Figure 1:
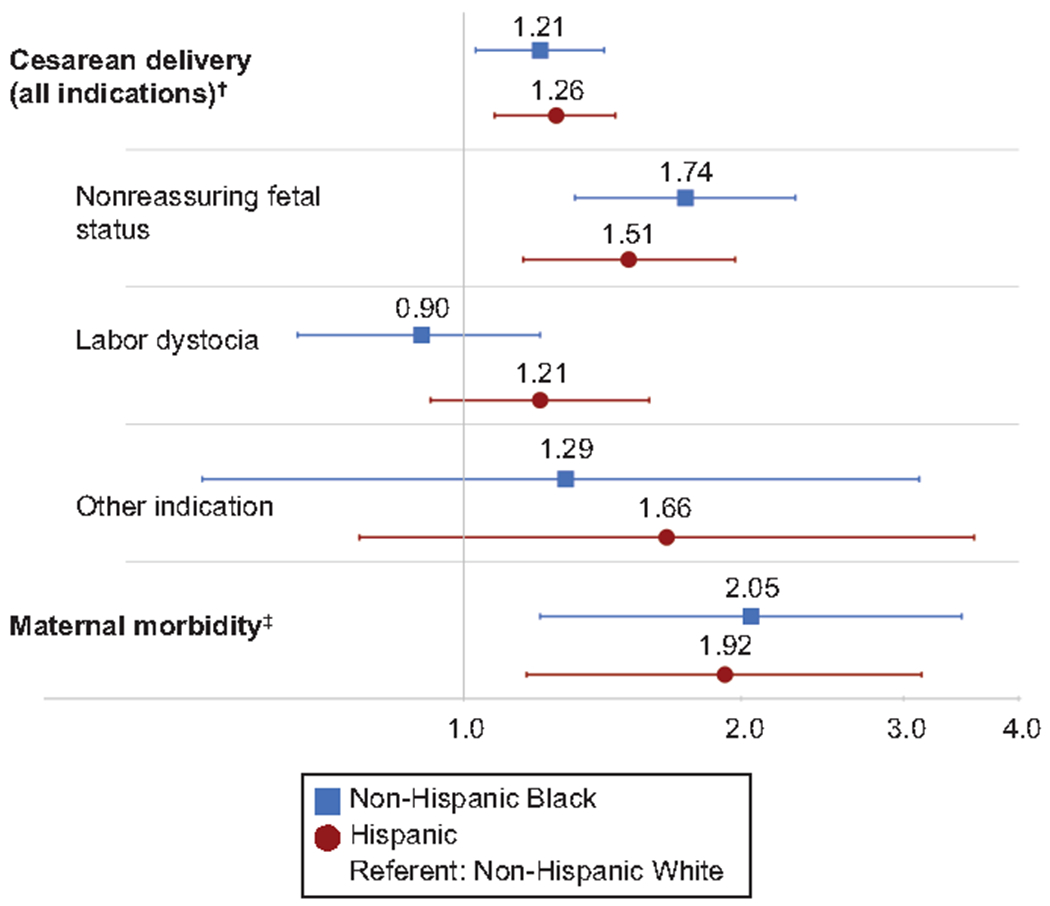
Adjusted* relative risks (aRRs) for cesarean birth and maternal morbidity, and adjusted* odds of cesarean indications, by race and ethnicity. Blue squares with blue lines indicate aRR or adjusted odds ratio (aOR), with error bars for 95% CIs for non-Hispanic Black individuals vs non-Hispanic White individuals. Red circles with red lines indicate aRR or aOR, with error bars for 95% CIs for Hispanic individuals vs non-Hispanic White individuals. Vertical grey line is an indicator for a relative risk or odds of 1.0 (line of unity). *Adjusted for clinical factors (maternal age, body mass index, modified Bishop score at admission, study group) and socioeconomic factors (employment status, insurance status, and marital status). †Vaginal delivery is the outcome referent for all models in which cesarean birth is the primary outcome, including multinomial model of indication for cesarean. ‡Composite includes transfusion of 4 or more units of packed red blood cells, transfusion of any other blood products, postpartum infection (postpartum endometritis, wound complication, cellulitis requiring antibiotics, pneumonia, pyelonephritis, bacteremia of unknown source, or septic pelvic thrombosis), intensive care unit admission, hysterectomy, venous thromboembolism, or maternal death. Maternal morbidity models are additionally adjusted for chorioamnionitis and excluded the covariate of modified Bishop score.
