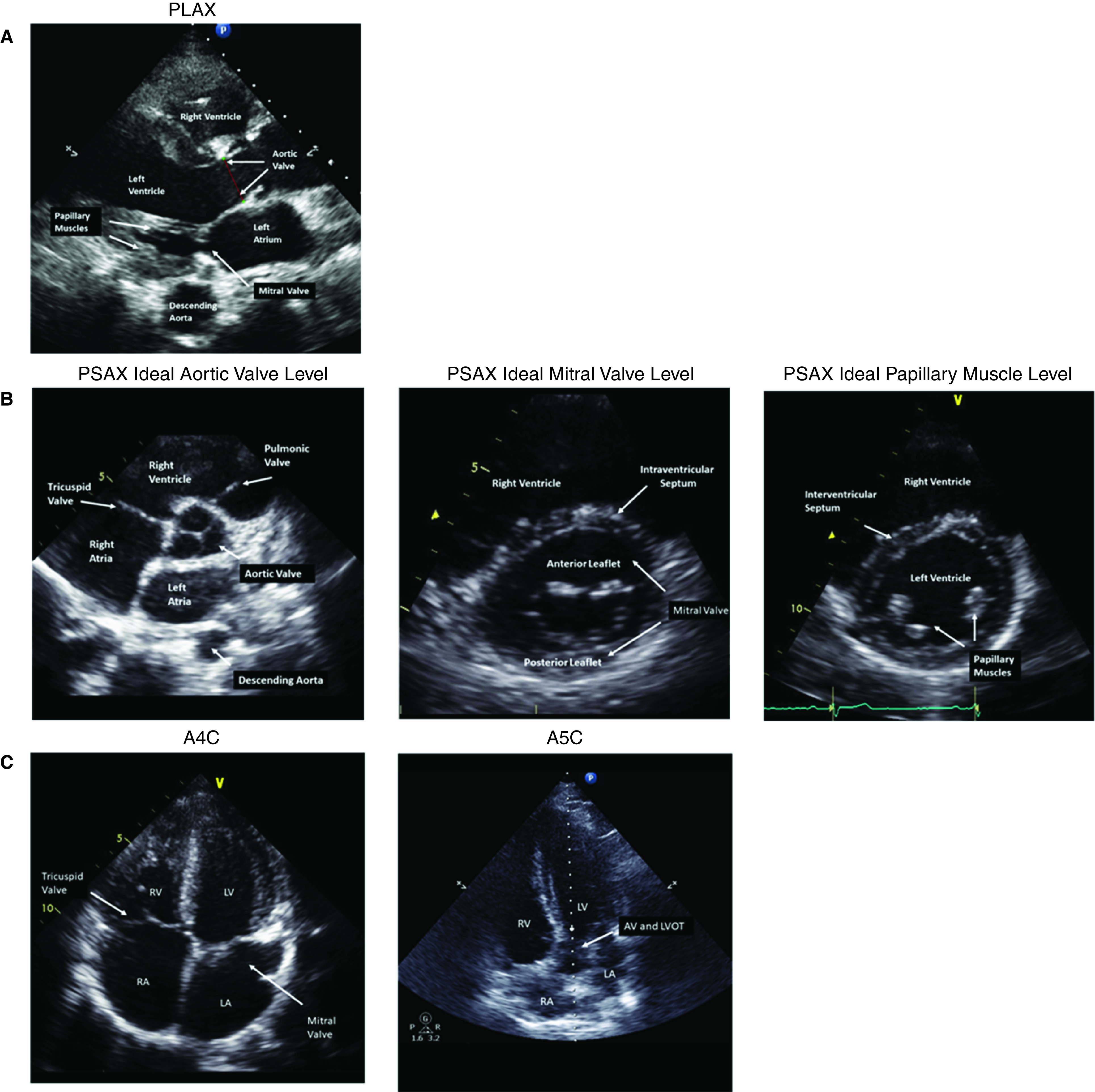
Echocardiographic windows used to acquire cardiac images. (A) parasternal long-axis (PLAX) view; (B) parasternal short-axis (PSAX) view; and (C) apical four-chamber (A4C) and apical five-chamber (A5C) views. AV, aortic valve; LA, left atrium; LV, left ventricle; LVOT, left ventricular outflow tract; RA, right atrium; RV, right ventricle.
Figure 7.
Ultrasonography examination for Case 1. (A) Hepatic vein, (B) portal vein, and (C) intrakidney Doppler waveforms.
Figure 8.
Ultrasonography examination for Case 2. (A) Hepatic vein, (B) portal vein, and (C) intrakidney Doppler waveforms.
CEUS and USE
New ultrasonography technologies may open additional venues that kidney hemodynamics could be assessed independently and with higher accuracy. CEUS and USE are among these emerging technologies. Although the clinical utilization of these new technologies remains to be investigated, being familiar with this field’s progress would potentially provide perspectives in research or clinical applications of ultrasonography.
Ultrasound contrast agents are used to enhance the resolution of cardiac and vascular images. Agitated saline contains microbubbles, and its use for higher resolution of aortic images was introduced in 1968 (38). Because the agitated saline air microbubbles had a short t1/2, the next generation of microbubbles includes a layer of albumin or galactose palmitic acid as a shell. Further, heavy mol wt gas agents, e.g., sulfur hexafluoride, to fill the microbubbles and surfactant, as the shell, improved the agent stability (39). CEUS use for kidney hemodynamic assessment has been reported in the literature. For instance, Schneider et al. (18,40) described kidney microvascular cortical perfusion changes in response to NE infusion, angiotensin II, and captopril using CEUS. Recent advances made in image resolution and ultrasound penetration depth have led to the development of high-resolution images of the kidney microvessels (e.g., super-resolution ultrasound microvessel imaging) (33,41–43). Although these technologies remain in preclinical investigation phases, they provide a vast potential for kidney hemodynamic assessment.
The other new technology in development with potential in enhanced ability in kidney hemodynamic assessment is USE. Because kidney elasticity changes with hemodynamic alterations, elastography can provide a unique perspective on kidney hemodynamic alterations (44). In a swine model, investigators showed that using USE correlates with intra-abdominal pressure and pressure inside the kidney capsule significantly more than bladder pressure (19). This imaging technique can potentially enhance our ability to manage fluid therapy, particularly in identifying kidney congestion.
Challenges and Benefits of Using POCUS
Factors that may limit POCUS usability include the patients’ body habitus, bowel gas, and mechanical ventilation, making it harder to obtain ultrasonographic windows. However, many of these challenges also exist for other diagnostic modalities. In addition, other diagnostic modalities raise challenges that do not exist for POCUS. For example, transporting patients who are obese and patients on mechanical ventilation to radiology for diagnostic imaging poses a safety issue, including infectious control issues, especially in pandemics.
POCUS for hemodynamic evaluation is clearly feasible, but interobserver variability is poorly studied. Its accuracy depends on the skill of the person obtaining the images. It is best used by a well-trained individual provider as a point-in-time assessment or to track changes over time. Left ventricular ejection fraction and right ventricle function can be assessed in >90% of patients who are critically ill by using a protocol that obtains all four cardiac windows (36,37). Further, Spegial et al. (12) on venous flow patterns showed that HV flow assessments could be completed in >90%, the portal in > 80%, and kidney in about 75% of patients in the ICU.
POCUS has been successfully applied within telemedicine. Tele-ultrasound has advanced in recent years, both in high-income settings and in resource-limited countries where demand for tests often outpaces the access to diagnostic modalities needed to identify disease. According to the World Health Organization, imaging is required for diagnosis in 20%–30% of clinical cases, and ultrasound and/or plain radiographs are sufficient for 80%–90% of those cases (45).
Conclusion
Because POCUS has become an integrated part of patient care in inpatient and outpatient settings, understanding potential ultrasonography techniques to provide additional information about kidney-related hemodynamics is essential. Assessing right-sided venous flow patterns using POCUS is feasible and informative, not only for evaluating venous congestion, but also for estimating organ congestion, particularly that of the liver and kidney. The advent of novel ultrasonography technologies, such as CEUS and USE, may open this window even further. We predict that ultrasound devices will continue to get smaller, more portable, and less expensive, while providing higher resolution images. This progress is in concert with other technologic advances that will make ultrasound more feasible and invaluable in many clinical scenarios.
Disclosures
K.B. Kashani reports having consultancy agreements with AM Pharma; serving as a scientific advisor for, or member of, GE, La Jolla Inc., and MediBeacon Inc.; and receiving research funding from La Jolla Inc. All remaining authors have nothing to disclose.
Funding
None.
Author Contributions
K.B. Kashani conceptualized the study and provided supervision; K.B. Kashani and S. Murthi reviewed and edited the manuscript; and S. Safadi wrote the original draft.
References
- 1.Seymour CW, Rosengart MR: Septic shock: Advances in diagnosis and treatment. JAMA 314: 708–717, 2015. 10.1001/jama.2015.7885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marik PE, Cavallazzi R: Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med 41: 1774–1781, 2013. 10.1097/CCM.0b013e31828a25fd [DOI] [PubMed] [Google Scholar]
- 3.Levy MM, Evans LE, Rhodes A: The Surviving Sepsis Campaign bundle: 2018 update. Intensive Care Med 44: 925–928, 2018. 10.1007/s00134-018-5085-0 [DOI] [PubMed] [Google Scholar]
- 4.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP: Surviving Sepsis Campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43: 304–377, 2017. 10.1007/s00134-017-4683-6 [DOI] [PubMed] [Google Scholar]
- 5.Hu B, Chen JCY, Dong Y, Frank RD, Passe M, Portner E, Peng Z, Kashani K: Effect of initial infusion rates of fluid resuscitation on outcomes in patients with septic shock: A historical cohort study. Crit Care 24: 137, 2020. 10.1186/s13054-020-2819-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malbrain MLNG, Van Regenmortel N, Saugel B, De Tavernier B, Van Gaal PJ, Joannes-Boyau O, Teboul JL, Rice TW, Mythen M, Monnet X: Principles of fluid management and stewardship in septic shock: It is time to consider the four D’s and the four phases of fluid therapy. Ann Intensive Care 8: 66, 2018. 10.1186/s13613-018-0402-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prowle JR, Chua HR, Bagshaw SM, Bellomo R: Clinical review: Volume of fluid resuscitation and the incidence of acute kidney injury - a systematic review. Crit Care 16: 230, 2012. 10.1186/cc11345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ostermann M, Liu K, Kashani K: Fluid management in acute kidney injury. Chest 156: 594–603, 2019. 10.1016/j.chest.2019.04.004 [DOI] [PubMed] [Google Scholar]
- 9.Chen KP, Cavender S, Lee J, Feng M, Mark RG, Celi LA, Mukamal KJ, Danziger J: Peripheral edema, central venous pressure, and risk of AKI in critical illness. Clin J Am Soc Nephrol 11: 602–608, 2016. 10.2215/CJN.08080715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dalfino L, Tullo L, Donadio I, Malcangi V, Brienza N: Intra-abdominal hypertension and acute renal failure in critically ill patients. Intensive Care Med 34: 707–713, 2008. 10.1007/s00134-007-0969-4 [DOI] [PubMed] [Google Scholar]
- 11.Cruces P, Salas C, Lillo P, Salomon T, Lillo F, Hurtado DE: The renal compartment: A hydraulic view. Intensive Care Med Exp 2: 26, 2014. 10.1186/s40635-014-0026-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spiegel R, Teeter W, Sullivan S, Tupchong K, Mohammed N, Sutherland M, Leibner E, Rola P, Galvagno SM Jr, Murthi SB: The use of venous Doppler to predict adverse kidney events in a general ICU cohort. Crit Care 24: 615, 2020. 10.1186/s13054-020-03330-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah MR, Hasselblad V, Stevenson LW, Binanay C, O’Connor CM, Sopko G, Califf RM: Impact of the pulmonary artery catheter in critically ill patients: Meta-analysis of randomized clinical trials. JAMA 294: 1664–1670, 2005. 10.1001/jama.294.13.1664 [DOI] [PubMed] [Google Scholar]
- 14.Barrot L, Asfar P, Mauny F, Winiszewski H, Montini F, Badie J, Quenot JP, Pili-Floury S, Bouhemad B, Louis G, Souweine B, Collange O, Pottecher J, Levy B, Puyraveau M, Vettoretti L, Constantin JM, Capellier G; LOCO2 Investigators and REVA Research Network: Liberal or conservative oxygen therapy for acute respiratory distress syndrome. N Engl J Med 382: 999–1008, 2020. 10.1056/NEJMoa1916431 [DOI] [PubMed] [Google Scholar]
- 15.Iida N, Seo Y, Sai S, Machino-Ohtsuka T, Yamamoto M, Ishizu T, Kawakami Y, Aonuma K: Clinical implications of intrarenal hemodynamic evaluation by doppler ultrasonography in heart failure. JACC Heart Fail 4: 674–682, 2016. 10.1016/j.jchf.2016.03.016 [DOI] [PubMed] [Google Scholar]
- 16.Beaubien-Souligny W, Eljaiek R, Fortier A, Lamarche Y, Liszkowski M, Bouchard J, Denault AY: The association between pulsatile portal flow and acute kidney injury after cardiac surgery: A retrospective cohort study. J Cardiothorac Vasc Anesth 32: 1780–1787, 2018. 10.1053/j.jvca.2017.11.030 [DOI] [PubMed] [Google Scholar]
- 17.Beaubien-Souligny W, Benkreira A, Robillard P, Bouabdallaoui N, Chassé M, Desjardins G, Lamarche Y, White M, Bouchard J, Denault A: Alterations in portal vein flow and intrarenal venous flow are associated with acute kidney injury after cardiac surgery: A prospective observational cohort study. J Am Heart Assoc 7: e009961, 2018. 10.1161/JAHA.118.009961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schneider AG, Goodwin MD, Schelleman A, Bailey M, Johnson L, Bellomo R: Contrast-enhanced ultrasonography to evaluate changes in renal cortical microcirculation induced by noradrenaline: A pilot study. Crit Care 18: 653, 2014. 10.1186/s13054-014-0653-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kashani KB, Mao SA, Safadi S, Amiot BP, Glorioso JM, Lieske JC, Nyberg SL, Zhang X: Association between kidney intracapsular pressure and ultrasound elastography. Crit Care 21: 251, 2017. 10.1186/s13054-017-1847-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hughes RE, Magovern GJ: The relationship between right atrial pressure and blood volume. AMA Arch Surg 79: 238–243, 1959. 10.1001/archsurg.1959.04320080074009 [DOI] [PubMed] [Google Scholar]
- 21.Katsi V, Felekos I, Kallikazaros I: Christian Andreas Doppler: A legendary man inspired by the dazzling light of the stars. Hippokratia 17: 113–114, 2013 [PMC free article] [PubMed] [Google Scholar]
- 22.Sekiguchi H, Seaburg LA, Suzuki J, Astorne WJ, Patel AS, Keller AS, Gajic O, Kashani KB: Central venous pressure and ultrasonographic measurement correlation and their associations with intradialytic adverse events in hospitalized patients: A prospective observational study. J Crit Care 44: 168–174, 2018. 10.1016/j.jcrc.2017.10.039 [DOI] [PubMed] [Google Scholar]
- 23.Ciozda W, Kedan I, Kehl DW, Zimmer R, Khandwalla R, Kimchi A: The efficacy of sonographic measurement of inferior vena cava diameter as an estimate of central venous pressure. Cardiovasc Ultrasound 14: 33, 2016. 10.1186/s12947-016-0076-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barbier C, Loubières Y, Schmit C, Hayon J, Ricôme JL, Jardin F, Vieillard-Baron A: Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med 30: 1740–1746, 2004. 10.1007/s00134-004-2259-8 [DOI] [PubMed] [Google Scholar]
- 25.Beigel R, Cercek B, Luo H, Siegel RJ: Noninvasive evaluation of right atrial pressure. J Am Soc Echocardiogr 26: 1033–1042, 2013. 10.1016/j.echo.2013.06.004 [DOI] [PubMed] [Google Scholar]
- 26.Marik PE, Baram M, Vahid B: Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest 134: 172–178, 2008. 10.1378/chest.07-2331 [DOI] [PubMed] [Google Scholar]
- 27.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU: Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28: 1–39.e14, 2015. 10.1016/j.echo.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 28.Prekker ME, Scott NL, Hart D, Sprenkle MD, Leatherman JW: Point-of-care ultrasound to estimate central venous pressure: A comparison of three techniques. Crit Care Med 41: 833–841, 2013. 10.1097/CCM.0b013e31827466b7 [DOI] [PubMed] [Google Scholar]
- 29.Taniguchi T, Ohtani T, Nakatani S, Hayashi K, Yamaguchi O, Komuro I, Sakata Y: Impact of body size on inferior vena cava parameters for estimating right atrial pressure: A need for standardization? J Am Soc Echocardiogr 28: 1420–1427, 2015. 10.1016/j.echo.2015.07.008 [DOI] [PubMed] [Google Scholar]
- 30.Via G, Tavazzi G, Price S: Ten situations where inferior vena cava ultrasound may fail to accurately predict fluid responsiveness: a physiologically based point of view. Intensive Care Med 42: 1164–1167, 2016. 10.1007/s00134-016-4357-9 [DOI] [PubMed] [Google Scholar]
- 31.Zhang Z, Lu B, Sheng X, Jin N: Accuracy of stroke volume variation in predicting fluid responsiveness: a systematic review and meta-analysis. J Anesth 25: 904–916, 2011. 10.1007/s00540-011-1217-1 [DOI] [PubMed] [Google Scholar]
- 32.Denault AY, Beaubien-Souligny W, Elmi-Sarabi M, Eljaiek R, El-Hamamsy I, Lamarche Y, Chronopoulos A, Lambert J, Bouchard J, Desjardins G: Clinical significance of portal hypertension diagnosed with bedside ultrasound after cardiac surgery. Anesth Analg 124: 1109–1115, 2017. 10.1213/ANE.0000000000001812 [DOI] [PubMed] [Google Scholar]
- 33.Song P, Trzasko JD, Manduca A, Huang R, Kadirvel R, Kallmes DF, Chen S: Improved Super-resolution ultrasound microvessel imaging with spatiotemporal nonlocal means filtering and bipartite graph-based microbubble tracking. IEEE Trans Ultrason Ferroelectr Freq Control 65: 149–167, 2018. 10.1109/TUFFC.2017.2778941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nijst P, Martens P, Dupont M, Tang WHW, Mullens W: Intrarenal flow alterations during transition from euvolemia to intravascular volume expansion in heart failure patients. JACC Heart Fail 5: 672–681, 2017. 10.1016/j.jchf.2017.05.006 [DOI] [PubMed] [Google Scholar]
- 35.Beaubien-Souligny W, Rola P, Haycock K, Bouchard J, Lamarche Y, Spiegel R, Denault AY: Quantifying systemic congestion with Point-Of-Care ultrasound: Development of the venous excess ultrasound grading system. Ultrasound J 12: 16, 2020. 10.1186/s13089-020-00163-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murthi SB, Markandaya M, Fang R, Hong CM, Galvagno SM, Lissuaer M, Stansbury LG, Scalea TM: Focused comprehensive, quantitative, functionally based echocardiographic evaluation in the critical care unit is feasible and impacts care. Mil Med 180: 74–79, 2015. 10.7205/MILMED-D-14-00374 [DOI] [PubMed] [Google Scholar]
- 37.Murthi SB, Hess JR, Hess A, Stansbury LG, Scalea TM: Focused rapid echocardiographic evaluation versus vascular cather-based assessment of cardiac output and function in critically ill trauma patients. J Trauma Acute Care Surg 72: 1158–1164, 2012. 10.1097/TA.0b013e31824d1112 [DOI] [PubMed] [Google Scholar]
- 38.Gramiak R, Shah PM: Echocardiography of the aortic root. Invest Radiol 3: 356–366, 1968. 10.1097/00004424-196809000-00011 [DOI] [PubMed] [Google Scholar]
- 39.Dijkmans PA, Juffermans LJM, Musters RJP, van Wamel A, ten Cate FJ, van Gilst W, Visser CA, de Jong N, Kamp O: Microbubbles and ultrasound: From diagnosis to therapy. Eur J Echocardiogr 5: 245–256, 2004. 10.1016/j.euje.2004.02.001 [DOI] [PubMed] [Google Scholar]
- 40.Schneider AG, Hofmann L, Wuerzner G, Glatz N, Maillard M, Meuwly J-Y, Eggimann P, Burnier M, Vogt B: Renal perfusion evaluation with contrast-enhanced ultrasonography. Nephrol Dial Transplant 27: 674–681, 2012. 10.1093/ndt/gfr345 [DOI] [PubMed] [Google Scholar]
- 41.Tang S, Song P, Trzasko JD, Lowerison M, Huang C, Gong P, Lok UW, Manduca A, Chen S: Kalman filter-based microbubble tracking for robust super-resolution ultrasound microvessel imaging. IEEE Trans Ultrason Ferroelectr Freq Control 67: 1738–1751, 2020. 10.1109/TUFFC.2020.2984384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang C, Song P, Gong P, Trzasko JD, Manduca A, Chen S: Debiasing-based noise suppression for ultrafast ultrasound microvessel imaging. IEEE Trans Ultrason Ferroelectr Freq Control 66: 1281–1291, 2019. 10.1109/TUFFC.2019.2918180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang C, Zhang W, Gong P, Lok U-W, Tang S, Yin T, Zhang X, Zhu L, Sang M, Song P, Zheng R, Chen S: Super-resolution ultrasound localization microscopy based on a high frame-rate clinical ultrasound scanner: An in-human feasibility study. Phys Med Biol 66: 08NT01, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Warner L, Yin M, Glaser KJ, Woollard JA, Carrascal CA, Korsmo MJ, Crane JA, Ehman RL, Lerman LO: Noninvasive in vivo assessment of renal tissue elasticity during graded renal ischemia using MR elastography. Invest Radiol 46: 509–514, 2011. 10.1097/RLI.0b013e3182183a95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Britton N, Miller MA, Safadi S, Siegel A, Levine AR, McCurdy MT: Tele-ultrasound in resource-limited settings: A systematic review. Front Public Health 7: 244, 2019. 10.3389/fpubh.2019.00244 [DOI] [PMC free article] [PubMed] [Google Scholar]