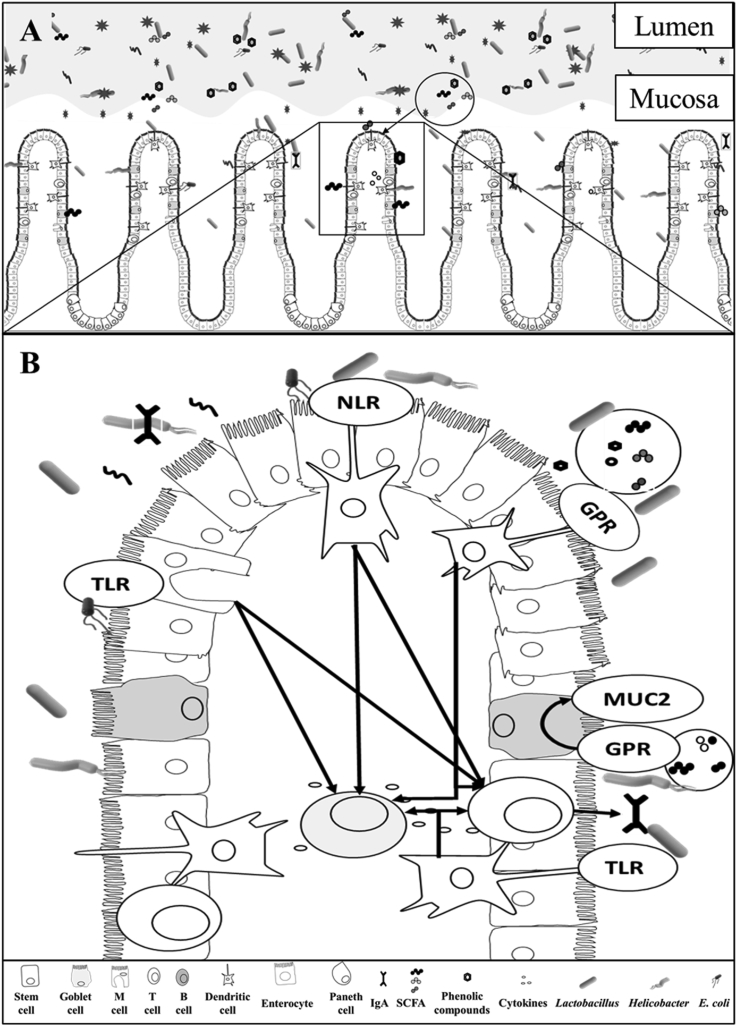
Fig. 1.
The distinct microbiota profile in the intestinal lumen and mucosa and its interaction with the immune system (Adhikari et al., 2019; Burrough et al., 2017; Mu et al., 2017; De Rodas et al., 2018), drawn by Marcos E. Duarte. (A) The luminal microbiota interacts with digesta, affecting nutrient digestion in addition to secretion of metabolites that would further affect the immune response. (B) Mucosa-associated microbiota directly crosstalk with intestinal immune cells (Arpaia et al., 2013; Belkaid and Hand, 2014; Mulder et al., 2011). Epithelial cells, M cells, and dendritic cells directly sense mucosa-associated microbiota and metabolites inducing the production of Toll-like receptors (TLR), and nucleotide-binding oligomerization domain-like receptors to recruit both T and B cells to aid in the production of cytokines and immunoglobulins (Gutzeit et al., 2014). Toll-like receptors recognize the lipopolysaccharides (LPS) in the cell wall of Gram-negative bacteria inducing the production of nuclear factor kappa β (NF-κβ), tumor necrosis factor-alpha (TNF-α), and interleukin 8 (IL-8) (Stephens and von der Weid, 2020). Goblet cells proliferation are upregulated directly by the mucosa-associated microbiota or by the short-chain fatty acids (SCFA) increasing the production of mucin 2 (MUC2) (Zhang et al., 2017). Dendritic cells recognize metabolites, including SCFA and directly activate G protein-coupled receptors (GPR) recruiting immune cells (Sina et al., 2009) inducing the intestinal immunoglobulin A (IgA) production and reducing the expression of C-X-C motif chemokine ligand 8 (CXCL8) or (IL-8), C–C motif chemokine ligand 20 (CCL20), TNF-α, and interferon gamma (IFN-γ) (Diao et al., 2019; Wen et al., 2012; Zhong et al., 2019). The production of IgA prevents the translocation of bacteria through the epithelial layer and contribute to the modulation of the mucosa-associated microbiota.