Highlights
-
•
A database research presents uptake of pneumococcal vaccine in people older than 65.
-
•
A databased retrospective research following 20,591 people older than 65 years for uptake of pneumococcal vaccine during 5 years.
-
•
The research was conducted in a large HMO that provided the vaccine free of charge.
-
•
Uptake of the vaccine was associated with other health promotion activities.
-
•
Uptake of the vaccine was not associated with visits to family health clinics.
Keywords: Pneumococcal vaccine, Older adults, Clinic visits, Early detection of cancer, Influenza vaccine
Abstract
The 23-valent pneumococcal vaccine is recommended for people aged 65 years and over, to prevent pneumonia, a leading cause of infectious morbidity in older people. This study assessed pneumococcal vaccination in people aged 65–74 years living in northern Israel who were eligible for the pneumococcal vaccine since introduction free of charge. This retrospective study used the database of Clalit Health Services, the largest health maintenance organization in Israel.
We fitted a Cox regression model to assess associations of vaccine uptake with sociodemographic and clinical characteristics, and a Wilcoxon rank-sum test and Chi-square test to assess associations of vaccine uptake with the performance of other health-related activities.
The analysis included 20,591 people. People aged 65–70 were more likely to take the vaccine than people aged 71–74 [HR = 1.8; CI: 1.6–1.9]. Jews were more likely to take it than Arabs [HR = 1.1; CI: 1.0–1.2], and men were more likely to take it than women [HR = 1.1; CI: 1.0–1.2]. In women who took the vaccine, the rate of performance of mammography was higher (61.9 % ± 45.3 vs 50.3% ± 44.5, p < 0.0001). A similar trend was found for men and women with respect to occult blood tests (36.3% ± 31.5 vs 31.7% ± 30, p < 0.0001).
Frequency of visits to family medicine clinics was negatively associated with vaccination.
Uptake of the pneumococcal vaccine was associated with some parameters indicative of self-care but not with the level of exposure to the primary health care staff.
After-hours health promotion activities by trained personnel may be an effective way to cope with the gap in performance.
1. Introduction
Streptococcus (Strep) pneumoniae is the leading cause of community acquired bacterial pneumonia (Postma et al., 2012). The most prevalent reason for visits of people over age 65 to the emergency department is infectious diseases, of which lower respiratory tract infections are the most common (Campos-Outcalt, 2014). The incidence of pneumonia and invasive infections related to Strep pneumonia tend to increase in this age group (Blasi et al., 2012, Hinman et al., 2011) and thus comprise a predominant cause for mortality (Goto et al., 2016). This poses an increasing health care concern, due to the ever-aging population (Hinman et al., 2011).
Previous studies have reported on the effectiveness of pneumococcal vaccination in reducing the incidence of pneumonia and bacteremia (Porchia et al., 2017, Dagan, 2009, Falkenhorst et al., 2017, Aliberti et al., 2014). The 23-valent vaccine is recommended for use as a single dose for people aged 65 years and over (Tomczyk et al., 2014).
A significant contribution to the literature comes from studies that accompanied an intervention program in Japan to raise the rate of vaccination in older people, with initiating subsidy for the vaccine. Factors reported to be associated with higher uptake of the pneumococcal vaccine included: having chronic diseases (Shono et al., 2018), and advice from health care staff – both physicians and nurses (Higuchi et al., 2018, Sakamoto et al., 2018, Sabapathy et al., 2014). An previous study in Israel reported lower rates of influenza vaccination among older persons of Arab origin living in the northern periphery (Sheetrit et al., xxxx).
The pneumococcal vaccination was included in 1995 in the services provided by the four health maintenance organizations in Israel, with copay; since 2008 it has been defined as a quality measure (National program, xxxx). In the winter of 2009–2010, the vaccine was introduced for all people aged 65 years and over, without copay (Immunizations for senior citizens, xxxx). The Israeli health system provides for all residents according to the national health law. Clalit Health Services (CHS) is the largest of the four health maintenance organizations in Israel. Family medicine clinics are located in all residential areas in the north of Israel and are accessible within a 30-minute drive. Visits to family physicians and nurses are free of charge.
We examined the uptake of pneumococcal vaccination among people aged 65–74 years in northern Israel, during the 5 years since the vaccine was introduced without copay for people of these ages and was a component of the quality measures program. We focused on two areas: contact with the primary health care team; and indicators of self-care in health promotion, namely, uptake of the influenza vaccine and performance of examinations for early detection of cancer. We also evaluated associations of vaccination with sociodemographic parameters and with parameters described previously as being associated with vaccination, such as chronic diseases.
2. Methods
This retrospective study included people aged 65–74 years in the northern district of CHS. Clalit Health Services is a health care provider under the Israeli National Insurance Scheme (Cohen and Rabin, 2016) for 75% of the inhabitants in this area. The CHS central register contains information on chronic conditions of all its insurees, updated regularly (Rennert and Peterburg, 2001). Visits to physicians and nurses are recorded together with such activities as prescriptions, lab tests, and vaccinations. The salaries of physicians and nurses in CHS are not related to their patients' visits and staff members are not reimbursed for health promotion activities. The data are linked to the Israel Ministry of Internal Affairs, using a unique national personal identification number.
Our study protocol followed the scheme of vaccination of people aged 65–74 years, beginning in 2010, the year that the vaccine was first offered free of charge. Continuously updated lists of persons eligible for vaccination were processed and delivered to family physicians and nurses in the community.
The study began on January 1, 2010. The study sample included all persons aged 65–74 who were eligible for vaccination on the start point of the study. They were monitored until December 31, 2015, or earlier, for those who were either vaccinated, reached the age of 75, or died during the study period. We followed the protocol used in the CHS, of identifying people in the target population for pneumococcal vaccination in the lists of insurees.
The demographic data retrieved for this study were gender, age and ethnic origin (Jews or Arabs). Data accessed in relation to contact with primary health care teams were visits to the clinic, including family physicians and nurses, during the study period. The date of vaccination was also recorded. Information was collected on factors that could indicate a positive attitude towards prevention of diseases and vaccinations: performance of screening mammography and occult blood in stool, and receiving the influenza vaccine. Other factors indicating health behavior were smoking and obesity. Obesity was represented by the Body Mass Index (BMI) (obese: BMI ≥ 30). As an indication for chronic disease, we selected hypertension, which is the most prevalent chronic disease in Israel (National health interview survey, 2013-2015). Data was collected at the entry point and throughout the study period.
The performance targets for screening examinations were defined according to the recommended intervals and the study period. For mammography, which is recommended to be performed once in two years, the defined performance target was twice during the study period. For occult blood in stool and the influenza vaccine, which are recommended to be performed annually, the defined performance target was 4 times during the study period. For people who did not complete the study period, performance of these examinations was calculated according to their time in the study. The rate of performance was determined as the mean value of performance of all the participants. Visits to family physicians and practice nurses were recorded for the study period and presented as mean visits per year. Values higher than the median value represented more frequent visits.
2.1. Statistical analysis
The data were analyzed by SAS version 9.4. P-values of less than 0.05 were considered significant. Categorical data were reported as numbers (%) and association with vaccination was performed using the Chi-square test. Rate of performance of screening mammography and occult blood in stool, and rate of performance of the influenza vaccine were reported as mean ± SD and median. Between-group comparisons were performed using the Wilcoxon rank–sum test for independent samples. A Cox regression model was designed to examine the prediction of uptake of the pneumococcal vaccine, taking into account variables of demographics, hypertension and smoking.
The research was approved by the Helsinki Committee of CHS, number 0142-16-com2. A waiver of informed consent was obtained due to the use of data anonymization.
3. Results
The cohort numbered 20,591 people aged 65–74 who were eligible for pneumococcal vaccination.. The mean age at baseline was 69.5 ± 2.5 years median 69.7). People were monitored for an average of 3.9 ± 1.9 years (median −4.2).
Vaccination was documented for 3315 (15.2%) persons until the end of the monitoring period. Among those who were vaccinated compared to those who were not vaccinated, there was a higher proportion of men, Jews, smokers, and people below the age of 70 (Table 1). Hypertension was negatively associated with vaccination. There was no difference in the rate of obesity between the groups.
Table 1.
Characteristics of people aged 65–74 by vaccination status.
| Variables | Vaccination status |
Significance | |||
|---|---|---|---|---|---|
|
All the people in the study N = 20,591 Number (%) |
People who were not vaccinated N=17,456 Number (%) |
People who were vaccinated N=3,135 Number (%) |
|||
| Gender | Women | 10,863 (52.8) | 9,296 (85.6) | 1,567 (14.4) | 0.0007 |
| Men | 9,728 (47.2) | 8,160 (83.9) | 1,568 (16.1) | ||
| Ethnic origin | Arab | 6,264 (30.4) | 5,358 (85.5) | 906 (14.5) | 0.0443 |
| Jewish | 14,327 (69.6) | 12,098 (84.4) | 2,229 (15.6) | ||
| Obesity (BMI ≥ 30) | No | 1,364 (52.7) | 1,195 (87.6) | 169 (12.4) | 0.5278 |
| Yes | 1,226 (47.3) | 1,084 (88.4) | 142 (11.6) | ||
| Smoking | No | 14,549 (70.7) | 12,414 (85.3) | 2,135 (14.7) | 0.0006 |
| Yes | 6,042 (29.3) | 5,042 (83.5) | 1,000 (16.5) | ||
| Hypertension | No | 6,550 (31.8) | 5,400 (82.4) | 1,150 (17.6) | <0.0001 |
| Yes | 14,041 (68.2) | 12,056 (85.9) | 1,985 (14.1) | ||
| Age at start of the study | 65–70 | 13,855 (67.3) | 11,145 (80.4) | 2,710 (19.6) | <0.0001 |
| 71–74 | 6,736 (32.7) | 6,311 (93.7) | 425 (6.3) | ||
| Annual visit to the clinic (Mean/person) | <=9 | 14,324 (69.6) | 12,023 (83.9) | 2,301 (16.1) | <0.0001 |
| >9 | 6,267 (30.4) | 5,433 (86.7) | 834 (13.3) | ||
| Annual visit to the family doctor (Mean/person) | <=12 | 13,615 (66.1) | 11,435 (84.0) | 2,180 (16.0) | <0.0001 |
| >12 | 6,976 (33.9) | 6,021 (86.3) | 955 (13.7) | ||
| Annual visit to the family nurse (Mean/person) | <=6 | 15,903 (77.2) | 13,400 (84.3) | 2,503 (15.7) | 0.0002 |
| >6 | 4,688 (22.8) | 4,056 (86.5) | 632 (13.5) | ||
A Cox regression model was designed to examine the parameters associated with uptake of the pneumococcal vaccine. The parameters were gender, ethnic origin, smoking, hypertension and age group. Due to missing data we were not able to include data on obesity. In the regression model (Table 2), younger age at entry into the study (65–70 years) predicted vaccination more than did older age (71–74 years) [HR = 1.8; 95% CI: 1.6–1.9). Being Jewish predicted vaccination more than did being Arab [HR = 1.1; 95% CI: 1.0–1.2]. Men were also more likely to be vaccinated than women [HR = 1.1; 95% CI: 1.0–1.2]. Smoking did not predict vaccination. People with hypertension were less likely to take the vaccine than those without hypertension [HR = 0.9; 95% CI: 0.8–0.9] (Table 2).
Table 2.
Cox regression analysis of factors associated with uptake of pneumococcal vaccine by people aged 65–74.
| Variables | HR | 95% CI | p-value |
|---|---|---|---|
| Gender (Men vs. Women) | 1.12 | 1.04–1.21 | 0.002 |
| Ethnic origin (Jewish vs. Arab) | 1.14 | 1.05–1.23 | 0.001 |
| Smoking | 0.991 | 0.915–1.07 | 0.834 |
| Hypertension | 0.885 | 0.823–0.952 | 0.001 |
| Age (65–70 vs. 71–74) | 1.79 | 1.61–1.99 | <0.0001 |
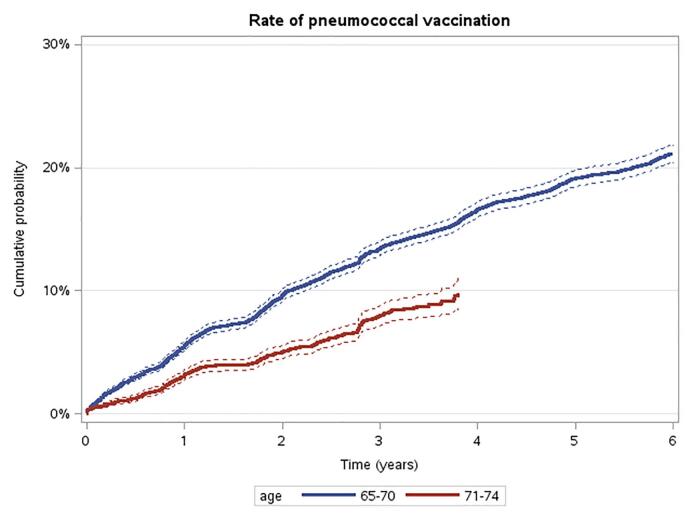
During the study period, the mean annual number of visits to the practice was 7.7 ± 5.2 per person. More visits were made to family doctors than to nurses (10.7 ± 7.5 vs 4.8 ± 4.4 respectively). More frequent visits were defined as higher than median in each category. More frequent visits of all kinds were negatively associated with vaccination (Table 1). The comparison between age groups regarding time to vaccination is presented as the cumulative probability of pneumococcal vaccination over time by age group (Fig. 1). This comparison shows that at any point during the study period younger people were vaccinated more than older people.
Fig. 1.
Rate of pneumococcal vaccination by age group. The comparison between age groups regarding time to pneumococcal vaccination was significant according to the Log-Rank test (p < 0.0001).
Among people who were vaccinated, the rate of performance of examination for early detection of cancer was higher than among those who were not vaccinated. This was reflected both in mammography among women, and in occult blood examinations among both genders (61.9 % ± 45.3; median: 66.7 vs 50.3% ± 44.5; and 36.3% ± 31.5; median: 33.3 vs 31.7% ± 30, respectively; p < 0.0001 for both). The rate of performance of the influenza vaccination was lower among those who were vaccinated for pneumonia, than among those were not (59.7% ± 35.4; median: 66.7 vs 63.5% ± 38.9; median: 83.3, p < 0.0001).
4. Discussion
Our study followed the uptake of 23-valent pneumococcal vaccination from the time of introduction free of charge. Uptake of the pneumococcal vaccine varied among people by age, being higher among relatively younger (aged 65–70) than older (aged 71–74) people.
Our approach of exploring associations between uptake of the vaccine and other activities of self-care yielded diverse outcomes. On one hand, actions for early detection of cancer, such as screening mammography and occult blood tests, were associated with higher rates of pneumococcal vaccination. These associations may indicate a population that adheres more closely to health-related behaviors connected to early detection of cancer. On the other hand, we found a negative association with the rate of performance of influenza vaccination. Two studies from Japan assessed the introduction of subsidized pneumococcal vaccination by web-based questionnaires (Shono et al., 2018, Sakamoto et al., 2018). One of these studies reported an association between the two vaccines, referring to people being “ever vaccinated” during the previous three years (Sakamoto et al., 2018). The other study reported a non-significant relationship between them, referring both to annual and “sometime vaccination” (Shono et al., 2018). Another study found an association between vaccinating for both diseases, but not limited to an older age (Dower et al., 2011). Our study referred to annual vaccination for influenza, and our data were based on a performance report.
Eligibility for subsidy was indicated as an important factor contributing to uptake of the vaccine (Shono et al., 2018, Higuchi et al., 2018). Our study followed people from the time that the vaccine was provided free of charge, thus closing financial gaps.
Exposure to the primary health care team is expected to contribute to performance of activities for health promotion. Surprisingly, in our study, “more visits to the practice” was associated with a lower rate of vaccination. This outcome could be interpreted by the fact that the pneumococcal vaccine was introduced into the routine work of CHS without specific training of the team members. A higher proportion of the younger group in the study (aged 65–70) was vaccinated, and the progression of performance was higher in this group. It seems that longer and more frequent exposure to the primary health care staff did not result in better vaccination outcomes. This could be due to not using appointments as an opportunity for promoting vaccination or not fitting the promotion individually, according to age, state of health and other health needs.
A study on Alberta Healthcare Services in Calgary, Canada, evaluated the association between pneumococcal vaccination and acute visits to the doctor. It reported a higher rate of vaccination in the visiting older people, with outcomes for both primary and long stay settings (Sabapathy et al., 2014). Our study is community-based, collecting data from various clinics of different sizes spread around the district.
Hypertension, as the most prevalent chronic disease, also represents an opportunity for higher exposure to the primary health care staff. Hypertension was found to be negatively associated with the rate of vaccination. Associations with chronic diseases have been reported in previous studies: the role of chronic conditions was reported from a web-based survey that evaluated the benefit of subsidizing the vaccine for people over the age of 65. The survey showed an association between uptake of vaccination and having “any disease under treatment”, which correlated to chronic diseases (Shono et al., 2018). In contrast to that study, based on self-reporting, our study used the updated valid database of CHS (Cohen and Rabin, 2016).
As with other health-related activities, a patient’s decision to be vaccinated is influenced by various factors. Better performance of pneumococcal vaccination is associated with perceptions of its effectiveness in preventing pneumonia (Higuchi et al., 2018) and of the severity of pneumonia (Sakamoto et al., 2018). Information provided by reading materials in the practice resulted in an increased rate of vaccination in Singapore (Ho et al., 2019). In Japan, recommendation for vaccination, provided by medical personnel, not necessarily physicians (Sakamoto et al., 2018), or family physicians (Shono et al., 2018, Higuchi et al., 2018), was a contributing factor. Intervention by training family physicians in preventive health care has also led to a high rate of vaccination (Higuchi et al., 2018).
4.1. Strengths of the study
The strengths of our study include its considerable sample size and the comprehensiveness and validity of the available data, based on performance. Our data, sourced from the quality measures program of CHS, are continuously updated (Cohen and Rabin, 2016, Cohen et al., 2010). Members of CHS are insured nationally and listed for personal identified primary care physicians. This enables complete follow-up of the cohort and of their visits to family care clinics. The structure of the Israeli health system, providing primary health care services free of charge, including vaccination, enabled us to analyze vaccination regardless of financial considerations.
4.2. Limitations of the study
While we had information on the number of clinical visits, we did not have information on their content. Thus, we did not have information on whether the primary health care team approached people regarding vaccination. Likewise, we could not identify “persistent refusers” of the pneumococcal vaccine, for whom any effort for persuasion would be predicted to fail. “Frequency of visits” was retrieved for the time frame of the study, but not specifically in relation to the date of vaccination. The same was also true for the performance of occult blood testing and mammography. We assume that performance of the examinations and visits to the practice represent general self-care behavior and do not change with time. The information related to smoking was retrieved at entry and during the study period. From our experience it is reasonable that in that age group documentation on smoking is a new documentation, rather than new information. Obesity data were also collected at any point during the study. Obesity might be not accurate if people lost weight during the study period, thus weakening its value in the analysis. Data on hypertension were not analyzed in relation to the date of vaccination, which could limit the power of the analysis. However, hypertension is the most common chronic disease (Rennert and Peterburg, 2001), and chronic diseases are often accompanied by other chronic diseases, so we believe that this is still an indicator for chronic morbidity.
5. Conclusions
Uptake of pneumococcal vaccination was higher in the younger age group (age 65–70) and correlated with performance of some activities for health promotion. The rate of vaccination was not associated with exposure to the practice, according to frequency of visits or having a chronic disease. This raises concerns that the forum for promoting pneumococcal vaccination has not been sufficiently used in the primary care setting. The findings suggest an opportunity for implementing a structured intervention program by trained personnel to initiate visits dedicated to the promotion of vaccination against pneumonia in older people.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
We thank Ms. Adi Edri-Shor for the data mining, Ms. Hila Kefir for research coordination and Ms. Shiraz Vered for the statistical analysis.
References
- Aliberti S., Mantero M., Mirsaeidi M., Blasi F. The role of vaccination in preventing pneumococcal disease in adults. Clin. Microbiol. Infect. 2014;20:52–58. doi: 10.1111/1469-0691.12518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blasi F., Mantero M., Santus P., Tarsia P. Understanding the burden of pneumococcal disease in adults. Clin. Microbiol. Infect. 2012;18:7–14. doi: 10.1111/j.1469-0691.2012.03937.x. [DOI] [PubMed] [Google Scholar]
- Campos-Outcalt D. Pneumococcal vaccines for older adults: getting the timing right. J. Fam. Pract. 2014;63:730–733. [PubMed] [Google Scholar]
- Cohen, R, Rabin, G. Membership in Sick Funds 2016. Jerusalem; 2017. <http://www.btl.gov.il>.
- Cohen A.D., Dreiher J., Regev-Rosenberg S., Yakovson O., Lieberman N., Goldfracht M., Balicer R.D. The quality indicators program in Clalit Health Services: the first decade. Harefuah. 2010;149:204–209. (Hebrew) [PubMed] [Google Scholar]
- Dagan R. New insights on pneumococcal disease: What we have learned over the past decade. Vaccine. 2009;27:C3–C5. doi: 10.1016/j.vaccine.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Dower J.o., Donald M., Begum N., Vlack S., Ozolins I. Patterns and determinants of influenza and pneumococcal immunisation among adults with chronic disease living in Queensland, Australia. Vaccine. 2011;29(16):3031–3037. doi: 10.1016/j.vaccine.2011.01.116. [DOI] [PubMed] [Google Scholar]
- Falkenhorst G., Remschmidt C., Harder T., Hummers-Pradier E., Wichmann O., Bogdan C., Ho P.L. Effectiveness of the 23-valent pneumococcal polysaccharide vaccine (PPV23) against pneumococcal disease in the elderly: systematic review and meta-analysis. PLoS ONE. 2017;12(1) doi: 10.1371/journal.pone.0169368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto T., Yoshida K., Tsugawa Y., Camargo C.A., Hasegawa K. Infectious disease–related emergency department visits of elderly adults in the United States, 2011–2012. J. Am. Geriatr. Soc. 2016;64(1):31–36. doi: 10.1111/jgs.13836. [DOI] [PubMed] [Google Scholar]
- Higuchi M., Narumoto K., Goto T., Inoue M. Correlation between family physician’s direct advice and pneumococcal vaccination intention and behavior among the elderly in Japan: a cross-sectional study. BMC Family Pract. 2018;19:153. doi: 10.1186/s12875-018-0841-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinman A.R., Orenstein W.A., Schuchat A. Vaccine-preventable diseases, immunizations, and the Epidemic Intelligence Service. Am. J. Epidemiol. 2011;174(suppl 11):S16–S22. doi: 10.1093/aje/kwr306. [DOI] [PubMed] [Google Scholar]
- Ho H.J., Tan Y.-R., Cook A.R., Koh G., Tham T.Y., Anwar E., Hui Chiang G.S., Lwin M.O., Chen M.I. Increasing influenza and pneumococcal vaccination uptake in seniors using point-of-care informational interventions in primary care in Singapore: a pragmatic, cluster-randomized crossover trial. Am. J. Publ. Health. 2019;109(12):1776–1783. doi: 10.2105/AJPH.2019.305328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Immunizations for senior citizens. Senior health. Ministry of Health. <https://www.health.gov.il/English/Topics/SeniorHealth/HealthPromo/Pages/Vaccines>.
- National health interview survey INHIS-3, 2013-2015: selected findings. Israel Center for Disease Control (ICDC). Publication 2017;374. <https://www.health.gov.il/publicationsfiles/inhis_3.pdf>.
- National program for quality indicators in community healthcare. Elderly adults-definition and results. <https://en.israelhealthindicators.org/elderly-adults>.
- Porchia B.R., Bonanni P., Bechini A., Bonaccorsi G., Boccalini S. Evaluating the costs and benefits of pneumococcal vaccination in adults. Expert Rev. Vaccines. 2017;16(2):93–107. doi: 10.1080/14760584.2017.1242419. [DOI] [PubMed] [Google Scholar]
- Postma D.F., Van Werkhoven C.H., Huijts S.M., Bolkenbaas M., Oosterheert J.J., Bonten M.J., et al. New trends in the prevention and management of community-acquired pneumonia. Neth. J. Med. 2012;70:337–348. [PubMed] [Google Scholar]
- Rennert G., Peterburg Y. Prevalence of selected chronic diseases in Israel. Israel Med. Assoc. J. 2001;3:404–408. http://www.ncbi.nlm.nih.gov/pubmed/11433630 [PubMed] [Google Scholar]
- Sabapathy D., Strong D., Myers R., Li B., Quan H. Pneumococcal vaccination of the elderly during visits to acute care providers: Who are vaccinated? Prev. Med. 2014;62:155–160. doi: 10.1016/j.ypmed.2013.11.009. [DOI] [PubMed] [Google Scholar]
- Sakamoto A., Chanyasanha C., Sujirarat D., Matsumoto N., Nakazato M. Factors associated with pneumococcal vaccination in elderly people: a cross-sectional study among elderly club members in Miyakonojo City, Japan. BMC Publ. Health. 2018;18:1172. doi: 10.1186/s12889-018-6080-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheetrit, A, Wallen, B, Hoffert, A. Health disparities: Influenza vaccines, data from the knowledge center on health inequality. The National Knowledge Center on Inequality of the Ministry of Health, at the Gartner Institute for Epidemiology and Health Policy Research (Hebrew).
- Shono A., Hoshi S.-L., Kondo M. The impact on vaccination coverage following introduction of a routine pneumococcal vaccination programme for the elderly in Japan. Vaccine. 2018;36(39):5886–5890. doi: 10.1016/j.vaccine.2018.08.023. [DOI] [PubMed] [Google Scholar]
- Tomczyk S., Bennett N.M., Stoecker C., Gierke R., Moore M.R., Whitney C.G., Hadler S., Pilishvili T. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged≥ 65 years: recommendations of the Advisory Committee on Immunization Practices (ACIP) Morb. Mortal. Wkly Rep. 2014;63:822–825. [PMC free article] [PubMed] [Google Scholar]