Abstract
The worldwide coronavirus disease 2019 (COVID-19) pandemic has seriously affected not only physical health but also mental wellbeing (i.e mental stress and suicide intention) of numerous urban inhabitants across the globe. While many studies have elucidated urban parkland enhances and mental wellbeing of urban residents, the potential for parkland to mitigate mental health burden imposed by the COVID-19 has received no attention. This nationwide study systematically explored the association between parkland, the COVID-19 pandemic situation and mental wellbeing from 296 cities in China. The study innovatively used big data from Baidu Search Engine to assess city-level mental wellbeing, thereby enabling comparisons among cities. The results show that the provision of parkland is positively associated with mental wellbeing during the COVID-19 epidemic. For COVID-19-related indicators, the geographical distance to Wuhan city, work resumption rate, and travel intensity within the city are also positively associated with mental wellbeing, while the number of COVID-19 infections and the proportion of migrants from Hubei Province for each city are negatively associated with mental wellbeing. Last, the most important finding is that parkland reduces the negative effect of COVID-19 on mental wellbeing during the COVID-19 epidemic. To achieve the goal of promoting mental wellbeing through urban planning and design during the future pandemics, policymakers and planners are advised to provide more well-maintained and accessible parkland and encourage residents to use them with proper precautions.
Keywords: Parkland, COVID-19, Mental wellbeing, Buffer effect, Big data
1. Introduction
As of July 5, 2020, the COVID-19 virus had infected more than 10 million people and caused more 500,000 deaths worldwide (World Health Organization, 2021). In addition to posing a threat to physical health, the epidemic also imposes a considerable psychological burden; thus, the World Health Organization and some scholars have begun to call for attention to mental disorders (Campion et al., 2020; Holmes et al., 2020) and suicide prevention (Gunnell et al., 2020) during the pandemic.
While the exact mental health burden of the current COVID-19 is still too early to measure because many countries are witnessing news waves of virus cases. However, previous natural disasters offer some valuable insights. Some studies have suggested that some people experiencing major natural disasters had tremendous pain for various reasons, financial lost, feeling of insecurity, or losing relatives or friends (Tsuboya et al., 2016). For example, Munro et al. (2017) found that people's depression and anxiety symptoms increase after a flood in UK. Hogg et al. (2016) pointed out that people had worse mental health after experiencing the 2011 Christchurch earthquake in New Zealand. In recent years, increasing numbers of scholars have begun to focus on the psychological impact of major epidemic outbreaks (Jalloh et al., 2018; Page et al., 2011; Pfefferbaum et al., 2012; Shultz et al., 2015; Thomas, 2015; Yadav and Rawal, 2015). Compared with natural disasters, major epidemic diseases have a more pronounced impact on mental wellbeing because major epidemic diseases tend to last longer and lead to citywide lockdowns. For instance, Jalloh et al. (2018) found that one year after the outbreak of Ebola, people's posttraumatic stress disorder (PTSD), anxiety and depression symptoms increased. Pfefferbaum et al. (2012) found that novel influenza A (H1N1) brought psychological trauma to vulnerable groups, such as the elderly, children and pregnant women. A recent study focusing on COVID-19 found that various factors, such as potential infection risk, living in the worst affected areas, experiencing quarantine and experiencing unemployment caused by the epidemic, are related to mental disorders (Shi et al., 2020).
Scholars and policymakers have become increasingly aware of the mental health benefits of parkland, especially for urban residents (van den Bosch and Sang, 2017). A large number of empirical studies confirmed that urban parkland is beneficial to mental wellbeing (Dzhambov and Dimitrova, 2014; Grilli et al., 2020; Li et al., 2019; Roberts et al., 2019; Veitch et al., 2020; Wan et al., 2020; Wolf and Wohlfart, 2014; Wu et al., 2020; Yigitcanlar et al., 2020). There are at least four underlying pathways explaining why green spaces can improve mental health and wellbeing (Markevych et al., 2017).
First, as a large green infrastructure, parkland can mitigate the negative effect of air pollution on people' mental wellbeing (Su et al., 2011; Vieira et al., 2018). For example, Vieira et al. (2018) found that vegetation in urban parkland the ecological function of air purification, which is beneficial for both physical and mental health. Su et al. (2011) found that public parkland has the lowest pollutant concentrations of nitrogen dioxide (NO2) and fine particulate (PM2.5) on average.
The second pathway linking parkland and its level of biodiversity to mental wellbeing is associated with the environmental psychological factor. Environmental psychological theories, such as stress reduction theory (SRT) and attention restoration theory (ART), highlighted the role of the natural environment in reducing psychological stress (Kaplan, 1995; Ulrich et al., 1991). For instance, Li et al. (2019) conducted an experiment in China which indicated that after visiting the park, people's affected states, such as relaxation and contentment, increased. Lin et al. (2019) suggested that urban parks help visitors to restore their attention level. Payne (2008) found that frequent visit to urban parks provide people with restorative experience in UK. Ojala et al. (2019) suggested that visiting urban greenspace has psychological restorative effects for people. An online survey in Norway indicated that the amount of greenspace in urban parks influences people's park preference and restorative experience (Nordh et al., 2011).
Third, numerous studies have documented that the presence of urban parks may encourage people to undertake physical activity (Cohen et al., 2007; Kaczynski et al., 2008; Wang et al., 2020; Wolf and Wohlfart, 2014). Urban parks can attract residents living around it to visit and take physical activity, such as walking, running and cycling (Xie et al., 2021)). Research evidence further pointed out that undertaking physical activity in an urban park, often called green exercise, is more beneficial to mental wellbeing than indoor physical activity (Thompson Coon et al., 2011). Also, duration of the visit and green exercise (e.g., walking) within the park play an important role in shaping mental wellbeing (De Bloom et al., 2017). For example, Kaczynski et al. (2008) found that park features and amenities are significantly related to park-based physical activity. Floyd et al. (2011) pointed out that recreation facilities of parks can attract surrounding residents to undertake park-based physical activity.
Last, parkland also facilitates social cohesion, which is beneficial for mental wellbeing (Gómez et al., 2018; Jennings and Bamkole, 2019; Peters et al., 2010). Most green spaces, such as parks or greenways, are also the public spaces for people to socialize with one another. Scholars found that park-based activities, such as dog walking, can enhance the dog owners' social cohesion, since they can share the experience of taking care of dogs with each other (Gómez et al., 2018).
Previous studies also support that exposure to green spaces can moderate mental health burden imposed by stressful life events or severe diseases (Cimprich and Ronis, 2003; Gidlöf-Gunnarsson and Öhrström, 2007; Marselle et al., 2019; Orsega-Smith et al., 2004; Ottosson and Grahn, 2008; Van Den Berg et al., 2010; Wells and Evans, 2003). For example, conducting walking or exercise in parks can help people temporarily forget about stressful events, which otherwise may lead to worse mental health (Marselle et al., 2019; Orsega-Smith et al., 2004). In addition, contact with people inside the park can also help people release stress and pressure (Orsega-Smith et al., 2004). Furthermore, the restorative effects of vegetation (i.e., being away) in urban parks (i.e., being away) can help people recover from stressful events (Kaplan, 1995). Evidence suggests that exposure to green spaces can reduce the negative emotions associated with stressful life events or breast cancer (Cimprich and Ronis, 2003; Ottosson and Grahn, 2008).
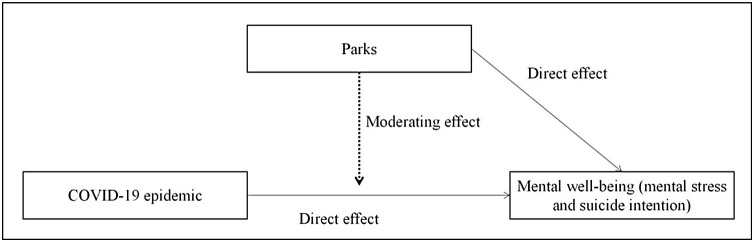
As a major global epidemic disease, COVID-19 has brought great psychological burdens (Campion et al., 2020; Holmes et al., 2020). Greenspace such as parkland and indoor greenery accrue mental health benefits, as demonstrated by evidence (Grilli et al., 2020; Li et al., 2019; Roberts et al., 2019; Veitch et al., 2020; Wan et al., 2020, Wang et al., 2021a, b). However, it is still unclear whether greenspace can mitigate mental health burden imposed by the COVID-19 pandemic, so it is necessary to examine whether and how parkland reduces the mental health burden during the pandemic. In this study, we postulate parkland may directly affect mental wellbeing, and it may also moderate the negative mental health burden imposed by the COVID-19 (Fig. 1 ). The rationale for such hypothesis is in the abovementioned pathways, via which the mental health burden of COVID-19 is potentially mitigated by parkland. This study extends previous research in several respects. First, the study enhances our knowledge of the direct effect of urban parkland on mental wellbeing during the COVID-19 epidemic. Second, the study further explores the indirect buffer effect of parkland regarding the association between the COVID-19 epidemic and mental wellbeing. Third, the study reveals the relationship between the COVID-19 epidemic and mental wellbeing in a Chinese context. Last but not least, this study contributes to the methodological development. We used big data retrieved with Baidu Search Engine, the dominating search engine in China, to assess urban residents' mental wellbeing in 296 cities in China during the pandemic. This study extends previous research in several respects. First, the study enhances our knowledge of the direct effect of urban parkland on mental wellbeing during the COVID-19 epidemic in China. Second, the study further explores the indirect buffer effect of parkland regarding the association between the COVID-19 epidemic and mental wellbeing. Third, the study also reveals the relationship between the COVID-19 epidemic and mental wellbeing in a Chinese context. Last but not least, this study contributes to the methodological development. We used big data retrieved with Baidu Search Engine, the dominating search engine in China, to assess urban residents' mental wellbeing in 296 cities in China during the pandemic.
Fig. 1.
Theoretical framework of this study. The amount of parkland may directly affect mental wellbeing, and it may also moderate the negative mental health burden imposed by the COVID-19 pandemic.
2. Data and methods
2.1. Data
The research area covered 31 provinces in China. The basic geographical units were 296 prefecture-level cites, as well as four special municipality including Beijing, Tianjin, Shanghai, and Chongqing, as of 2019. The dependent variables in this study were collected from Baidu Search Engine big data provided by Baidu Inc. (http://index.baidu.com/).
Data related to the COVID-19 epidemic were from the number of cases released by the National Health Commission in China (http://www.nhc.gov.cn/) and Baidu migration and travel big data (https://qianxi.baidu.com/). Parkland and other data were from the Department of Urban Social Economic Survey of the National Bureau of Statistics (National Bureau of Statistics, 2019; China Statistics Press, 2019) and Data Center for Resources and Environmental Sciences, Chinese Academy of Sciences (http://www.resdc.cn/Default.aspx).
2.2. Measures
2.2.1. Outcome
At present, Baidu is the most widely used search engine in China, with more than 600 million active users in China. Baidu Search Index (which is similar to Google Search Trends) shows the weighted search frequency of different keywords (http://index.baidu.com/). Previous studies have used this index to assess people' health status or health-related behaviors at the city level, such as physical activity (Cesare et al., 2019) and mental wellbeing (Chen et al., 2020). In this study, we used this index to measure urban residents' mental wellbeing for 296 cities in China during the COVID-19 epidemic.
In this study, the average value of Baidu Search Index of each city between January 30 to March 8, 2020 were retrieved. Previous studies found that the higher the search intensity of certain keywords related to negative emotional problems in a certain city was, the poorer the mental wellbeing of city residents was (Chen et al., 2020). This kind of method has been widely used for measuring people's behaviors and state in health-related studies during COVID-19. For example, Lin et al. (2020) used Google Search Index to measure people's hygiene habits and behaviors among 21 countries during COVID-19. Husnayain et al. (2020) applied Google Search Index for measuring people's awareness of prevention against the epidemic in Taiwan. Kluger and Scrivener (2020) pointed out that Google Search Index can reflect people's COVID-19-related symptoms, while Walker et al. (2020) found Google Search Index reflects people's loss-of-smell COVID-19-related symptoms in Italy, Spain, UK, USA, Germany, France, Iran, and The Netherlands. Hong et al. (2020) used Google Search Index to measure people's telemedicine behaviors in USA during COVID-19. This study constructed two types of mental wellbeing related indices. (1) Mental stress index: this index included average search intensity for the three search keywords, including “mental health/stress (心理健康/压力)”, “depression (抑郁)” and “anxiety (焦虑)”. Research on global burden of disease indicated that depression and anxiety were the two most serious mental disorder diseases from 1990 to 2015 (Vos et al., 2016). Therefore, the above three keywords can reflect residents' attention on their mental stress level. We used principal component analysis (PCA) to reduce the search intensity of these three keywords into one variable. (2) Suicide index: this index included average search intensity for “suicide (自杀)”. This keyword can reflect residents' intention to commit suicide and attention to methods of suicide; thus, it measures the suicidal ideation of residents for each city (Chen et al., 2020).
To take into account the different number of internet users in different cities, the two indexes were divided by the number of internet users in each city. Number of internet users is the sum of the number of mobile phone users and internet broadband users, both of which were derived from the Statistical Yearbook of Chinese Cities 2019, which was provided by the Department of Urban Social Economic Survey of the National Bureau of Statistics (National Bureau of Statistics, 2019; China Statistics Press, 2019). Last, we standardized the two indices. Higher scores indicate poorer mental wellbeing of city residents.
2.2.2. Parkland indicator
Following previous studies (Chong et al., 2013), the key independent variable in this study was the proportion of parkland area (%) in a city. The data were derived from the Statistical Yearbook of Chinese Cities 2019, which was provided by the Department of Urban Social Economic Survey of the National Bureau of Statistics (National Bureau of Statistics, 2019; China Statistics Press, 2019). Specifically, the amount of parkland area was measured by the item of “area of parks and green spaces” in the yearbook. The proportion of parkland area was calculated as the area of parkland to the total area of a city (km2/km2*100 %). We further validated this parkland indicator in two steps. First, the Statistical Yearbook of Chinese Cities 2019 also provides the area of green land for the whole city. The Spearman coefficients of proportion of green land for the whole city versus proportion of parkland area showed associations of 0.969 (p < 0.001), which indicates that our parkland indicator can also reflect the presence of greenspace for the whole city. Second, following Li et al. (2020), we collected polygon data for parks in China using the Autonavi electronic navigation map (AMAP, https://ditu.amap.com) and recalculated proportion of parkland area for each city. The Spearman coefficients between two indicators showed associations of 0.886 (p < 0.001), which validates the accuracy of parkland indicator from Statistical Yearbook.
2.2.3. COVID-19 indicators
We selected five COVID-19-related indicators following previous studies (Shi et al., 2020). (1) COVID-19-related policy factor: previous studies show that government's interventions and policies to cope with major public health crises influence people's mental wellbeing (Holmes et al., 2020). This study used the presence of lockdown policy (yes vs. no) to measure the government regulation factor. According to the Covid-19 Prevention and Control Plan (National Health Commission of the People’s Republic of China, 2020), different cities had different levels of risk and different policies. Cities were classified as high-risk, middle-risk and low-risk levels (supplement file). Middle-risk and low-risk cities did not regulate residents' outdoor activities, while high-risk cities did so with lockdown policies. The lockdown policies suspend all traffic within a city should be suspended (e.g. bus, rail, taxi, and cars) and limit all outdoor activities, and/or allow only one or two people in each household to go shopping once a day. This lockdown policies are dynamic. Most cities only conducted lockdown for a short period between January 30 to March 8. However, cities in Hubei province have longer and stricter lockdown. For example, Wuhan was completely locked down in this period, which prohibits any outdoor activities, except essential activities. Some cities allow only outdoor activities within their neighbourhoods. (2) COVID-19-related infection factor: the number of infections can directly reflect the severity of the epidemic in a city, which may trigger panic and affect the mental wellbeing of residents (Tausczik et al., 2012). This study used the number of COVID-19 infections (numbers) to measure the severity of the COVID-19 epidemic in a city. (3) COVID-19-related geographical factor: literature indicated that the geographical distance to a severely affected epidemic area can affect residents' assessment of their own affected risk and thus has influence on their mental wellbeing (Shi et al., 2020). This study used the geographical distance to Wuhan city (km) to measure the geographical factor. (4) COVID-19-related population mobility factor: previous studies showed that long-distance travel is an important factor affecting the spread of COVID-19, which also places a certain psychological burden on people (Wang et al., 2020). Baidu migration and travel big data provide the proportion of the population flowing into each city; therefore, we calculated the proportion of migrants from Hubei province, which include Wuhan city and nearby cities with large number of infected cases, during the epidemic for each city (%). Last, many people stopped work compulsorily or voluntarily during the COVID-19 pandemic, which also affected residents' mental wellbeing (Holmes et al., 2020). We used work resumption rate to measure the state of recovery to normal life in each city. Baidu migration and travel big data provide a migration intensity index for each city. This index measures the size of the population flowing into each city. Work resumption rate for each city was measured by the following formula: total inflow intensity during the COVID-19 epidemic in 2020/total inflow intensity during the same period in 2019. (5) COVID-19-related travel factor: existing studies found that people's travel was restricted during the COVID-19 epidemic, which influenced their mental wellbeing (Holmes et al., 2020). Baidu migration and travel big data also provide a travel index within the city during the COVID-19 epidemic in 2020 for each city. We included these data because it measures residents' travel intensity within the city during the COVID-19 epidemic.
2.2.4. Covariates
Following previous studies (Becker et al., 2019; Evandrou et al., 2014), we adjusted for a series of confounding covariates including: (1) demographic and socioeconomic factors: population (10,000 persons), gross domestic product (GDP) per capita (10,000 Chinese Yuan) and unemployment rate; (2) medical resource factors: number of hospital beds (numbers/10,000 persons) and number of doctors (numbers/10,000 persons); and (3) environmental factors: average annual temperature (℃), average annual precipitation (mm) and environment stress index. We used PCA to create an environment stress index based on the volume of industrial waste water discharged (10,000 tons), volume of industrial sulfur dioxide emission (ton), volume of industrial nitrogen dioxide emission (ton) and volume of industrial soot (dust) emission (ton). All of the above data were derived from Statistical Yearbook of Chinese Cities 2019 (National Bureau of Statistics, 2019; China Statistics Press, 2019) and Data Center for Resources and Environmental Sciences, Chinese Academy of Sciences (http://www.resdc.cn/Default.aspx).
Table 1 summarizes the characteristics of the variables. The average suicide index and mental stress index were 0.221 (SD = 0.105) and 0.504 (SD = 0.211), respectively. As for the independent variables, the proportion of parkland area was 0.279 % (SD = 0.812). About 39.527 % of the cities has implemented lockdown policy. Furthermore, the average distance to Wuhan city was 923.508 (SD = 559.076) km, while the average number of COVID-19 infections was 197.459 (SD = 1933.566) cases. The average proportion of migrants from Hubei province was 2.763 % (SD = 10.649). The average work resumption rate was 0.315 (SD = 0.081), and the average travel index within the city was 2.626 (SD = 0.706).
Table 1.
Summary statistics for all variables.
| Dependent variables | Proportion/mean (SD) |
|---|---|
| Suicide index (0−1) | 0.221(0.105) |
| Mental stress index (0−1) | 0.504(0.211) |
| Independent variables | |
| The proportion of parkland area (%) | 0.279(0.812) |
| The presence of lockdown policy (%) | |
| Yes | 39.527 |
| No | 60.473 |
| Distance to Wuhan city (km) | 923.508(559.076) |
| The number of COVID-19 infections (numbers) | 197.459(1933.566) |
| The proportion of migrants from Hubei province (%) | 2.763(10.649) |
| Work resumption rate | 0.315(0.081) |
| Travel (intensity) index within the city | 2.626(0.706) |
| Covariates | |
| Population (10,000 persons) | 441.047(326.177) |
| Number of hospital beds (numbers/10,000 persons) | 45.482(18.688) |
| Number of doctors (numbers/10,000 persons) | 25.139(11.793) |
| GDP per capita (10,000 Chinese Yuan) | 3.837(5.539) |
| Unemployment rate | 0.052(0.033) |
| Environment stress index | 0.175(0.252) |
| Average annual temperature (℃) | 9.628(5.686) |
| Average annual precipitation (mm) | 720.626(491.018) |
In addition, as for the covariates, the average population was 441.047 persons (SD = 326.177). The average number of hospital beds and doctors per 10,000 persons were 45.482 (SD = 18.688) and 25.139 (SD = 11.793), respectively. Also, the average GDP per capita was 3.837 (SD = 5.539) 10,000 Chinese Yuan. The average unemployment rate was 0.052 (SD = 0.033), while environment stress index was 0.175 (SD = 0.252). Last, the average annual temperature and precipitation were 9.628 ℃ (SD = 5.686) and 720.626 mm (SD = 491.018), respectively.
2.2.5. Methods
We initially employed two types of statistical analyses to evaluate the association among parkland, COVID-19 epidemic and mental wellbeing: ordinary least-squares (OLS) regression and two types of spatial regression (spatial lag and spatial error regressions). However, Robust LM (lag) and Robust LM (error) tests indicated that there was no spatial dependence for both the mental stress index [LM (lag): value = 0.001, p-value = 0.922; LM (error): value = 0.156, p-value = 0.689] and suicide index [LM (lag): value = 1.386, p-value = 0.239; LM (error): value = 1.282, p-value = 0.258]; therefore, we only showed the results of OLS. Variance inflation factors (VIF < 3) suggested no severity of multicollinearity among predictors.
First, we regressed the mental stress index (Model 1) and suicide index (Model 2) on parkland, COVID-19 indicators and covariates respectively. Second, interaction terms between parkland and COVID-19 indicators were added to Model 1 to examine whether parkland moderates the relationship between COVID-19 indicators and mental stress index (Model 3–8). Third, interaction terms between parkland and COVID-19 indicators were added to Model 2 to examine whether parkland moderates the relationship between COVID-19 indicators and suicide index (Model 9–14).
3. Results
Table 2 presents the results of the association among parkland, COVID-19 epidemic and mental wellbeing. Model 1 shows that distance to Wuhan city (Coef. = -0.102, SE = 0.026), work resumption rate (Coef. = -0.311, SE = 0.149) and travel index within the city (Coef. = -0.006, SE = 0.003) were negatively associated with mental stress index. Hence, cities with Q2 (Coef. = -0.082, SE = 0.035) and Q3 (Coef. = --0.085, SE = 0.036) proportion of parkland had lower mental stress indexes than those with Q1 proportion of parkland. For covariates, both population (Coef. = -0.001, SE = 0.000) and GDP per capita (Coef. = -0.010, SE = 0.004) were negatively associated with mental stress index.
Table 2.
Association among parkland, COVID-19 epidemic and mental wellbeing.
| Mode l (DV = Mental stress index) |
Model 2 (DV = Suicide index) |
|
|---|---|---|
| Coef. (SE) | Coef. (SE) | |
| Independent variables | ||
| Lockdown (ref: No lockdown) | 0.014 (0.019) | 0.024(0.022) |
| The geographical distance to Wuhan city | −0.102***(0.026) | −0.036***(0.012) |
| The number of COVID-19 infections | 0.010(0.014) | 0.011**(0.005) |
| The proportion of migrants from Hubei province | −0.001(0.002) | 0.003***(0.001) |
| Work resumption rate | −0.311**(0.149) | −0.054(0.102) |
| Travel index within the city | −0.006**(0.003) | −0.014(0.013) |
| The proportion of parkland (ref: Q1) | ||
| Q2 | −0.082**(0.035) | −0.010(0.015) |
| Q3 | −0.085**(0.036) | −0.030*(0.016) |
| Q4 | 0.058(0.045) | −0.057***(0.020) |
| Covariates | ||
| Population | −0.001***(0.000) | 0.001***(0.000) |
| Number of hospital beds | 0.001(0.001) | 0.001(0.001) |
| Number of doctors | 0.004*(0.002) | 0.002**(0.001) |
| GDP per capita | −0.010**(0.004) | −0.004**(0.002) |
| Unemployment rate | 0.127(0.382) | 0.409(0.171) |
| Environment stress index | −0.057(0.053) | 0.036(0.024) |
| Average annual temperature | 0.006(0.005) | 0.002(0.002) |
| Average annual precipitation | 0.000(0.000) | 0.000(0.000) |
| Constant | 1.176***(0.221) | 0.572***(0.098) |
| R2 | 0.274 | 0.445 |
| AIC | −108.427 | −586.18 |
Note: Coef. = coefficient; SE = standard error; AIC = Akaike information criterion. *p < 0.10, **p < 0.05, ***p < 0.01.
Model 2 shows that distance to Wuhan city (Coef. = -0.036, SE = 0.012) was negatively associated with suicide index, while the number of COVID-19 infections (Coef. = 0.011, SE = 0.005) and the proportion of migrants from Hubei province (Coef. = 0.003, SE = 0.001) were positively associated with suicide index. Hence, cities with Q4 (Coef. = -0.057, SE = 0.020) proportion of parkland had lower suicide index than those with Q1 proportion of parkland. For covariates, both population (Coef. = 0.001, SE = 0.000) and number of doctors (Coef. = 0.002, SE = 0.001) were positively associated with suicide index, while GDP per capita was negatively associated with suicide index (Coef. = -0.004, SE = 0.002).
Table 3 presents the moderation effect of parkland on the association between COVID-19 epidemic and mental wellbeing. Model 3–8 shows the interaction term between the proportion of parkland and COVID-19-related indicators for the mental stress index. There was evidence to suggest that the proportion of parkland moderated the association between work resumption rate and mental stress index (Model 7). For instance, compared with cities with Q1 proportion of parkland, the effect of work resumption rate on the mental stress index was strengthened in cities with Q3 proportion of parkland (Coef. = -0.674, SE = 0.333). Additionally, the proportion of parkland moderated the association between the travel index within the city and the mental stress index (Model 8). Specifically, compared with cities with Q1 proportion of parkland, the effect of the travel index within the city on the mental stress index was strengthened in cities with Q3 proportion of parkland (Coef. = -0.099, SE = 0.047). However, no evidence can support the hypothesis that the proportion of parkland also moderates the association between other COVID-19-related indicators and mental parkland (Model 3–6) (Table 4 ).
Table 3.
Buffer effect of parkland on the association between the COVID-19 epidemic and mental wellbeing (DV = Mental stress index).
| Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | |
|---|---|---|---|---|---|---|
| Coef. (SE) | Coef. (SE) | Coef. (SE) | Coef. (SE) | Coef. (SE) | Coef. (SE) | |
| Independent variables | ||||||
| Lockdown (ref: No lockdown) | 0.054(0.060) | 0.021(0.027) | 0.015(0.027) | 0.015(0.027) | 0.012(0.027) | 0.012(0.027) |
| The geographical distance to Wuhan city | −0.104***(0.027) | −0.124***(0.030) | −0.109***(0.027) | −0.099***(0.028) | −0.104***(0.027) | −0.104***(0.027) |
| The number of COVID-19 infections | 0.009(0.014) | 0.011(0.014) | 0.036(0.019) | 0.011(0.014) | 0.010(0.014) | 0.012(0.014) |
| The proportion of migrants from Hubei province | −0.001(0.002) | −0.001(0.002) | −0.001(0.002) | −0.001(0.004) | −0.001(0.002) | −0.001(0.002) |
| Work resumption rate | −0.279**(0.133) | −0.281**(0.139) | −0.229**(0.113) | −0.313**(0.151) | −0.399**(0.189) | −0.305**(0.134) |
| Travel index within the city | −0.010**(0.005) | −0.014**(0.006) | −0.019**(0.009) | −0.016**(0.008) | −0.017**(0.009) | −0.036**(0.018) |
| The proportion of parkland (ref: Q1) | ||||||
| Q2 | −0.085**(0.040) | −0.080**(0.035) | −0.059**(0.027) | −0.084**(0.035) | −0.080**(0.035) | −0.071**(0.036) |
| Q3 | −0.100**(0.043) | −0.080**(0.037) | −0.061**(0.030) | −0.085**(0.037) | −0.082**(0.037) | −0.075**(0.038) |
| Q4 | 0.074(0.052) | 0.066(0.046) | 0.034(0.046) | 0.057(0.045) | 0.055(0.046) | 0.048(0.046) |
| Interaction term | ||||||
| The proportion of parkland (ref: Q1)×Lockdown (ref: No lockdown) | ||||||
| Q2×Lockdown (ref: No lockdown) | −0.026(0.076) | |||||
| Q3×Lockdown (ref: No lockdown) | −0.059(0.076) | |||||
| Q4×Lockdown (ref: No lockdown) | −0.058(0.078) | |||||
| The proportion of parkland (ref: Q1)×The geographical distance to Wuhan city | ||||||
| Q2×The geographical distance to Wuhan city | −0.046(0.040) | |||||
| Q3×The geographical distance to Wuhan city | −0.018(0.051) | |||||
| Q4×The geographical distance to Wuhan city | −0.095*(0.050) | |||||
| The proportion of parkland (ref: Q1)×The number of COVID-19 infections | ||||||
| Q2×The number of COVID-19 infections | −0.042*(0.022) | |||||
| Q3×The number of COVID-19 infections | −0.041(0.027) | |||||
| Q4×The number of COVID-19 infections | −0.032(0.024) | |||||
| The proportion of parkland (ref: Q1)×The proportion of migrants from Hubei province | ||||||
| Q2×The proportion of migrants from Hubei province | −0.001(0.004) | |||||
| Q3×The proportion of migrants from Hubei province | −0.001(0.005) | |||||
| Q4×The proportion of migrants from Hubei province | 0.000(0.004) | |||||
| The proportion of parkland (ref: Q1)×Work resumption rate | ||||||
| Q2×Work resumption rate | −0.087(0.387) | |||||
| Q3×Work resumption rate | −0.674**(0.333) | |||||
| Q4×Work resumption rate | 0.078(0.452) | |||||
| The proportion of parkland (ref: Q1)×Travel index within the city | ||||||
| Q2×Travel index within the city | −0.044(0.046) | |||||
| Q3×Travel index within the city | −0.099**(0.047) | |||||
| Q4×Travel index within the city | 0.041(0.055) | |||||
| R2 | 0.276 | 0.285 | 0.285 | 0.275 | 0.275 | 0.279 |
| AIC | −103.287 | −106.71 | −106.711 | −102.682 | −102.869 | −104.254 |
Note: Models adjusted for all covariates. Coef. = coefficient; SE = standard error; AIC = Akaike information criterion. *p < 0.10, **p < 0.05, ***p < 0.01.
Table 4.
Buffer effect of parkland on the association between the COVID-19 epidemic and mental wellbeing (DV = Suicide index).
| Model 9 | Model 10 | Model 11 | Model 12 | Model 13 | Model 14 | |
|---|---|---|---|---|---|---|
| Coef. (SE) | Coef. (SE) | Coef. (SE) | Coef. (SE) | Coef. (SE) | Coef. (SE) | |
| Independent variables | ||||||
| Lockdown (ref: No lockdown) | 0.016(0.017) | 0.017(0.012) | 0.014(0.012) | 0.014(0.012) | 0.014(0.012) | 0.014(0.012) |
| The geographical distance to Wuhan city | −0.036***(0.012) | −0.039***(0.013) | −0.029**(0.012) | −0.035***(0.013) | −0.035***(0.012) | −0.043***(0.012) |
| The number of COVID-19 infections | −0.011**(0.005) | −0.012**(0.006) | −0.013**(0.007) | −0.011**(0.005) | −0.010**(0.005) | −0.011**(0.005) |
| The proportion of migrants from Hubei province | 0.003***(0.001) | 0.003***(0.001) | 0.003***(0.001) | 0.003**(0.001) | 0.002***(0.001) | 0.002***(0.001) |
| Work resumption rate | −0.055(0.104) | −0.049(0.102) | −0.076(0.104) | −0.054(0.103) | 0.006(0.141) | −0.029(0.103) |
| Travel index within the city | −0.014(0.013) | −0.013(0.013) | −0.011(0.013) | −0.014(0.013) | −0.018(0.013) | −0.033**(0.017) |
| The proportion of parkland (ref: Q1) | ||||||
| Q2 | −0.013(0.018) | −0.006(0.016) | −0.004(0.016) | −0.010(0.016) | −0.011(0.016) | −0.014(0.016) |
| Q3 | −0.031*(0.019) | −0.032**(0.016) | −0.024*(0.014) | −0.031*(0.016) | −0.033**(0.016) | −0.038**(0.017) |
| Q4 | −0.059**(0.023) | −0.057***(0.020) | −0.056***(0.021) | −0.058***(0.020) | −0.062***(0.020) | −0.063**(0.020) |
| Interaction term | ||||||
| The proportion of parkland (ref: Q1)×Lockdown (ref: No lockdown) | ||||||
| Q2×Lockdown (ref: No lockdown) | −0.043(0.034) | |||||
| Q3×Lockdown (ref: No lockdown) | −0.017(0.034) | |||||
| Q4×Lockdown (ref: No lockdown) | −0.068**(0.032) | |||||
| The proportion of parkland (ref: Q1)×The geographical distance to Wuhan city | ||||||
| Q2×The geographical distance to Wuhan city | 0.029(0.018) | |||||
| Q3×The geographical distance to Wuhan city | −0.017(0.023) | |||||
| Q4×The geographical distance to Wuhan city | 0.017(0.022) | |||||
| The proportion of parkland (ref: Q1)×The number of COVID-19 infections | ||||||
| Q2×The number of COVID-19 infections | 0.003(0.010) | |||||
| Q3×The number of COVID-19 infections | −0.005(0.012) | |||||
| Q4×The number of COVID-19 infections | −0.019**(0.009) | |||||
| The proportion of parkland (ref: Q1)×The proportion of migrants from Hubei province | ||||||
| Q2×The proportion of migrants from Hubei province | 0.001(0.002) | |||||
| Q3×The proportion of migrants from Hubei province | −0.001(0.002) | |||||
| Q4×The proportion of migrants from Hubei province | −0.001(0.002) | |||||
| The proportion of parkland (ref: Q1)×Work resumption rate | ||||||
| Q2×Work resumption rate | −0.178(0.172) | |||||
| Q3×Work resumption rate | 0.178(0.192) | |||||
| Q4×Work resumption rate | −0.194(0.200) | |||||
| The proportion of parkland (ref: Q1)×Travel index within the city | ||||||
| Q2×Travel index within the city | −0.004(0.020) | |||||
| Q3×Travel index within the city | −0.052**(0.022) | |||||
| Q4×Travel index within the city | 0.040(0.024) | |||||
| R2 | 0.445 | 0.454 | 0.455 | 0.445 | 0.453 | 0.462 |
| AIC | −580.341 | −585.145 | −585.777 | −580.426 | −584.884 | −589.601 |
Note: Models adjusted for all covariates. Coef. = coefficient; SE = standard error; AIC = Akaike information criterion. *p < 0.10, **p < 0.05, ***p < 0.01.
Model 9–14 shows the interaction term between the proportion of parkland and COVID-19-related indicators for suicide index. There was evidence to suggest that the proportion of parkland moderated the association between the number of COVID-19 infections and the suicide index (Model 11). For example, compared with cities with Q1 proportion of parkland, the effect of the number of COVID-19 infections on the suicide index was reduced in cities with Q4 proportion of parkland (Coef. = -0.019, SE = 0.009). Last, the proportion of parkland moderated the association between the travel index within the city and the suicide index (Model 14). Specifically, compared with cities with Q1 proportion of parkland, the effect of the travel index within the city on the suicide index was strengthened in cities with Q3 proportion of parkland (Coef. = -0.052 SE = 0.022). However, no evidence can support the hypothesis that the proportion of parkland also moderates the association between the rest of the COVID-19-related indicators and the suicide index (Model 10, 12 and 13).
4. Discussion
This study extends previous research on the association between parkland and mental wellbeing (mental stress and suicide intention) in several respects. First, the present study is among the first to systematically explore both direct effect of parkland on mental wellbeing, as well as moderation effect of parkland on the association between the COVID-19 epidemic and mental wellbeing. Second, the study also investigates the extent to which the COVID-19 epidemic has influence on mental wellbeing at a national level.
We found that the provision of parkland is positively associated with mental wellbeing during the COVID-19 epidemic in China. Previous cross-sectional studies in Australia (Wolf and Wohlfart, 2014), Ireland (Grilli et al., 2020) and the UK (Roberts et al., 2019) also found that some of the park attributes and park visits were positively related to mental wellbeing. Similarly, cross-sectional studies from China (Li et al., 2019; Wu et al., 2020), Iran (Yigitcanlar et al., 2020) and Bulgaria (Dzhambov and Dimitrova, 2014) also reported positive associations between urban parkland and the residents' mental wellbeing. In addition to these observational studies, experiments also reported that viewing green spaces within a park can promote peripheral capillary oxygen saturation and reduce blood pressure, which helps people feel relaxed and exert beneficial effects on mental wellbeing (Guan et al., 2017; Hassan et al., 2006; Lin et al., 2019). Although people's use of greenspace may be influenced during epidemic, recent research supports that greenspace such as parkland may still benefit mental health in this period. For example, Biswas and Sen (2020) as well as Kleinschroth and Kowarik (2020) pointed out that greenspaces such as parkland is particularly important for mental health during an epidemic. Slater et al. (2020) suggested that stay-at-home orders may limit access to parks which makes the use of park even more beneficial to mental well-being. Lopez et al. (2020) indicated people continued to use urban parks during the COVID-19, which are considered to be more important for mental health than before the epidemic. Further, Venter et al. (2020) found that people increase recreational use of urban parks and confirm it can provide them with restorative experience during COVID-19 outbreak in Oslo, Norway. Amerio et al. (2020) suggested that better quality of views (i.e more greenery) from people's home are positively associated with mental health during COVID-19 in Milan, Northern Italy. Lu et al. (2020) found an increase of park use during the pandemic in Asian cities. In this study, although people's use of parkland may be influenced during COVID-19, they may still view parkland from their home or in their daily routine, so parkland may provide people with restorative experience, reduce stress and benefit mental health.
In terms of two measurements of mental wellbeing, the mental stress index is more sensitive to the provision of parkland (2nd and 3rd quartile) than the suicide index (only 4th quartile). A possible explanation is that suicidal tendency is a more severe symptom than mental stress tendency, which is less modifiable by provision of healing environment (i.e., parkland) alone. Although most previous studies have confirmed that parkland is beneficial for people's mental wellbeing, it is the first national-level study to confirm that parkland is positively associated with mental wellbeing during the COVID-19 epidemic (Douglas et al., 2020; Kleinschroth and Kowarik, 2020; Lai et al., 2020; Slater et al., 2020; Venter et al., 2020).
We also found most COVID-19-related indicators are significantly associated with mental wellbeing. Our research is based on aggregated data an ecological study design at city level. This approach is consistent with a recent study in China that is based on individual survey data (Shi et al., 2020). First, work resumption rate and travel intensity within the city are positively associated with mental wellbeing. This finding is consistent with a recent study based on individual survey (Shi et al., 2020). Shi et al. (2020) also found that people who resumed work during the COVID-19 epidemic are less likely to report depression or anxiety than those who did not resume work. Resuming work can not only provide people with financial stability but also a distraction from the COVID-19 epidemic. Smart working which means that people work remotely from home (McEwan, 2016) may be an alternative in this period. Some studies indicated it may benefit people's mental health by increasing productivity and work-life balance (Hu, 2020). But others suggested that it may not benefit mental health and lead to income inequity (Bonacini et al., 2020). Furthermore, travel intensity within the city considers all trips for working, shopping, and recreation. Hence it measures the degree to which urban residents return to normal life, which can help people relax themselves and distract them from epidemic-related information (Druss, 2020; Jiménez-Pavón et al., 2020). Second, the number of COVID-19 infections, the proportion of migrants from Hubei Province and the geographical proximity to Wuhan city are negatively associated with mental wellbeing. These factors are all the risk factors related to being infected with COVID-19. Shi et al. (2020) reported that people having family members or friends who were infected with COVID-19, living in Hubei Province and having the chance to come into close contact with patients infected with COVID-19 are more likely to have depression or anxiety.
Most importantly, we found that the provision of parkland reduces the negative effect of COVID-19 on mental wellbeing. First, the proportion of parkland moderates the association between lockdown and mental wellbeing, as well as the association between the number of COVID-19 infections and mental wellbeing. The Stress Reduction Theory (SRT) provides a convincing explanation. According to SRT, natural environments help people recover from the after-effects of stressful experiences (Ulrich et al., 1991). The results from experiments have proved that exposure to natural environments reduces stress-related hormones, which leads to stress recovery (Van den Berg et al., 2015). For example, exposure to nature provides people strong immunization to subsequent stress, and prevents people from being influenced by stressors (Parsons et al., 1998). The Attention Restoration Theory (ART) also explains our findings. ART suggests that natural environments have four types of restorative features, including being away, extension, compatibility and fascination, which can relieve mental fatigue and stress in a person, drawing the individual's effortless attention and reducing attention fatigue symptoms (Kaplan, 2001, 1995).
Further, the proportion of parkland moderates the association between work resumption rate and mental wellbeing, as well as the association between travel intensity within the city and mental wellbeing, which indicates the provision of parkland strengthens the positive effect of restorative behaviors on mental wellbeing. For work resumption rate, the increased proportion of parkland may increase people's exposure to green spaces around workplaces. Previous studies indicated that natural environments around the workplace can help people reduce stress and improve their work efficiency (Dewa et al., 2004; Loder, 2014; Lottrup et al., 2013). Therefore, natural environments can help returning employees reduce pressure and strengthens the positive effect on employment on mental wellbeing. For travel intensity, previous studies suggested that viewing natural environments in people's daily travel routine can help people reduce stress and improve their mental wellbeing (Li et al., 2018; Mennis et al., 2018). Therefore, natural environments can strengthen the restorative effect of travel on mental wellbeing.
The following limitations of this study should be noted. First, this study was based on cross-sectional data, which prevents it from inferring causation between parkland, COVID-19 epidemic and mental wellbeing. Second, the mental wellbeing status was collected from Baidu search data. However, Baidu search data only measure internet users' attention on certain keywords and may not reflect their actual mental wellbeing status. Most internet users are young adults; therefore, our results may be influenced by self-selection bias. Third, our research is based ecological study design, which means data in this study are analysed at population level, rather than individual level. This means that our results may exhibit the ecological fallacy and not be valid for individuals. Future research should measure individuals' mental wellbeing and retest our hypothesis. Fourth, we did not have the information about the usage of parkland by residents, and the proportion of parkland may not reflect the exposure of green spaces or visit to parkland. Fifth, since we measured parkland at city level, the accessibility or distance from parkland was not included. Also, we did not have information regarding people's actual use of greenspace in each city, which may cause bias for the association between parkland and mental health. Sixth, we did not investigate the mechanisms linking parkland to mental health during COVID-19 in this study, so it is still unclear how parkland affect mental health in such a period. Seventh, this study is also limited due to the Modifiable Area Unit Problem (MAUP) because the city boundary was defined by the administrative boundary. Last, we only assessed the effect of parkland from a quantitative perspective (the amout of parkland). However, other perspective of parkland such as the quality of parkland (e.g., biodiversity) also plays an important role in shaping mental wellbeing.
5. Conclusion
This is the first national study which explores both the direct effect of parkland on mental health and the buffering effect of parkland on the association between the COVID-19 epidemic and mental wellbeing. The results show that the provision of parkland is positively associated with mental wellbeing during the COVID-19 epidemic. Among COVID-19-related indicators, distance to Wuhan city, work resumption rate, and travel intensity are positively associated with mental wellbeing, while the number of infections and the proportion of migrants from Hubei Province are negatively associated with it. Last, and most importantly, provision of parkland mitigates the negative effect of COVID-19 epidemic on mental wellbeing. To achieve the goal of promoting mental wellbeing through urban planning and design to combat future pandemics, policymakers and planners are advised to provide more parkland and green spaces and increase their usage while with proper precautions, such as wearing mask and social distancing.
Data availability
Data will be made available on request.
CRediT authorship contribution statement
Ruoyu Wang and Yao Yao conceived the ideas and designed methodology; Ruoyu Wang and Yao Yao collected the data; Ruoyu Wang and Yao Yao analysed the data; Ruoyu Wang led the writing of the manuscript. Yi Lu and Qingfeng Guan reviewed and edited the manuscript. All authors contributed critically to the drafts and gave final approval for publication.
Declaration of Competing Interest
The authors declare that there are no conflicts of interest.
Acknowledgement
The work described in this paper was fully supported by the grants from the National Key Research and Development Program of China (Grant No. 2019YFB2102903), National Natural Science Foundation of China [Project No. 41801306, 41671408, 51778552] and Research Grants Council of the Hong Kong SAR, China [Project No. CityU11207520].
Handling Editor: Wendy Chen
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ufug.2021.127451.
Appendix A. Supplementary data
The following is Supplementary data to this article
References
- Amerio A., Brambilla A., Morganti A., Aguglia A., Bianchi D., Santi F., et al. COVID-19 lockdown: housing built environment’s effects on mental health. Int. J. Environ. Res. Public Health. 2020;17(16):5973. doi: 10.3390/ijerph17165973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker D.A., Browning M.H., Kuo M., Van Den Eeden S.K. Is green land cover associated with less health care spending? Promising findings from county-level Medicare spending in the continental United States. Urban For. Urban Green. 2019;41:39–47. [Google Scholar]
- Biswas R., Sen S. Urban eco-psychological attitude during COVID-19 ‘Lockdown’: a survey. International Journal of Creative Research Thoughts. 2020;8(7) [Google Scholar]
- Bonacini L., Gallo G., Scicchitano S. Working from home and income inequality: risks of a ‘new normal’with COVID-19. J. Popul. Econ. 2020:1–58. doi: 10.1007/s00148-020-00800-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campion J., Javed A., Sartorius N., Marmot M. Addressing the public mental health challenge of COVID-19. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30240-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesare N., Nguyen Q.C., Grant C., Nsoesie E.O. Social media captures demographic and regional physical activity. BMJ Open Sport Exerc. Med. 2019;5 doi: 10.1136/bmjsem-2019-000567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., He G., Chen B., Wang S., Ju G., Ge T. The association between PM2. 5 exposure and suicidal ideation: a prefectural panel study. BMC Public Health. 2020;20:1–10. doi: 10.1186/s12889-020-8409-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- China Statistics Press . China Statistics Press; Beijing: 2019. China Statistical Yearbook of Chinese Cities. [Google Scholar]
- Chong S., Lobb E., Khan R., Abu-Rayya H., Byun R., Jalaludin B. Neighbourhood safety and area deprivation modify the associations between parkland and psychological distress in Sydney. Australia. BMC Public Health. 2013;13:422. doi: 10.1186/1471-2458-13-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimprich B., Ronis D.L. An environmental intervention to restore attention in women with newly diagnosed breast cancer. Cancer Nurs. 2003;26:284–292. doi: 10.1097/00002820-200308000-00005. [DOI] [PubMed] [Google Scholar]
- Cohen D.A., Mckenzie T.L., Sehgal A., Williamson S., Golinelli D., Lurie N. Contribution of public parks to physical activity. Am. J. Public Health. 2007;97:509–514. doi: 10.2105/AJPH.2005.072447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bloom J., Sianoja M., Korpela K., Tuomisto M., Lilja A., Geurts S., Kinnunen U. Effects of park walks and relaxation exercises during lunch breaks on recovery from job stress: two randomized controlled trials. J. Environ. Psychol. 2017;51:14–30. [Google Scholar]
- Dewa C.S., Lesage A., Goering P., Caveen M. Nature and prevalence of mental illness in the workplace. Healthcare Papers. 2004;5:12–25. doi: 10.12927/hcpap..16820. [DOI] [PubMed] [Google Scholar]
- Douglas M., Katikireddi S.V., Taulbut M., McKee M., McCartney G. Mitigating the wider health effects of covid-19 pandemic response. Bmj. 2020:369. doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss B.G. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.0894. [DOI] [PubMed] [Google Scholar]
- Dzhambov A.M., Dimitrova D.D. Elderly visitors of an urban park, health anxiety and individual awareness of nature experiences. Urban For. Urban Green. 2014;13:806–813. [Google Scholar]
- Evandrou M., Falkingham J., Feng Z., Vlachantoni A. Individual and province inequalities in health among older people in China: evidence and policy implications. Health Place. 2014;30:134–144. doi: 10.1016/j.healthplace.2014.08.009. [DOI] [PubMed] [Google Scholar]
- Gidlöf-Gunnarsson A., Öhrström E. Noise and well-being in urban residential environments: the potential role of perceived availability to nearby green areas. Landsc. Urban Plan. 2007;83:115–126. [Google Scholar]
- Gómez E., Baur J.W., Malega R. Dog park users: an examination of perceived social capital and perceived neighborhood social cohesion. J. Urban Aff. 2018;40:349–369. [Google Scholar]
- Grilli G., Mohan G., Curtis J. Public park attributes, park visits, and associated health status. Landsc. Urban Plan. 2020;199 [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O’Connor R.C., Pirkis J., Caine E.D. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan K., Loar R., Anderson B.J., Heptulla R.A. The role of socioeconomic status, depression, quality of life, and glycemic control in type 1 diabetes mellitus. J. Pediatr. 2006;149:526–531. doi: 10.1016/j.jpeds.2006.05.039. [DOI] [PubMed] [Google Scholar]
- Hogg D., Kingham S., Wilson T.M., Ardagh M. The effects of relocation and level of affectedness on mood and anxiety symptom treatments after the 2011 Christchurch earthquake. Soc. Sci. Med. 2016;152:18–26. doi: 10.1016/j.socscimed.2016.01.025. [DOI] [PubMed] [Google Scholar]
- Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Silver R.C., Everall I. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong Y.R., Lawrence J., Williams D., Jr., Mainous Iii A. Population-level interest and telehealth capacity of US hospitals in response to COVID-19: cross-sectional analysis of Google search and national hospital survey data. JMIR Public Health Surveill. 2020;6(2) doi: 10.2196/18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu R. COVID-19, smart work, and collaborative space: a crisis-opportunity perspective. J. Urban Manag. 2020 [Google Scholar]
- Husnayain A., Fuad A., Su E.C.Y. Applications of google search trends for risk communication in infectious disease management: a case study of COVID-19 outbreak in Taiwan. Int. J. Infect. Dis. 2020;95:221–223. doi: 10.1016/j.ijid.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalloh M.F., Li W., Bunnell R.E., Ethier K.A., O’Leary A., Hageman K.M., Sengeh P., Jalloh M.B., Morgan O., Hersey S. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob. Health. 2018;3 doi: 10.1136/bmjgh-2017-000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings V., Bamkole O. The relationship between social cohesion and urban green space: an avenue for health promotion. Int. J. Environ. Res. Public Health. 2019;16:452. doi: 10.3390/ijerph16030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiménez-Pavón D., Carbonell-Baeza A., Lavie C.J. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people. Prog. Cardiovasc. Dis. 2020 doi: 10.1016/j.pcad.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaczynski A.T., Potwarka L.R., Saelens B.E. Association of park size, distance, and features with physical activity in neighborhood parks. Am. J. Public Health. 2008;98:1451–1456. doi: 10.2105/AJPH.2007.129064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan S. The restorative benefits of nature: toward an integrative framework. J. Environ. Psychol. 1995;15:169–182. [Google Scholar]
- Kaplan R. The nature of the view from home: psychological benefits. Environ. Behav. 2001;33:507–542. [Google Scholar]
- Kleinschroth F., Kowarik I. COVID‐19 crisis demonstrates the urgent need for urban greenspaces. Front. Ecol. Environ. 2020;18(6):318. doi: 10.1002/fee.2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluger N., Scrivener Y. The use of Google trends for acral symptoms during COVID‐19 outbreak in France. J. Eur. Acad. Dermatol. Venereol. 2020;34:e358–e360. doi: 10.1111/jdv.16572. [DOI] [PubMed] [Google Scholar]
- Lai K.Y., Webster C., Kumari S., Sarkar C. The nature of cities and the COVID-19 pandemic. Curr. Opin. Environ. Sustain. 2020 doi: 10.1016/j.cosust.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D., Deal B., Zhou X., Slavenas M., Sullivan W.C. Moving beyond the neighborhood: daily exposure to nature and adolescents’ mood. Landsc. Urban Plan. 2018;173:33–43. [Google Scholar]
- Li D., Zhai Y., Xiao Y., Newman G., Wang D. Subtypes of park use and self-reported psychological benefits among older adults: a multilevel latent class analysis approach. Landsc. Urban Plan. 2019;190 doi: 10.1016/j.landurbplan.2019.103605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F., Li F., Li S., Long Y. Deciphering the recreational use of urban parks: experiments using multi-source big data for all Chinese cities. Sci. Total Environ. 2020;701 doi: 10.1016/j.scitotenv.2019.134896. [DOI] [PubMed] [Google Scholar]
- Lin W., Chen Q., Jiang M., Zhang X., Liu Z., Tao J., Wu L., Xu S., Kang Y., Zeng Q. The effect of green space behaviour and per capita area in small urban green spaces on psychophysiological responses. Landsc. Urban Plan. 2019;192 [Google Scholar]
- Lin Y.H., Liu C.H., Chiu Y.C. Google searches for the keywords of “wash hands” predict the speed of national spread of COVID-19 outbreak among 21 countries. Brain Behav. Immun. 2020;87:30–32. doi: 10.1016/j.bbi.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loder A. ‘There’s a meadow outside my workplace’: a phenomenological exploration of aesthetics and green roofs in Chicago and Toronto. Landsc. Urban Plan. 2014;126:94–106. [Google Scholar]
- Lopez B., Kennedy C., McPhearson T. Parks are Critical Urban Infrastructure: Perception and Use of Urban Green Spaces in NYC During COVID-19. Preprints. 2020 [Google Scholar]
- Lottrup L., Grahn P., Stigsdotter U.K. Workplace greenery and perceived level of stress: benefits of access to a green outdoor environment at the workplace. Landsc. Urban Plan. 2013;110:5–11. [Google Scholar]
- Lu Y., Zhao J., Wu X., Lo S.M. Escaping to nature in pandemic: a natural experiment of COVID-19 in Asian cities. Center for Open Science. 2020 [Google Scholar]
- Markevych I., Schoierer J., Hartig T., Chudnovsky A., Hystad P., Dzhambov A.M., et al. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ. Res. 2017;158:301–317. doi: 10.1016/j.envres.2017.06.028. [DOI] [PubMed] [Google Scholar]
- Marselle M.R., Warber S.L., Irvine K.N. Growing resilience through interaction with nature: Can group walks in nature buffer the effects of stressful life events on mental health? Int. J. Environ. Res. Public Health. 2019;16:986. doi: 10.3390/ijerph16060986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwan A.M. CRC Press; 2016. Smart Working: Creating the Next Wave. [Google Scholar]
- Mennis J., Mason M., Ambrus A. Urban greenspace is associated with reduced psychological stress among adolescents: a Geographic Ecological Momentary Assessment (GEMA) analysis of activity space. Landsc. Urban Plan. 2018;174:1–9. doi: 10.1016/j.landurbplan.2018.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munro A., Kovats R.S., Rubin G.J., Waite T.D., Bone A., Armstrong B., Beck C.R., Amlôt R., Leonardi G., Oliver I. Effect of evacuation and displacement on the association between flooding and mental health outcomes: a cross-sectional analysis of UK survey data. Lancet Planet. Health. 2017;1:e134–e141. doi: 10.1016/S2542-5196(17)30047-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bureau of Statistics . China Statistics Press; Beijing: 2019. . China Statistical Yearbook of Chinese Cities. [Google Scholar]
- National Health Commission of the People’s Republic of China . 2020. Covid-19 Prevention and Control Plan (Fifth Edition)http://www.nhc.gov.cn/jkj/s3577/202002/a5d6f7b8c48c451c87dba14889b30147/files/3514cb996ae24e2faf65953b4ecd0df4.pdf Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordh H., Alalouch C., Hartig T. Assessing restorative components of small urban parks using conjoint methodology. Urban For. Urban Green. 2011;10(2):95–103. [Google Scholar]
- Ojala A., Korpela K., Tyrväinen L., Tiittanen P., Lanki T. Restorative effects of urban green environments and the role of urban-nature orientedness and noise sensitivity: a field experiment. Health Place. 2019;55:59–70. doi: 10.1016/j.healthplace.2018.11.004. [DOI] [PubMed] [Google Scholar]
- Orsega-Smith E., Mowen A.J., Payne L.L., Godbey G. The interaction of stress and park use on psycho-physiological health in older adults. J. Leis. Res. 2004;36:232–256. [Google Scholar]
- Ottosson J., Grahn P. The role of natural settings in crisis rehabilitation: how does the level of crisis influence the response to experiences of nature with regard to measures of rehabilitation? Landsc. Res. 2008;33:51–70. [Google Scholar]
- Page L.A., Seetharaman S., Suhail I., Wessely S., Pereira J., Rubin G.J. Using electronic patient records to assess the impact of swine flu (influenza H1N1) on mental health patients. J. Ment. Health. 2011;20:60–69. doi: 10.3109/09638237.2010.542787. [DOI] [PubMed] [Google Scholar]
- Parsons R., Tassinary L.G., Ulrich R.S., Hebl M.R., Grossman-Alexander M. The view from the road: implications for stress recovery and immunization. J. Environ. Psychol. 1998;18:113–140. [Google Scholar]
- Payne S.R. Are perceived soundscapes within urban parks restorative. J. Acoust. Soc. Am. 2008;123(5) 3809-3809. [Google Scholar]
- Peters K., Elands B., Buijs A. Social interactions in urban parks: stimulating social cohesion? Urban For. Urban Green. 2010;9:93–100. [Google Scholar]
- Pfefferbaum B., Schonfeld D., Flynn B.W., Norwood A.E., Dodgen D., Kaul R.E., Donato D., Stone B., Brown L.M., Reissman D.B. The H1N1 crisis: a case study of the integration of mental and behavioral health in public health crises. Disaster Med. Public Health Prep. 2012;6:67–71. doi: 10.1001/dmp.2012.2. [DOI] [PubMed] [Google Scholar]
- Roberts H., Kellar I., Conner M., Gidlow C., Kelly B., Nieuwenhuijsen M., McEachan R. Associations between park features, park satisfaction and park use in a multi-ethnic deprived urban area. Urban For. Urban Green. 2019;46 [Google Scholar]
- Shi L., Lu Z.-A., Que J.-Y., Huang X.-L., Liu L., Ran M.-S., Gong Y.-M., Yuan K., Yan W., Sun Y.-K. Prevalence of and Risk Factors Associated With Mental Health Symptoms Among the General Population in China During the Coronavirus Disease 2019 Pandemic. JAMA network open. 2020;3 doi: 10.1001/jamanetworkopen.2020.14053. e2014053-e2014053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shultz J.M., Baingana F., Neria Y. The 2014 Ebola outbreak and mental health: current status and recommended response. Jama. 2015;313:567–568. doi: 10.1001/jama.2014.17934. [DOI] [PubMed] [Google Scholar]
- Slater S.J., Christiana R.W., Gustat J. Recommendations for Keeping Parks and Green Space Accessible for Mental and Physical Health During COVID-19 and Other Pandemics. Prev. Chronic Dis. 2020:17. doi: 10.5888/pcd17.200204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su J.G., Jerrett M., de Nazelle A., Wolch J. Does exposure to air pollution in urban parks have socioeconomic, racial or ethnic gradients? Environ. Res. 2011;111:319–328. doi: 10.1016/j.envres.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Tausczik Y., Faasse K., Pennebaker J.W., Petrie K.J. Public anxiety and information seeking following the H1N1 outbreak: blogs, newspaper articles, and Wikipedia visits. Health Commun. 2012;27:179–185. doi: 10.1080/10410236.2011.571759. [DOI] [PubMed] [Google Scholar]
- Thomas S.P. Ebola and mental health. Issues Ment. Health Nurs. 2015;36:247–248. doi: 10.3109/01612840.2015.1023616. [DOI] [PubMed] [Google Scholar]
- Thompson Coon J., Boddy K., Stein K., Whear R., Barton J., Depledge M.H. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ. Sci. Technol. 2011;45:1761–1772. doi: 10.1021/es102947t. [DOI] [PubMed] [Google Scholar]
- Tsuboya T., Aida J., Hikichi H., Subramanian S., Kondo K., Osaka K., Kawachi I. Predictors of depressive symptoms following the Great East Japan earthquake: a prospective study. Soc. Sci. Med. 2016;161:47–54. doi: 10.1016/j.socscimed.2016.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulrich R.S., Simons R.F., Losito B.D., Fiorito E., Miles M.A., Zelson M. Stress recovery during exposure to natural and urban environments 1. J. Environ. Psychol. 1991;11:201–230. [Google Scholar]
- Van den Berg M.M., Maas J., Muller R., Braun A., Kaandorp W., Van Lien R., Van Poppel M.N., Van Mechelen W., Van den Berg A.E. Autonomic nervous system responses to viewing green and built settings: differentiating between sympathetic and parasympathetic activity. Int. J. Environ. Res. Public Health. 2015;12:15860–15874. doi: 10.3390/ijerph121215026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Den Berg A.E., Maas J., Verheij R.A., Groenewegen P.P. Green space as a buffer between stressful life events and health. Soc. Sci. Med. 2010;70:1203–1210. doi: 10.1016/j.socscimed.2010.01.002. [DOI] [PubMed] [Google Scholar]
- van den Bosch M., Sang Å.O. Urban natural environments as nature-based solutions for improved public health–a systematic review of reviews. Environ. Res. 2017;158:373–384. doi: 10.1016/j.envres.2017.05.040. [DOI] [PubMed] [Google Scholar]
- Veitch J., Flowers E., Ball K., Deforche B., Timperio A. Designing parks for older adults: a qualitative study using walk-along interviews. Urban For. Urban Green. 2020 [Google Scholar]
- Venter Z., Barton D., Gundersen V., Figari H., Nowell M. Urban nature in a time of crisis: recreational use of green space increases during the COVID-19 outbreak in Oslo. Norway. Environmental Research Letters. 2020 [Google Scholar]
- Vieira J., Matos P., Mexia T., Silva P., Lopes N., Freitas C., Correia O., Santos-Reis M., Branquinho C., Pinho P. Green spaces are not all the same for the provision of air purification and climate regulation services: the case of urban parks. Environ. Res. 2018;160:306–313. doi: 10.1016/j.envres.2017.10.006. [DOI] [PubMed] [Google Scholar]
- Vos T., Allen C., Arora M., Barber R.M., Bhutta Z.A., Brown A., Carter A., Casey D.C., Charlson F.J., Chen A.Z. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker A., Hopkins C., Surda P. The use of google trends to investigate the loss of smell related searches during COVID‐19 outbreak. Int. Forum Allergy Rhinol. 2020;10:839–847. doi: 10.1002/alr.22580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan C., Shen G.Q., Choi S. Effects of physical and psychological factors on users’ attitudes, use patterns, and perceived benefits toward urban parks. Urban For. Urban Green. 2020 [Google Scholar]
- Wang R., Lu Y., Wu X., Liu Y., Yao Y. Relationship between eye-level greenness and cycling frequency around metro stations in Shenzhen, China: A big data approach. Sustain. Cities Soc. 2020;59:102201. [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang R., Feng Z., Pearce J., Liu Y., Dong G. Are greenspace quantity and quality associated with mental health through different mechanisms in Guangzhou, China: A comparison study using street view data. Environ. Pollut. 2021;290 doi: 10.1016/j.envpol.2021.117976. [DOI] [PubMed] [Google Scholar]
- Wang R., Feng Z., Pearce J., Zhou S., Zhang L., Liu Y. Dynamic greenspace exposure and residents’ mental health in Guangzhou, China: from over-head to eye-level perspective, from quantity to quality. Landsc. Urban Plan. 2021;215 [Google Scholar]
- Wells N.M., Evans G.W. Nearby nature: a buffer of life stress among rural children. Environ. Behav. 2003;35:311–330. [Google Scholar]
- Wolf I.D., Wohlfart T. Walking, hiking and running in parks: a multidisciplinary assessment of health and well-being benefits. Landsc. Urban Plan. 2014;130:89–103. [Google Scholar]
- World Health Organization. Coronavirus disease (COVID-19) pandemic. Accessed June 3, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- Wu W., Dong G., Yeran S., Yun Y. Contextualized effects of Park access and usage on residential satisfaction: a spatial approach. Land Use Policy. 2020;94 [Google Scholar]
- Xie B., Lu Y., Wu L., An Z. Dose-response effect of a large-scale greenway intervention on physical activities: The first natural experimental study in China. Health and Place. 2021;67 doi: 10.1016/j.healthplace.2020.102502. [DOI] [PubMed] [Google Scholar]
- Yadav S., Rawal G. The current mental health status of Ebola survivors in Western Africa. Journal of clinical and diagnostic research: JCDR. 2015;9 doi: 10.7860/JCDR/2015/15127.6559. LA01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yigitcanlar T., Kamruzzaman M., Teimouri R., Degirmenci K., Alanjagh F. Association between park visits and mental health in a developing country context: the case of Tabriz. Iran. Landscape And Urban Planning. 2020;199 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.