Fig. 1. Renal and Intestinal Urate Physiology.
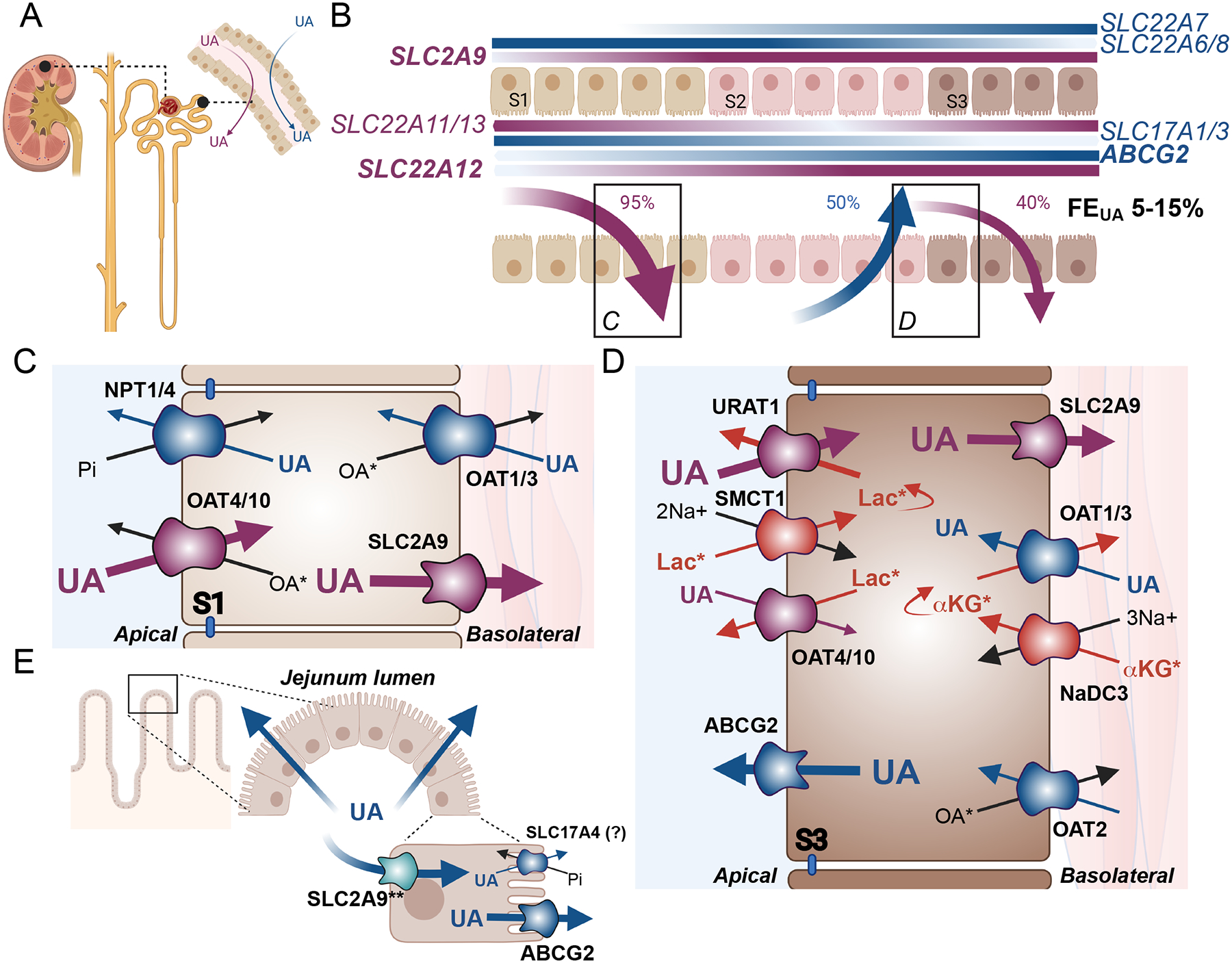
(A) The proximal tubule of the renal nephron is the principal site of urate (UA) handling through both secretion (blue arrow) and reabsorption (purple arrow). (B) Expression patterns of human urate transporter genes. Secretory transporter genes are shown in blue, while reabsorptive transporter genes are shown in purple. Gradients are displayed on the membranes of expression, with SLC22A6/7/8 and SLC2A9 coding for basolateral proteins, and ABCG2, SLC17A1/3, and SLC22A11/12/13 encoding apical transporters. The darker the color, the higher the expression, based on data from the Kidney Interactive Transcriptomics database[62]. Percentages delineate the amount of the original urate filtered load is either reabsorbed (purple arrows) or secreted (blue arrow) leading to a final fraction excretion of urate (FEUA) shown in black. Transporter protein localization and transport patterns are shown for the S1 (C) and S3 (D) segments. (C) Transporters most abundantly expressed in the S1 segments include transporters of the secretory pathway: NPT1 (SLC17A1), NPT4 (SLC17A3), OAT1 (SLC22A6) and OAT3 (SLC22A8), shown in blue, and transporters of the reabsorptive pathway: OAT4 (SLC22A11), OAT10 (SLC22A13), and SLC2A9/GLUT9 (SLC2A9), shown in purple. (D) Transporters most abundantly expressed in the S3 segment include secretory pathway transporters ABCG2/BCRP (ABCG2), OAT1, OAT2 (SLC22A7) and OAT3 shown in blue, and reabsorptive pathway transporters URAT1 (SLC22A12), SLC2A9, OAT4, and OAT10, shown in purple. Additional transporters that are functionally coupled to urate transport include the sodium cotransporters SMCT1 (SLC5A8) and NaDC3 (SLC13A3) shown in red. Blue and purple arrows indicate the direction of urate transport, while black and red arrows indicate transport of counter ions. (E) Urate is also excreted through the jejunum segment of the small intestine, where urate may enter through basolateral SLC2A9 (**well established in mice, requires further confirmation in humans), and is then secreted into the lumen primarily through ABCG2 with some potential contribution from SLC17A4 (SLC14A4).. *Some transporters have many known endogenous substrates, with only the most relevant shown. Lac: lactate; αKG: alpha-ketoglutarate; OA: organic anion; Pi: inorganic phosphate. Endogenous OAs for the OATs may include the following: OAT1: medium chain fatty acids, citrulline, prostaglandin E2 prostaglandin F2, cyclic nucleotides (cAMP, cGMP), folate[47, 50, 53]; OAT2: cAMP, GMP, GDP, GTP, cGMP, glutamate, glutarate, α-ketoglutarate, L-ascorbate, orotic acid, trigonelline, hypoxanthine, prostaglandin E2, prostaglandin F2, estrone-3-sulfate, dehydroepiandrosterone sulphate[50, 67]; OAT3: cAMP, cortisol, glutarate, prostaglandin E2, prostaglandin F2α, dehydroepiandrosterone sulphate, estrone sulphate, estradiol-17β-glucuronide, taurocholate, cholate, indoxyl sulphate [47, 50, 54, 130]; OAT4 estrone-3-sulfate, prostaglandin E2, prostaglandin F2, dehydroepiandrosterone sulphate[50, 67]; OAT10: lactate, nicotinate, glutathione, succinate[50, 92]. An additional endogenous OA for NPT1 and NP4 is inorganic phosphate co-transported in cis with Na+[57, 58]. SMCT1 mediates sodium dependent transport of monocarboxylates including short chain fatty acids, pyruvate and nicotinate[131], while NaDC3 mediates sodium coupled transport of di- and tri-carboxylates including, α-ketoglutarate, glutarate and its derivatives, citrate, succinate, and amino acid N-acetyl-L-aspartate[75].
