Abstract
It is inevitable that some patients with suspected or confirmed COVID-19 may require urgent surgical procedures. The objective of this review was to discuss the modifications required in the operating room during COVID-19 times for minimal access, laparoscopy, and robotic surgery, especially with regard to minimally invasive surgical instruments, buffalo filter, trocars with smoke evacuator, and special personal protection equipment. We have discussed the safety measures to be followed for the suspected or confirmed COVID-19 patient. In addition to surgical patients, health care workers should also protect themselves by following the guidelines and recommendations while treating these patients. Although there is little evidence of viral transmission through laparoscopic or open approaches, we recommend modifications to surgical practice such as the use of safe smoke evacuation and minimizing energy device use to reduce the risk of exposure to aerosolized particles to the health care team. Therefore, hospitals must follow specific protocols and arrange suitable training of the health care workers. Following well-established plans to accomplish un-deferrable surgeries in COVID-19–positive patients is strongly recommended.
Keywords: COVID-19, SARS-CoV-2, minimally invasive surgery, personal protection equipments
Introduction
Cancer is a disease with high mortality rates. The incidence in India is >100 000 new cases per month. Due to high mortality rates and time-sensitive nature of the treatment, delaying therapy is not advisable as many patients may lose their lives early.1 Corona virus disease 2019 (COVID-19 or SARS-CoV-2) virus is a ribonucleic acid (RNA) virus belonging to the family Corona virus. COVID-19 affects the respiratory tract. This epidemic began in December 2019 in Wuhan, China, and spread rapidly throughout the World and is now a pandemic within 3-4 months. COVID-19 has shown a tendency to spread at an exponential rate, with a significant impact on lives of individuals and the practice of health care professionals.
There are high chances of morbidity (40%) and mortality (20%) in patients after elective surgery in the face of COVID-19 infection post-surgery. Also, the chance of spread of infection to surgeons and other health workers is high while operating on a patient of COVID-19 infection.1 COVID-19 can infect anyone and is contagious prior to the onset of symptoms or even without developing symptoms. Therefore, aggressive testing or screening of asymptomatic patients’ needs to be done.2 There are 2 types of COVID-19 tests: RNA tests and the serological antibody tests.3
COVID-19 virus is not usually present in blood. In COVID-19 infection, patients generally seroconvert after 7-11 days of exposure, although a few patients may develop antibodies earlier. Therefore, antibody testing may not be beneficial in the setting of an acute infection.2 Further, it is also not clear whether individuals who recovered from COVID-19 will be protected, either fully or partially, from reinfection in future.3 Testing for COVID-19 with combined immunoglobulin M (IgM) and IgG antibodies test is an effective method for the rapid diagnosis, where IgM antibodies indicate a recent infection and IgG antibodies indicate a later stage of infection.4 The results of COVID-19 antibody test must be complemented by other tests such as reverse transcription–polymerase chain reaction/enzyme-linked immunosorbent assay tests and possibly Computed Topography scanning of the thorax in appropriate situations.5-7
COVID-19 is spreading like wildfire due to its highly contagious nature. Currently, most hospitals have stopped elective surgeries. This decision has been taken due to a high chance of COVID-19 infection to the health care workers involved in elective surgery. Further, it is not clear when the curve of the COVID-19 pandemic will flatten. Although extremely challenging, it is vital that hospitals can perform surgeries for patients with urgent needs even if the pandemic continues.8 In such a pandemic-like situation, patients requiring urgent surgery should always be assumed to be possible carriers of COVID-19, even if they are afebrile, and have no history of exposure or travel and no respiratory symptoms.3 Maintaining the balance between preventing the spread of COVID-19 and cancer treatment is challenging. Moreover, in India, due to the fear of community spread of COVID-19, it is necessary to have uniformity in guidelines to pave the way forward for cancer surgery.
Hence, it is necessary to discuss special precautions to be taken by surgeons and other health care professionals involved in cancer surgery. In this pandemic, some safety measures are discussed, which will not only help in supporting the health care professionals but also address a number of doubts regarding patient safety and care during surgical practice.
In this review, in addition to literature related to the COVID-19 pandemic, recommendations from different guidelines such as Indian Association of Surgical Oncology (IASO),1 Association of Minimal Access Surgeons of India (AMASI),5 Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and European Association of Endoscopic Surgery,9 EAU Robotic Urology Section (ERUS),10 Association of PeriOperative Registered Nurses (AORN),11 and Inter Association Surgical Practice Recommendations (AMASI, Indian Association Of Gastrointestinal Endosurgeons, and Society Of Endoscopic and Laparoscopic Surgeons of India)7 guidelines have also been discussed. The present review is focused on the following objective:
What modifications should the surgeon do in the operation theater (OT) during COVID-19 times for minimal access, and laparoscopic and robotic surgery, with special emphasis on minimally invasive surgical (MIS) instruments, buffalo filter, trocars with smoke evacuator, and special personal protection equipment (PPE) for performing MIS and endoscopy.
Literature Review and Guideline Recommendations
OT Modifications
The chances of COVID-19 infection to staff during surgery (open, laparoscopic, or robotic) are high. It is advised to reduce the risk of COVID-19 infection to surgical staff in the OT room. Therefore, protective methods should be strictly employed.9
In COVID-19–positive/suspected cases, surgeries should be performed in a dedicated OT.10,12 OT rooms should be preferably situated on 1 side of the hospital complex.13 In negative cases also, general recommendations to reduce COVID-19 transmission need to be followed.10,12 OT rooms for suspected or confirmed COVID-19 patients should be adequately filtered and ventilated with an integrated high-efficiency particulate air (HEPA) filter. Negative pressure rooms should be considered to decrease the contamination of the neighboring OT.7,9 A high frequency of air changes (>25 cycles per hour) speedily reduces the viral load in the OT room. No unnecessary movement should be allowed inside the OT room.13
Intubation and extubation should take place in a negative pressure room.14,15 Video laryngoscope (VL) is advised for intubation. The use of viral filter in the breathing circuit (intersurgical or thermovent HEPA) or heat and moisture exchanger (HME) filter is advised. These filters should be attached to the endotracheal tube (ETT), but before that, intubation filter to the expiratory end of circuit should also be installed. Positive pressure ventilation should be avoided if possible. Extubation should follow the same precautions as intubation.5
Surgical equipment used for COVID-19–positive or suspected COVID-19 patients should be cleaned separately from other surgical equipment. All reusable contaminated material should be sterilized immediately.5,7 The monitor and cables of the VL should be cleaned with an alcohol-based sanitizer and kept in a UV chamber, while the blade should undergo ethylene oxide or plasma sterilization.5,9
Endoscopic procedures requiring additional insufflation of carbon dioxide (CO2) or room air should be avoided. Removal of caps on endoscopes should be avoided due to chances of release of fluid or air.9 Suction devices should be used to evacuate the smoke from the abdomen.5 Electronic gadgets such as pagers, laptop, or mobile, and hospital case sheets should be left outside the OT rooms. Disposable pens should be used.13 Surgical aids such as OT trolley, laparoscopy trolley, anesthesia trolley, and gas cylinders should be kept inside the OT to avoid the increase in OT time. The patients should be brought inside the OT room once all preparations are done. All other requisites such as drugs, sutures, and emergency equipment should be present in the OT room prior to the start of surgery.5
All MIS should be performed by experienced surgeons.12 Surgeries should be performed with the minimum number of OT staff. Surgical training fellowships should be temporarily suspended.10 Only the anesthesia team should remain in the OT during intubation and extubation. OT should be cleaned and sterilized post-surgery.5 Disposable materials only (such as gloves or paper towel) should be used for cleaning. Containers should be closed and sealed before transferring to the collection unit.16 There should be a gap of minimum of 1 hour between 2 surgical procedures.5,7
Laparoscopic Trocar–Cannula Modifications
Use of appropriate trocars helps to avoid surgical accidents which can cause serious and fatal injuries. The chance of laparoscopic instruments transmitting fomites and cross-infection to staff and other patients is high. Incisions for ports should be appropriate to permit the passage of ports while preventing leakage around ports.5,7,9 Once placed, ports should not be used for evacuation of smoke or for desufflation without taking adequate precautions.7 Sudden bursts of release of pneumoperitoneum from trocar valves during exchange of instruments or during the venting of trocars may allow for the transmission of COVID-19. Hence instrument exchanges should be minimized. Further, traditional trocars may be better, with 1-way valves within the proximal portion of the port. In robotic surgery, the leakage should be avoided from trocars when inserting 8-mm or 5-mm instruments through the 12-mm trocars. Also, the use of 5-mm instruments through even the 8-mm trocars should perhaps be minimized.17
CO2 insufflation pressure should be maintained at a minimum, and an ultrafiltration system (smoke evacuation system or filtration) should be used. All pneumoperitoneum should be safely evacuated via a filtration system before closure, trocar removal, specimen extraction, or conversion to open.9
The IASO recommends that in the green zones (if no COVID-19 case seen for the last 24 days), surgeons should begin treating curable cancers with due care while in orange/white zones, and surgeries need to start carefully. In the red zone (more than 6 active cases, or if cases double in less than a week), previous guidelines should be followed with extreme care. Surgeries, if undertaken, must be simple and short and with low morbidity and minimal blood loss.1
Smoke Evacuators
Reliable information related to the safety of smoke evacuation in laparoscopic procedures and whether COVID-19 could be aerosolized during such procedures is not available at present. However, the risk of viral exposure during endoscopy and airway procedures is high.18,19 Ultrasonic scalpels or diathermy equipment used in MIS can produce huge amounts of surgical smoke, and the low temperature aerosol from ultrasonic scalpels or scissors cannot effectively deactivate the cellular components of virus in patients.19 Various studies have shown Corynebacterium, papillomavirus, and human immunodeficiency virus to be detected in surgical smoke.20-22 Hepatitis B virus (HBV) has been present in surgical smoke in 10 of 11 HBV-affected patients.23 Therefore, it is likely that the COVID-19 virus can spread during aerosol generating procedures and possibly infect the surgical staff.18 Several surgeons have contracted a rare papillomavirus suspected to be connected to surgical smoke exposure.24 Thus, the risk of COVID-19 infection via aerosol should not be any exception.10 SARS-Cov-2 has aerosol and fomite transmission potential comparable to SARS-Cov-1, and it can remain in aerosols for 3 hours or more, and on various surfaces for up to 72 hours.25,26 Therefore, effective measures should be followed for the evacuation of smoke in surgery of patients suspected of COVID-19.
Low-temperature aerosol from ultrasonic scalpels cannot effectively deactivate the cellular components of the COVID-19. Due to previous reports of aerosolization of other viruses,27,28 COVID-19 infection should also be tackled during MIS procedures by the use of devices to filter released CO2 for aerosolized particles.9 Standard electrostatic filters (HME filters) used in ventilation machines can filter bacterial and viral loads with great efficacy.26 These filters may provide >99% protection against hepatitis C virus and HBV having a diameter of >30 nm.18 HEPA can remove up to 99.97% of contaminants (≥.3 microns in diameter) and ultralow particulate (ULPA) air filters up to 99.99% (≥.12 microns).29 COVID-19 is reported to have a diameter of 60–90 nm.10,30 It should be kept in mind that COVID-19 can be transmitted by droplets, contact, aerosol, and fecal–oral route. Viral contamination can also occur from aerosol formation.
Laparoscopic surgery can be done, but gases must be managed well (i.e., with use of filtering aids such as CO2 filter).31 Standard electrostatic filters can be expected to efficiently protect from the COVID-19 virus. These filters should be connected via standard tubing to the trocar evacuation port which can be used to evacuate the produced smoke and filter the possible viral load.18 If a reliable filtering and evacuation system for gases is used, laparoscopy is preferable to open surgery, where smoke contamination is intense. Regular cleaning of instruments, evacuating pneumoperitoneum prior to removing trocars, and conversion or specimen extraction are particularly helpful.19 The use of intelligent, integrated flow systems is recommended for the maintenance of low intra-abdominal pressure which ensures a self-maintained constant pneumoperitoneum.5,10,11 Two-way pneumoperitoneum insufflators should be avoided so that pathogen colonization of circulating aerosol in the pneumoperitoneum circuit or the insufflator can be prevented. The integrated flow systems should be configured in a continuous smoke evacuation and filtration mode, preferably through a ULPA filter.10,11
Complete desufflation of the pneumoperitoneum at the end of the surgical procedure should be ensured. Due to the enclosed gas in the pneumoperitoneum, aerosol formed during the surgery may get concentrated in the abdominal cavity.19 Rapid release of trocar valves, non-airtight exchange of instruments, or even small abdominal extraction incisions can possibly expose the health care team to the intra-abdominal aerosol. Therefore, systems with integrated, active smoke evacuation modes are advised.9 Conversely, traditional insufflation systems that are not equipped with active smoke evacuation mode or other filters may expose health care personnel to higher risk of COVID-19 aerosol transmission.10
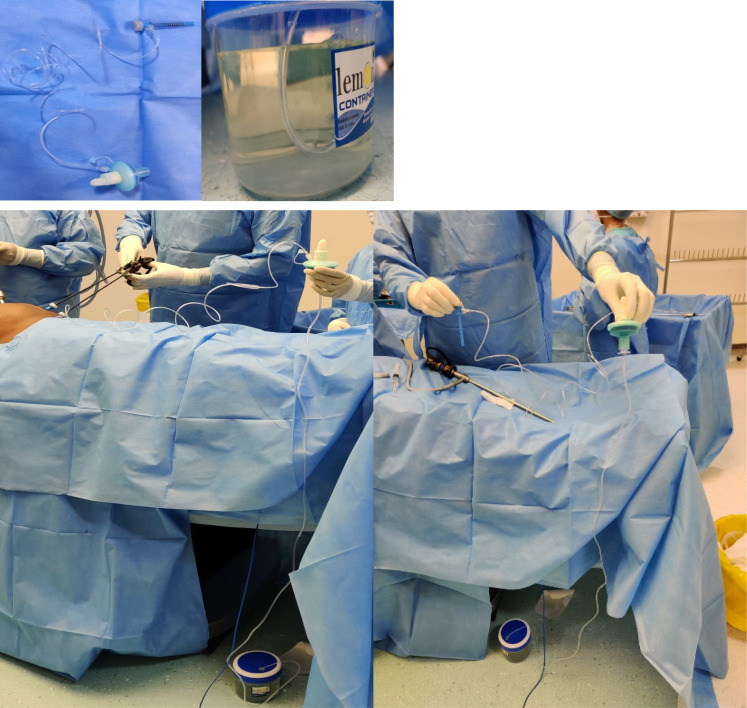
At Manipal Hospital, we have used an indigenous circuit devised from an HME filter (with or without HEPA filter) and an underwater seal using sodium hypochlorite solution for safe evacuation of pneumoperitoneum during COVID-19 response time (Figure 1). This system is simple, disposable, quick to assemble, and efficient for smoke evacuation during laparoscopic procedures.
Figure 1.
HME filter with or without HEPA filter and under water seal sodium hypochlorite. Indian, Manipal modification for lap evacuator under seal sodium hypochlorite during COVID-19 response time.
Note. HEPA = high-efficiency particulate air; HME = heat and moisture exchanger.
Setup: A dedicated 5-mm port is used for evacuation of the gas/surgical smoke continuously which is first connected to an intravenous drip set. The other end of the drip set is connected to the HME filter through which the gas enters the filter. The other end of the HME filter is fitted with a 3/3.5 ETT proximal tube which is turn connected to the drip set. The other end of the drip set is then finally let immersed into a jar containing 1% sodium hypochlorite solution which is nearly 50% filled. Surgical smoke or gas continuously flows through the drip set through the HME filter, and then enters the jar containing hypochlorite solution.
Buffalo Filters
Buffalo filter offers a wide line of filters and prefilters to fit the surgical procedure requirements. Buffalo filter has 4 stages of filtration that ensure 99.999% efficiency for .1-.2 microns, and HME filters provide bacterial and viral filtration above 99.9%. Buffalo filter smoke evacuator tubing is connected to 2 HME filters and placed under the drape to provide air filtration. The use of multifilter system ensures maximum efficiency in filtering viral particles.32
Anesthesia Modifications
By minimizing the aerosol-generating processes during general anesthesia, anesthesiologists may reduce exposure to patient’s respiratory secretions and the risk of perioperative viral transmission to health care personnel and patients.33 Intubation during general anesthesia may result in general aerosolization causing risk to anesthesia team as well as the OT personnel. Hence, preference should be given to regional anesthesia (open surgery) during surgical procedures.7,34 Regional anesthesia offers benefits of preservation of respiratory function, avoidance of aerosolization and hence viral transmission.33
Laminar airflow or air conditioner should be started after induction of anesthesia. Laminar airflow or air conditioner should be stopped 20 minute before the extubation.7 Anesthesia monitor should be covered with a plastic wrap. After the surgery, the anesthetic breathing circuit and the container of soda lime should be discarded immediately.13
Neuraxial anesthesia may cause the risk of seeding infection into the central nervous system (CNS) in infected patients. Therefore, its use should be balanced against the risk of performing general anesthesia on patients with COVID-19. It is advised to minimize the airborne contamination, by keeping in mind the possibility of converting to general anesthesia if regional anesthesia fails. A pencil-point spinal needle is helpful for spinal anesthesia as it may reduce the risk of transmission viral material into the CNS. There is less tissue coring in comparison to cutting tip spinal needles.34 VL is advised for intubation.
Personal Protection of Surgeons
All elective surgical and endoscopic cases should be postponed at the current time. For patients requiring urgent medical needs decisions should be made locally. In COVID-19 positive patients, the procedure should be postponed if not emergent.5,7,10 This will reduce the risk to surgeons, and also reduce the use of scarce resources (such as ventilators, intensive care unit [ICU] beds and personal protective equipment [PPE]) while also reducing morbidity and mortality.9 Patients scheduled for surgery should always be assumed to be potential carriers of the COVID-19, even if they pass the pre-operative risk-assessment (ie normal temperature, no exposure or travel history and no respiratory signs).3
Surgeons must avoid contact with droplets and use full body protection. Universal protection with PPE (appropriate gowns, N95/FFP2-3 masks and face shields/goggles) is strongly recommended for surgeons and other OT personnel.1,5,10 Donning of PPE should be done in the OT room and doffing should be done in wash area. OT foot-wear should be washed with soap and water immediately after the surgery.5 The ability to completely and effectively control aerosolization of virus during endoscopic procedures is lacking, therefore regular hand-wash, sanitizers and PPE use should be strictly followed. Multidisciplinary team (MDT) meetings should be virtual and restricted to core team members only. Only essential personnel should participate in the surgery and the size of surgical team should be reduced as much as possible.7,9 No one except the necessary staff should be allowed inside OT during intubation and extubation. Senior oncologists (age >60 years) and those with co-morbidities should abstain from surgery during the COVID-19 pandemic, especially if there are substitutes available. Special care should be taken by the anesthetists, surgeons and endoscopists.1
It is reported that COVID-19 is present in the stools of COVID-19 patients, but its transmission during laparoscopic procedures is not known. Also, fecal-oral transmission has not been reported though it may be possible.12,35 Therefore, it is better to minimize bowel handling and opening during surgical procedures to reduce the risk virus dissemination with CO2.10 Although no evidence of COVID-19 transmission through the urine is demonstrated,36 but urethral or ureteral catheterization during the laparoscopic and robotic procedures should be performed with caution, particularly if pneumoperitoneum is already induced.10
After the surgery, the surgical team should discard used gowns and gloves in the OT room and should renew hand hygiene before leaving the room. The removed PPE should be carefully discarded. All PPE should be removed outside the OT room. All surfaces, screens, keyboards, cables, monitors and anesthesia machines should be adequately decontaminated.
The aim during this COVID-19 times should be to conserve medical equipment such as masks, sanitizing gel or beds, while safeguarding the health of patients and health care personnel emergency cases requiring the use of OTs and ICUs.10
A proper OT exit pattern should be followed: surgical team, followed by patient after extubation, followed by anesthesia team, followed by cleaning and sterilization team.
Modifications in Diathermy Use
Electrocautery should be used at the lowest effective power setting and should be escorted by suction.1 Charring of tissues should be avoided to minimize the creation of smoke.5 During both open and laparoscopic surgery, the particle concentration may increase with use of energy sources. Use of monopolar electrosurgery, ultrasonic dissectors and bipolar machines should be reduced due to possibility of particle aerosolization.9 If unavoidable, monopolar diathermy pencils with attached smoke evacuators should be used. Energy devices should be minimally used. Cold hemostasis is the method of choice.7
Long dissecting times should be avoided on the same spot using energy devices to reduce surgical smoke. Sharp injury of protective equipment like gloves and body protection should also be avoided. Surgical drains should be used only if necessary. Suture closure devices for port closure that allow for leakage of insufflation should be avoided.7 Needle stick and stab injuries should be avoided.1
Laminar flow or air conditioner should not started until after intubation.5
Modification in Energy Device use in Lap/Minimal Access Surgery
Energy device produce plumes of surgical smoke. With the use of an energy device for 10 minutes, the concentration of the smoke in laparoscopic surgery is higher than the open surgery. It may be due to the small volume of gas in the pneumoperitoneum. Sudden release of trocar valves, non-air tight exchange of instruments or even small abdominal extraction incisions can expose the team to the pneumoperitoneum aerosol.37 Thus, it is recommended to use electrocautery at the lowest power setting possible.10
Negative Pressure OT
Negative pressure OT is an isolation technique used in hospitals to prevent cross-contamination from 1 OT to other. In negative pressure OT, air will flow from higher pressure to low pressure areas naturally, thereby avoiding contaminated air from escaping the OT room. Negative pressure inside the OT or, alternatively, frequent air change (25 cycle/hour) is advisable.1
Sodium Hypochlorite, Smoke and Under-Water Seal Evacuators
Post-surgery the OT should be cleaned with peroxyacetic acid/0.5-1% sodium hypochlorite/glutaraldehyde/benzalkonium chloride/ultraviolet C irradiation. Effective fumigation should be preferred.1,5,13 Stretcher should be sprayed with 1% hypochlorite solution after shifting the patients.5 Sodium hypochlorite solution 1% should be used for cleaning OT tables and trolleys after shifting the patient. Post-surgery all anesthesia equipment should be cleaned with 1% sodium hypochlorite solution.7 All the surfaces of medical devices should be cleaned with quaternary ammonium chloride disinfectant.
Suction should be performed with 2-bottle devices where 1 bottle should be filled with hypochlorite solution to allow the suctioned air/gas to pass through the solution before its evacuation into the second bottle. At the end of the procedure, complete desufflation should be done.5
Laparoscopy and MIS in Pediatric Surgery Patients during COVID-19 Times
Pediatrics with cancer are not severely affected by COVID-19. Most reports on COVID-19 in pediatrics describe mild to moderate symptoms such as fever, cough and nasal discharge.38 The infection is milder in pediatrics than in adults, but pediatrics or children undergoing cancer treatment have a weakened immune system which will make it tougher for the body to fight off COVID-19 infection. Also, pediatrics with COVID-19 infection may serve as vectors, likely to be important in disease transmission. Therefore, careful judgment should be made on what care requires postponement and what care is essential to be continued.
In addition to recommendations suggested for adults, reducing the number of attendances during and after laparoscopy and limiting the duration of clinical contact with children are necessary during the COVID-19 emergency. It is advisable to ensure preparation for early discharge. The goal should be to provide timely surgical care to pediatrics with critical issues while optimizing patient care resources (e.g., hospital and ICU beds, PPE, and ventilators) and preserving the health of health care team.39 Therefore, it is important for the surgeons as well as the children with their families to follow suggested recommendations for the protection. Each institution should adopt appropriate strategy according to their manpower, resources, and limitations. Similar to adults, the pediatric surgical care practices also need to be modified in hospitals.
Discussion
In this time of fear during the COVID-19 pandemic, we have discussed the safety measures recommended for health care professionals to prevent potential transmission of COVID-19 in laparoscopic or robotic surgeries. Numerous guidelines have been published related to the safety from the COVID-19 pandemic. SAGES cautioned about the possible risk of virus transmission during laparoscopy with CO2 and advised the use of devices to filter released CO2 for aerosolized particles.9 ERUS guidelines recommend to perform robotic surgery at the lowest intra-abdominal pressure.10 AORN recommends to evacuate the all surgical smoke as it contains hazardous chemicals, particles, bacteria, viruses, and cancer cells.11 Similarly, 1 report from the Annals of Surgery recommends to keep the pneumoperitoneum pressure and CO2 insufflation at the lowest level without compromise of the surgical field.19
A surgical smoke evacuator in each surgical approach (open, laparoscopic, or robotic) should be used. Self-maintained constant pneumoperitoneum system should be used. An adequate insufflation management system may enable the surgeon to operate at a low and stable pneumoperitoneum while minimizing the CO2 ventilation. Smoke evacuation through ULPA/HME filter can minimize the need to vent CO2 during laparoscopic procedures. We have described an indigenous method of safe smoke evacuation. Smoke evacuation disposables should be kept close to the source of smoke generation.7,9 For continuous active smoke evacuation and filtration for surgical procedures, dual-lumen smoke evacuation filtration can also be used. Ancillary suction-assisted smoke evacuation devices can be used to reduce the risk of aerosolized particles. During desufflation, the escaping CO2 gas and smoke should be passed through an ultrafiltration system, and desufflation mode should be used on insufflator.7 The use of devices with smoke evacuation filters may have a role in reducing the diffusion of COVID-19 although there are no specific data demonstrating the presence of the COVID-19 virus in the aerosol released during minimally invasive abdominal surgery.9 The potential benefits of MIS include minimum direct contact with the body tissues and shorter duration of hospitalization with reduced footfalls in the hospital. On the other hand, the chances of aerosolized particles in open surgery are high. Based on these facts, the potential benefits and risks of the surgical approach should be carefully weighed when considering laparoscopic vs open approach.5 The benefits and risks associated with robot-assisted, conventional laparoscopic and open surgery under COVID-19 times are compared in Table 1.40,41 Based on these recommendations, apart from indigenous systems, the current options available for laparoscopy and robotic during MIS minimal access surgeries during the COVID-19 pandemic include Buffalo filter, CONMED AIRseal System, Coviden RapidVacTM, smoke evacuator system.
Table 1.
Benefits and Risks of Surgical Approach (Robot-Assisted, Conventional Laparoscopic, and Open Surgeries) under COVID-19 Times.
| Area of Risk | Robot-Assisted Surgery | Conventional Laparoscopy | Open Surgery |
|---|---|---|---|
| Aerosol escape | Intra-abdominal dispersion, limited by filters or locks (no data on actual COVID-19 risk) | Intra-abdominal dispersion, limited by filters or locks (no data on actual COVID-19 risk) | Less aerosol formation, unconfined dispersion, unfiltered. Only present, but then unfiltered, and with maximal exposure, when using electrical and especially ultrasonic devices (no data on actual COVID-19 in risk) |
| Smoke | Confined, filtered, and less than at open surgery | Confined, filtered, and less than at open surgery | Maximum exposure to smoke |
| Blood, body fluids | Hardly if any blood loss and exposure at limited intervals | Hardly if any blood loss and exposure at limited intervals | More blood loss and constant exposure |
| Abdominal pressure | Minimal pressure (less than at conventional laparoscopy). Less than 10 mmHg | 10-15 mmHg | No abdominal pressure (0 mmHg) |
| Perioperative cleaning of instruments | Large surface of robot to disinfect, but limited number of instruments to clean of limited blood contamination | Limited number of instruments to clean of limited blood contamination | Only instrument to clean but these in large number and severely contaminated with blood |
| Health care staff | Usually 1 staff at the bedside, 1 staff away from the patient (remote) | Usually 3 staff at the bedside | Usually 3 staff at the bedside |
| Hospital stay | Short | Short | Long |
Currently, the best approach to tackle COVID-19 transmission during open, laparoscopic, and endoscopic surgeries is to use a multipronged approach which includes proper room filtration and ventilation, use of appropriate PPE, and smoke evacuation devices with a suction and filtration system. By following the recommendations from different guidelines, we can tackle the COVID-19 pandemic during surgical intervention of urgent cases which cannot be delayed (Table 2).
Table 2.
COVID-19 Surgical Patient’s Management Recommendations.
| Procedure and Recommendations |
|---|
| OT room |
| Dedicated OT room should be used |
| OT room should be adequately filtered and ventilated an integrated HEPA |
| High rate of air exchange >25 cycles/hour should be used |
| Negative pressure OT room should be preferred |
| Surgical equipment used for confirmed or suspected COVID-19 patients should be cleaned separately from other surgical equipment |
| Endoscopic procedures requiring additional insufflation of CO2 or room air should be avoided |
| Surgical aid such as OT trolley, laparoscopic trolley, anesthesia trolley, and gas cylinders should be used to avoid the increase in OT time |
| Surgeries should be performed with the minimum number of OT staff members |
| OT should be cleaned and sterilized post-surgery |
| Disposable materials (such as gloves or paper towel) should be used for cleaning |
| A minimum of 1 hour gap should be there between 2 surgical procedures |
| Consent discussion with patients to cover the risk of COVID-19 exposure and the potential consequences |
| Laparoscopy trocar cannula modifications |
| Incisions for ports should be very small to permit for the passage of ports but not for leakage around ports |
| Once placed port should not be used for evacuation of smoke or for desufflation without taking adequate precautions |
| Traditional trocars may be used with one-way valves within the proximal portion of the port |
| CO2 insufflation pressure should be minimum and an ultrafiltration (smoke evacuation system or filtration) should be used |
| All pneumoperitoneum should be safely evacuated via a filtration system before closure, trocar removal, specimen extraction, or conversion to open |
| Insufflator should be turned off only after the port that was used for inflation was closed to prevent gas going into the insufflator tubing |
| Smoke evacuators |
| Ultrasonic scalpels or electrical equipment used in MIS can produce huge amounts of surgical smoke |
| Standard electrostatic filters should be used in ventilation machines as these can filter bacterial and viral loads with great efficacy |
| Filters should be connected via standard tube to the trocar evacuation port which can evacuates the produced smoke and filter the possible viral load |
| Use of intelligent integrated flow systems is recommended for the maintenance of low intraabdominal pressure which ensures a self-maintained constant pneumoperitoneum |
| Integrated flow systems should be configured in a continuous smoke evacuation and filtration mode |
| HME filter with or without HEPA filter and under water seal sodium hypochlorite for lap evacuator under seal sodium hypochlorite can be used |
| Buffalo filters |
| Buffalo filter smoke evacuator tubing is connected to 2 HME filters and placed under the drape to provide air filtration. The use of multifilter system ensure maximum efficiency in filtering viral particles |
| Anesthesia modifications |
| Intubation during general anesthesia may result in general aerosolization, causing risk to anesthesia team as well as the OT person |
| During time of intubation or extubation barrier enclosures made up of plastic or acrylic as would decrease risk considerably |
| Preference should be given to regional anesthesia. Regional anesthesia offers benefits of preservation of respiratory function, avoidance of aerosolization, and hence viral transmission |
| Laminar airflow or air conditioner should be started after induction of anesthesia. Laminar airflow or air conditioner should be stopped 20 minute before the extubation |
| Reduce the Trendelenburg position time as much as possible. This minimizes the effect of pneumoperitoneum on lung function and circulation, in an effort to reduce pathogen susceptibility |
| Personal protections to surgeons |
| All elective surgical and endoscopic cases should be postponed at the current time, if not urgent |
| Surgeons must avoid contact with droplets and full body protection |
| Universal protection with PPE (appropriate gowns, N95/FFP2-3 masks, and face shields/goggles) are strongly recommended for surgeons |
| Surgery should be performed by the most qualified surgeon to minimize operative time |
| Donning of PPE should be done in the OT room and doffing should be done in wash area |
| MDT meetings should be virtual and restricted to core team members only |
| No 1 except the necessary staff should allowed inside OT while intubation and extubation |
| Senior oncologists (age >60 years) and those with co-morbidities should be abstain from surgery |
| Special care should be taken by the anesthetists or surgeons and endoscopists |
| All PPE should be removed outside the room |
| A proper OT exit pattern should be followed: Surgical team followed by patent after extubation followed by anesthesia team followed by cleaning and sterilization team |
| Cautery/diathermy low setting modifications |
| Electrocautery should be used in a lower power setting and should be escorted by suction |
| Charring of tissues should be avoided to minimize the creation of smoke |
| Energy devices should be minimally used. Cold hemostasis is the method of choice. Use more of clips and sutures |
| Long dissecting times should be avoided on the same spot using energy devices to reduce the surgical smoke |
| Energy devices used in lap minimal access surgery modifications |
| Energy device produce plume surgical smoke |
| With the use of energy device for 10 minute, the particle concentration of the smoke in laparoscopy surgery is higher than the open surgery |
| Sudden release of trocar valves, non-air tight exchange of instruments or even small abdominal extraction incisions can expose the team to the pneumoperitoneum aerosol |
| Negative pressure OT |
| Negative pressure inside the OT and alternatively frequent air change |
| It is important to perform surgeries at the lowest intra-abdominal pressure |
| Sodium hypochlorite smoke and gas under seal evaluators |
| Post-surgery the OT should be clean with peroxyacetic acid/0.5-1% sodium hypochlorite/gluraldehyde/benzalkonium chloride |
| Effective fumigation should be preferred |
Abbreviations: CO2 = carbon dioxide; HEPA = high-efficiency particulate air; HME = heat and moisture exchanger; MDT = multidisciplinary team; MIS = minimum invasive surgery; OT = operation theater; PPE = personal protection equipment.
Conclusion
Our health care system needs to quickly acclimatize to this rapidly changing environment of the COVID-19 pandemic. The next few months are crucial in alleviating the transmission of COVID-19 infection. The best outcomes for all can be achieved when individual patient and local circumstances are taken into account, along with surgical experience and judgment. Surgical treatment should be performed only for emergent, nondeferrable cases. In addition to surgical patients, health care workers should also protect themselves by following the guidelines while treating the surgical patients. Although there is little evidence of viral transmission through laparoscopic or open approaches, we still recommend modifications to surgical practice such as the use of smoke evacuation and minimizing energy device use to reduce the risk of aerosolized particle exposure to health care personnel. Therefore, it is necessary to follow best surgical practices by adhering to careful management plan and thoughtful methodology.
Footnotes
Author Contributions: Study concept and design: SP Somashekhar and S Manjiri
Acquisition of data: Rudra Acharya, C Rohit Kumar, and KR Ashwin
Study supervision: SP Somashekhar, KR Ashwin, and C Rohit Kumar
Analysis and interpretation: SP Somashekhar, S Manjiri, and Sumit Talwar
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
SP Somashekhar https://orcid.org/0000-0002-7898-1625
References
- 1.IASO (Indian Association of Surgical Oncology) . IASO Covid-19 guidelines. Updated April 16, 2020. https://iasoindia.in/ [DOI] [PMC free article] [PubMed]
- 2.Patel R, Babady E, Theel ES, et al. Report from the American Society for Microbiology COVID-19 international summit, 23 March 2020: Value of diagnostic testing for SARS–CoV-2/COVID-19. mBio. 2020;11:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Muharraqi MA. Testing recommendation for COVID-19 (SARS-CoV-2) in patients planned for surgery-continuing the service and ‘suppressing’ the pandemic. Br J Oral Maxillofac Surg. 2020;S0266-4356(20):30164-30169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVID-19 ER Kit . COVID-19 rapid IgG/IgM combined antibody assay. 2020. https://sensingself.me/covid.php
- 5.AMASI (Association of Minimal Access Surgeons of India) . AMASI guideline for conducting minimal access surgery during COVID-19 pandemic. 2020. https://www.amasi.org/
- 6.COVID-19 Rapid Antibody Test . 2020. Available athttps://www.biopanda.co.uk/php/products/rapid/infectious_diseases/covid19.php
- 7.Inter Association Guideline . Inter association surgical practice recommendations in COVID 19 era (For minimal access surgeons in India). April 23, 2020. [Google Scholar]
- 8.Suriraju V. Postponing of routine surgeries needed amidst corona outbreak. 2020. Available athttps://ehealth.eletsonline.com/2020/03/postponing-of-routine-surgeries-needed-amidst-corona-outbreak/
- 9.EAES and SAGES Guideline . Recommendations regarding surgical response to COVID-19 crisis. Released March 30, 2020. https://eaes.eu/eaes-and-sages-recommendations-regarding-surgical-response-to-covid-19-crisis/
- 10.ERUS (EAU Robotic Urology Section) . Guideline. 2020. Available athttps://uroweb.org/wp-content/uploads/ERUS-guidelines-for-COVID-def.pdf
- 11.AORN (Association of PeriOperative Registered Nurses) . Guideline. 2020. Available athttps://www.aorn.org/guidelines/aorn-support/covid19-faqs
- 12.Ficarra V, Novara G, Abrate A, et al. Urology practice during COVID-19 pandemic. Minerva Urol Nefrol. 2020;72:369-375. [DOI] [PubMed] [Google Scholar]
- 13.Bhattacharya K. Are surgeons in India prepared for COVID-19? Indian J Surg. 2020;17:1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67:568-576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liana Z, Nadav L, Desire K, Mike A, Satya KR. Anesthesia patient safety foundation. 2020. Available athttps://www.apsf.org/news-updates/perioperative-considerations-for-the-2019-novel-coronavirus-covid-19/
- 16.Coccolini F, Perrone G, Chiarugi M, et al. Surgery in COVID-19 patients: Operational directives. World J Emerg Surg. 2020;15:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vigneswaran Y, Prachand VN, Posner MC, Matthews JB, Hussain M. What is the appropriate use of laparoscopy over open procedures in the current COVID-19 climate? J Gastrointest Surg. 2020;24:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mintz Y, Arezzo A, Boni L, et al. A low cost, safe and effective method for smoke evacuation in laparoscopic surgery for suspected coronavirus patients. Ann Surg. 2020;272:e7-e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: Lessons learned in China and Italy. Ann Surg. 2020;272:e5-e6. https://journals.lww.com/annalsofsurgery/Documents/Minimally%20invasive%20surgery%20and%20the%20novel%20coronavirus%20outbreak%20-%20lessons%20learned%20in%20China%20and%20Italy.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Capizzi PJ, Clay RP, Battey MJ. Microbiologic activity in laser resurfacing plume and debris. Laser Surg Med. 1998;23:172-174. [DOI] [PubMed] [Google Scholar]
- 21.Hensman C, Baty D, Willis RG, Cuschieri A. Chemical composition of smoke produced by high-frequency electrosurgery in a closed gaseous environment. An in vitro study. Surg Endosc. 1998;12:1017-1019. [DOI] [PubMed] [Google Scholar]
- 22.Johnson GK, Robinson WS. Human immunodeficiency virus-1 (HIV-1) in the vapors of surgical power instruments. J Med Virol. 1991;33:47-50. [DOI] [PubMed] [Google Scholar]
- 23.Kwak HD, Kim SH, Seo YS, Song KJ. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Occup Environ Med. 2016;73:857-863. [DOI] [PubMed] [Google Scholar]
- 24.Gloster HM, Roenigk RK. Risk of acquiring human papillomavirus from the plume produced by the carbon dioxide laser in the treatment of warts. J Am Acad Dermatol. 1995;32:436-441. [DOI] [PubMed] [Google Scholar]
- 25.Van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564-1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dellamonica J, Boisseau N, Goubaux B, Raucoules-Aimé M. Comparison of manufacturers’ specifications for 44 types of heat and moisture exchanging filters. Br J Anaesth. 2004;93(4):532-539. [DOI] [PubMed] [Google Scholar]
- 27.Alp E, Bijl D, Bleichrodt RP, Hansson B, Voss A. Surgical smoke and infection control. J Hosp Infect. 2006;62:1-5. [DOI] [PubMed] [Google Scholar]
- 28.Choi SH, Kwon TG, Chung SK, Kim T-H. Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc. 2014;28:2374-2380. [DOI] [PubMed] [Google Scholar]
- 29.Chaudhary A. Difference between HEPA and ULPA Filters. 2020. Available athttps://www.pharmaguideline.com/2019/01/difference-between-hepa-and-ulpa-filters.html
- 30.Kim J-M, Chung Y-S, Jo HJ, et al. Identification of coronavirus Isolated from a patient in Korea with COVID-19. Osong Public Health Res Perspect. 2020;11:3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu G, Lou Z, Zhang W. Several considerations on the operation of colorectal cancer under the epidemic situation of new coronavirus pneumonia. Chinese J Gastrointestinal Surg. 2020;23:9-11. [Google Scholar]
- 32.Foster P, Cheung T, Craft P, et al. Novel approach to reduce transmission of COVID-19 during tracheostomy. J Am Coll Surg. 2020;230:1102-1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lie SA, Wong SW, Wong LT, Wong TGL, Chong SY. Practical considerations for performing regional anesthesia: Lessons learned from the COVID-19 pandemic. Can J Anaesth. 2020;67:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tang G, Chan M. Perioperative management of suspected/confirmed cases of COVID-19. General Anesthesia. 2020. Available athttps://www.wfsahq.org/components/com_virtual_library/media/1c4ec5c64b9aaacf7c47f76a61fb6edc-atow-422-01.pdf
- 35.Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: Is faecal-oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020;5:335-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ling Y, Xu SB, Lin YX, et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J (Engl). 2020;133:1039-1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li CI, Pai JY, Chen CH. Characterization of smoke generated during the use of surgical knife in laparotomy surgeries. J Air Waste Manag Assoc. 2020;70:324-332. [DOI] [PubMed] [Google Scholar]
- 38.Quaedackers JSLT, Stein R, Bhatt N, et al. Clinical and surgical consequences of the COVID-19 pandemic for patients with pediatric urological problems: Statement of the EAU guidelines panel for paediatric urology, March 30 2020. J Pediatr Urol. 2020;16(3):284-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.ACS (American College of Surgeons) . COVID-19 guidelines for triage of pediatric patients. 2020. Available athttps://www.facs.org/covid-19/clinical-guidance/elective-case/pediatric-surgery
- 40.Kimmig R Verheijen RHM Rudnicki M, for SERGS Council . Robot assisted surgery during the COVID-19 pandemic, especially for gynecological cancer: A statement of the Society of European Robotic Gynaecological Surgery (SERGS). J Gynecol Oncol. 2020;31(3):e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Society of European Gynaecological Surgery (SERGS Statement) . Statement on the use of robot assisted surgery (RAS) during the COVID-19 pandemic. 2020. Available athttps://www.sergs.org/media/2020/04/SERGS-Statement-finalApr1.pdf