Abstract
Objectives: Commentaries have suggested that initial emphasis on the higher susceptibility and mortality rates of older adults to COVID-19 has instigated ageism within the public discourse and policy decisions. Using the health belief model, the current study examined ageism in interaction with other factors influencing intention to social distance. Methods: Threat of contracting COVID-19, benefits and barriers to social distancing, benevolent and hostile ageism, and intention to social distance were examined in 960 adults (M = 37.81 years, SD = 11.65). Results: Benevolent and hostile ageism were significant moderators for both perceived threat and barriers on intent to social distance; hostile ageism also moderated benefits on intent to social distance. Discussion: The current study demonstrates how ageism influences behavior during a pandemic. With initial reports of COVID-19 presenting older adults as a homogenous group, ageism negatively interacted with intention to social distance and may place older adults at greater risk.
Keywords: ageism, COVID-19, health belief model, social distancing, health behaviors
On March 11, 2020, the World Health Organization declared the coronavirus disease 2019 (COVID-19) outbreak a pandemic (Centers for Disease Control and Prevention, 2020). This disease is a serious public health threat, impacting people around the world. With federal and local governments working to reduce spread, the majority of the US population has been advised to stay home (Gostin & Wiley, 2020), with nonessential businesses required to close or take additional safety measures. The higher susceptibility rates of older adults compared to other age-groups have unearthed ageist responses within the public discourse and in formal policy decisions regarding medical resource allocation (Colenda, et al., 2020), contributing to the view of older adults as a homogeneously vulnerable population. With blatant displays of ageism and heightened intergenerational tension (Ayalon, 2020), it is essential to understand the impact that ageism may have on a person’s intention to participate in recommended prevention measures.
Ageism
Ageism is defined as prejudice, discrimination, and overgeneralization on the basis of age (Butler, 1969; North & Fiske, 2013). It is unique from other forms of prejudice as the beliefs held about age may inadvertently influence ones’ own aging process as they become the stereotype target (Levy, 2009). Swift et al., 2017 identified three mechanisms by which ageism disrupts active aging, two of which emphasize the internalization of ageist beliefs: (1) stereotype embodiment (e.g., Levy, 2009); (2) stereotype threat (e.g., Lamont et al., 2015); and (3) age discrimination (e.g., Nelson, 2016).
Researchers have established that not all age-related beliefs are negative (e.g., Hummert, 1990; Kite et al., 2005) and can be distinguished along similar dimensions to sexism, resulting in hostile and benevolent forms (Cary et al., 2017). Hostile ageism encompasses harsh criticisms of later life, the perspective of older adults as a societal drain and burden, resulting in dismissive or resentful actions. Benevolent ageism, on the other hand, stereotypes older adults as fragile and dependent, and may result in actions that superficially appear as compassionate, but carry an undercurrent of control or patronization of older adults. Although hostile and benevolent ageism sound like two extremes of a single continuum, these forms of ageism, much like sexism (e.g., Glick & Fiske, 2001), are frequently found to be moderately correlated, resulting in ambivalence toward older adults (Cary et al., 2017). Prejudiced beliefs, regardless of whether they come from a place of resentment or pity, produce thoughts and actions that minimize the stereotyped target based on assumption rather than actual individual differences. In turn, these beliefs may influence treatment of the stereotyped targets (Nelson, 2016).
Ageism in the Time of COVID-19
In April 2020 (the time at which data were collected for the current study), details about the spread of COVID-19 were rapidly emerging even though the disease had been present and expanding in Wuhan, China since December 2019. One consistently reported finding was the differential susceptibility and mortality of those in their later years (Le Couteur et al., 2020). Early recommendations, including “social distancing,” targeted primarily older adults and those with known immunodeficiency circumstances (Rahman & Jahan, 2020). Le Couteur et al., 2020 and others (Ayalon, 2020; Brooke & Jackson, 2020) highlighted the risk of blanket statements and policies that identify older adults as a “high risk” population, including but not limited to threats to their socioemotional well-being as a result of isolation, anxiety, and increased ageism. Implicit ageism surfaced as some individuals outside of these high risk groups have downplayed the loss of life within these populations and declared themselves exempt from participating in safe practices due to the perception of low personal risk (D’cruz & Banerjee, 2020).
Indeed, many authors have addressed a rise in explicit ageism as witnessed in proposed healthcare policies (e.g., rationing treatment; Cesari & Proietti, 2020) and social media (e.g., referring to COVID-19 as #boomerremover as cited by Ayalon, 2020; Jimenez-Sotomayor et al., 2020). Others have talked about the long-term implications of heightened internal and external ageism in the aftermath of COVID-19, including stereotype embodiment and generational transmission of internalized ageism for younger adults (Ayalon et al., 2020), as well as difficulty recovering economically and socially in an age-unfriendly environment with persons of color and those in lower socioeconomic situations bearing an even greater burden (Morrow-Hollow et al., 2020). While most of the published articles focus on hostile ageism wherein older adults are dismissed as useless, expendable burdens, others (e.g., Fraser et al., 2020) point to the way in which benevolent ageism (i.e., stereotypes that view older adults’ as fragile and vulnerable, and thus in need of protection), while patronizing, may appear as intergenerational solidarity in the face of crisis (Ayalon et al., 2020). Stereotypes that elevate dependency, much like benevolent sexism, may be well-meaning but still perpetuate expectations of older adults as a homogenous population and objects to be cared for. Therefore, in the context of a pandemic where age has been highlighted as a salient risk factor, ageism may interact with other deciding factors in determining whether an individual will engage in preventative behaviors.
Theoretical Model for Understanding Engagement in Preventative Behaviors
Several models exist to organize the factors influencing engagement in preventative health behaviors, including the health belief model (HBM; Becker et al., 1978; Hochbaum, 1958; Janz & Becker, 1984; Champion, 1993). The HBM draws on psychological beliefs and perceptions in the context of moderating personal factors and contextual cues to predict the likelihood of preventative behavior. It has been used to examine both behavioral intentions and performed behavior across prevention behaviors including health screenings (e.g., Tanner-Smith & Brown, 2010), self-care medical regimens (e.g., Jones et al., 2014), and vaccinations (e.g., Kan & Zhang, 2018). The original HBM model included perceived susceptibility and severity of the avoided health condition (collectively, perceived threat) and perceived benefits and barriers of the preventative behavior (Becker et al., 1978; Hochbaum, 1958; Janz & Becker, 1984) in the context of personal and contextual modifying factors.
The current study applied the original four-factor HBM as a framework to examine internal and external factors influencing intention to social distance near the beginning of the first wave of COVID-19 in the United States. The HBM has been prominently used in examining preventative behaviors during other health crises internationally, including H1N1 and seasonal influenza with a primary focus on vaccination behavior (e.g., Ashbaugh et al., 2013; Huang et al., 2012; Fall et al., 2018; Setbon & Raude, 2010). These studies reflect a complicated picture of both the individual and interactive relationships among the HBM constructs.
At least one known study (Durham et al., 2012) examined the HBM in relation to crowd avoidance, or what is presently being referred to as “social distancing,” during the 2009–2010 H1N1 pandemic. In a longitudinal investigation of the original HBM in relation to both vaccination and crowd avoidance beliefs, univariate logistic correlations demonstrated that perceived benefit of avoiding crowds (i.e., effective as a preventative measure) and perceived severity (i.e., likelihood to die from illness) were the only HBM-specific predictors of crowd avoidance. Durham et al., 2012 also examined “cues to action,” such as media coverage and knowing someone who contracted the illness. In a multivariate regression model, perceived benefit was the only HBM-specific predictor to remain significant, along with age (older more likely) and gender (men less likely) as significant personal factors of crowd avoidance. Durham et al., 2012 suggest that some of the relationships may be changed or altered by cues to actions, and that their conclusions may have been weakened by the timing of their data collection at the downward trend of the H1N1 pandemic curve. The current study is similar in our application of HBM constructs, expanding to examine ageism as a possible modifying factor, given the saliency of age as a risk factor for severe consequences from COVID-19. Although not longitudinal, we examine these factors at the rise of the pandemic curve.
Current Study
Given the presentation of age as a primary risk factor, we set out to examine whether ageist beliefs (separated as hostile and benevolent) predicted intention to social distance in the early stages of the COVID-19 pandemic in the United States. We expected those higher on hostile ageism to report lower intention to social distance (as a dismissive action) and those higher on benevolent ageism to report higher intention to social distance (as a protective action). We also examined how ageism interacted with other known predictors of intention to social distance as a preventative health behavior, using the HBM as an organizational framework. Perceived threat (a combination of susceptibility and severity), perceived benefits, and perceived barriers of social distancing were examined in relation to intention to social distance with ageism moderating the relationship. In this way then, ageism was acting as a modifying factor in the model. Typically, greater perceived threat, more benefits, and fewer barriers predict increases in preventative behavior intentions and actual behavior (Kan & Zhang, 2018). With ageism as a moderator, we anticipated those reporting higher ageism to report a reduced intention to social distance, despite the above described circumstances.
Methods
Participants
Eligibility for the study required accessing Amazon’s Mechanical Turk (MTurk) with a US-originating IP address and having an approval rating on the site of 95% or better. MTurk is a micro-task website that allows “workers” to be paid for their participation in online tasks, such as surveys (Patrick, et al., 2016). The original sample (n = 1040) was reduced, omitting participants who failed multiple attention checks (n = 42) and those with 5% or more missing data (n = 38). Therefore, the final sample for analysis contained 960 participants. Participants in the final sample ranged in age from 18 to 73 years (M = 37.81, SD = 11.65). The majority identified as male (59.4%), white (71.5%), and educated at the level of a bachelor’s degree (64.7%). Close to 50 participants (4.8%) reported being diagnosed with COVID-19.
Measures
Health belief model variables
The HBM (Becker et al., 1978; Hochbaum, 1958; Janz & Becker, 1984; Champion, 1993) was used as a theoretical model to identify and organize factors influencing the likelihood of participants to engage in social distancing as a primary preventative behavior in the spread of COVID-19. There is difficulty in the consistency of applying this model due to measurement (Champion & Skinner, 2008) as all components of the model must be tailored to the specific behavior of focus. For the current study, items were adapted from existing measures of the HBM (Gözüm & Aydin, 2004; Vernon et al., 1997) and tailored using previous research on other pandemic-scale illnesses (e.g., Ashbaugh et al., 2013; Huang et al., 2012; Myers & Goodwin, 2011; Setbon & Raude, 2010) as well as media and governmental reports made available at the time of measure development (late March 2020). With less than 1% of scores missing for any given question, mean imputation was conducted if a participant had completed at least 75% of the questions.
Behavioral intention
The measure of behavioral intention consisted of 11 items; sample questions included the following: “I do not intend to change my routine in order to social distance” and “I do not intend to self-isolate if I travel across state lines during this time.” Each item was scored on a 5-point Likert-type scale (1: strongly disagree to 5: strongly agree). Six of the items were reverse scored. Scores were averaged over the 11 items (range: 1.45–5), with higher scores on the scale representing higher levels of behavioral intent (M = 3.96, SD = .75, and α = .84).
Perceived threat (susceptibility and severity)
The measure of perceived threat consisted of 12 items; questions included the following: “It is likely that I will get coronavirus (COVID-19),” and “I think that compared to other persons my age, I am at a lower risk for contracting COVID-19.” Each item was scored on a 5-point Likert-type scale (1: strongly disagree to 5: strongly agree). Two items were reverse scored. Scores were averaged over the 12 items (range: 1–5), with higher scores on the scale representing higher levels of perceived threat (M = 3.03, SD = .78, and α = .86).
Benefits and barriers (beliefs)
The measure of beliefs consisted of 40 items with 20 items examining benefits and 20 items examining barriers. The subscales of benefits and barriers were assessed separately in the analyses but were interspersed throughout the scale. A sample question for benefits included “Social distancing makes sense to me as a preventative measure” and for barriers included “I am worried about the effect social distancing will have on my career.” Half of the items were reverse scored prior to scaling. Each item was scored on a 5-point Likert-type scale (1: strongly disagree to 5: strongly agree). Scores for benefits were averaged over the 20 items (range: 1.10–5), with higher scores on the scale representing higher levels of perceived benefits (M = 4.20, SD = .71, and α = .94). Scores for barriers were averaged over the 20 items (range: 1–4.70), with higher scores on the scale representing higher levels of perceived barriers (M = 2.21, SD = .97, and α = .95).
Ageism—Benevolent and Hostile
Ageism was measured with the two subscales measuring benevolent and hostile ageism of the Ambivalent Ageism Scale (AAS; Cary et al., 2017). The hostile (4 items; ex. “Old people are a drain on the health care system and the economy”) and benevolent (9 items; “Even if they do not ask for help, older people should always be offered help”) subscales of the AAS recognize that ageism is multidimensional. Each item is measured on a 7-point Likert scale ranging from 1: strongly disagree to 7: strongly agree. Scores for each subscale are averaged with lower scores indicating less benevolent ageism (M = 3.54, SD = 1.39) and hostile ageism (M = 3.11, SD = 1.59). Reliabilities for each subscale (benevolent α = .92; hostile α = .91) were good.
Procedures
This study was a cross-sectional survey utilizing a convenience sample of adults over the age of 18, recruited from a crowdsourcing website. Data were collected in the span of 2 days in mid-April 2020. Participants were recruited through a study advertisement on MTurk, inviting participants to complete an online survey on behaviors and beliefs influencing adjustment during a global health pandemic. Other than a US-originating IP address, there were no additional eligibility requirements, although attention checks were embedded throughout the survey and data were screened for duplicate IP addresses. Participants accessed the survey, hosted by Qualtrics. An informed consent gated access to the survey. Once consent was granted by clicking a radial dial, participants completed several questions related to health in general, beliefs and behaviors in response to COVID-19, aging, and religious participation. They finished with a series of demographic questions. The study took approximately 15 minutes to complete, after which participants were directed to resources on COVID-19 and compensated for their participation (2USD). This research complied with APA ethical standards and was approved through Northern Kentucky University’s Institutional Review Board (protocol #988).
Analytical Strategy
A power analysis, using G*Power (Erdfelder et al., 1996), suggested that data from 109 adults would provide sufficient power (power = .80) to detect medium-sized effects (f2 = .15) in a 3-variable regression equation (p < .05). Because traditional approaches are not well suited for estimating power in moderated regression analyses (Hayes, 2012), PROCESS was adopted. PROCESS (Hayes, 2012) was used to test whether benevolent and hostile ageism moderated the effect of health belief model variables on behavioral intention, with race (coded as POC/white), gender (female/male), and age (continuous) as covariates. PROCESS was adopted over traditional methods of testing moderations because it allowed for 5000 bias-corrected boot-strapping samples which increase the stability of the beta weights, and continuous variables are automatically mean centered which ensure assumptions of generalized linear models were not violated (Hayes, 2012).
Results
To ascertain preliminary bivariate associations between behavioral intentions, benevolent and hostile ageism, perceived threat, benefits, and barriers, Pearson correlations were examined. Behavioral intentions were significantly associated with benevolent ageism (r(956) = −.39 and p = .00), hostile ageism (r(958) = −.55 and p = .00), benefits (r(960) = .72 and p = .00), barriers (r(960) = −.76 and p = .00), age (r(959) = .13 and p = .00), gender (r(951) = .20 and p = .00), and race (r(954) = .12 and p = .00). Behavioral intentions were not significantly associated with perceived threat (r(959) = .06 and p = .06). Benevolent ageism was significantly associated with hostile ageism (r(955) = .76 and p = .00), perceived threat (r(955) = .19 and p = .00), benefits (r(956) = −.15 and p = .00), barriers (r(956) = .58 and p = .00), age (r(955) = −.26 and p = .00), gender (r(947) = −.18 and p = .00), and race (r(950) = −.26 and p = .00). Hostile ageism was significantly associated with perceived threat (r(957) = .14 and p = .00), benefits (r(958) = −.30 and p = .00), barriers (r(958) = .68 and p = .00), age (r(957) = −.26 and p = .00), gender (r(949) = −.20 and p = .00), and race (r(952) = −.25 and p = .00) (see Table 1 for all correlations).
Table 1.
Mean, SD, and Pearson correlations.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| (1) Behavioral intentions (M = 3.96 and SD = .75) | – | – | – | – | – | – | ||
| (2) Benevolent ageism (M = 3.54 and SD = 1.39) | −.39** | – | – | – | – | – | ||
| (3) Hostile ageism (M = 3.11 and SD = 1.59) | −.55** | .76** | – | – | – | – | ||
| (4) Susceptibility/severity (M = 3.03 and SD = .78) | .06 | .19** | .14** | – | – | – | ||
| (5) Benefits (M = 4.20 and SD = .71) | .72** | −.15** | −.30** | .24** | – | – | ||
| (6) Barriers (M = 2.21 and SD = .97) | −.76** | .58** | .68** | .24** | −.46** | – | ||
| (7) Age (M = 37.81 and SD = 11.65) | .13** | −.26** | −.26** | .05 | .11** | −.21** | ||
| (8) Gender (coded as 0: male and 1: female) | .20** | −.18** | −.20** | .08∗ | .12** | −.16** | .20** | |
| (9) Race (coded as 0: POC and 1: white) | .12** | −.26** | −.25** | −.10** | .00 | −.19** | .20** | .06∗ |
Note.** Correlation is significant at the .01 level; * correlation is significant at the .05 level.
Moderation analyses were conducted to determine whether benevolent and hostile ageism moderated the effects of health belief model variables on behavioral intent. Age, race, and gender were controlled for in all models, given previous literature suggesting the influence of these variables on intention to socially distance (e.g., Durham et al., 2012).
Benevolent Ageism
Perceived threat
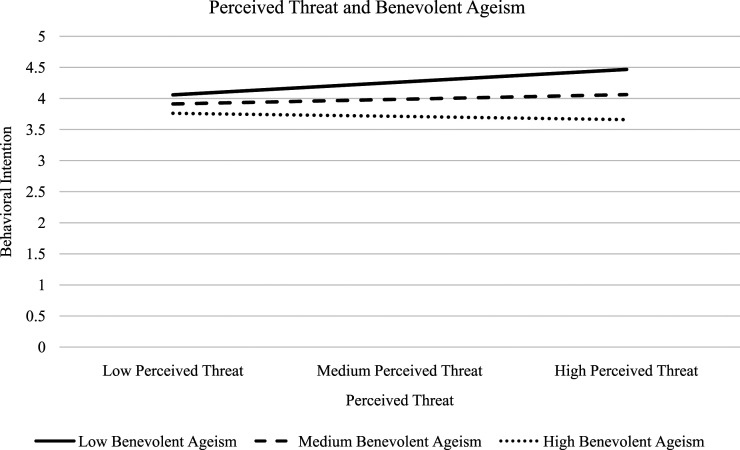
In the equation examining whether benevolent ageism moderated the effects of perceived threat on behavioral intent, an omnibus effect was detected [F(6, 936) = 41.64, p = .00, and R2= .21]. Benevolent ageism [b = −.19 and p = .00], perceived threat [b = .10 and p = .00], and the interaction [b = −.12 and p = .00] all uniquely contributed to the overall effect on behavioral intent (see Figure 1 for the interaction of perceived threat and benevolent ageism). By examining the conditional effects, it was found that at low levels of benevolent ageism, for a one unit increase in perceived threat, there is a .26 increase in behavioral intention, b = .26, t(936) = 6.83, and p < .00. At average levels of benevolent ageism, for a one unit increase in perceived threat, there is a .10 increase in behavioral intention, b = .10, t(936) = 3.33, and p < .00. At high levels of benevolent ageism, there is no significant relationship between perceived threat and behavioral intention, b = −.07, t(936) = −1.59, and p = .11.
Figure 1.
Graph of the interaction between perceived threat and benevolent ageism on behavioral intent.
Benefits
In the equation examining whether benevolent ageism moderated the effects of benefits on behavioral intent, an omnibus effect was detected [F(6, 937) = 235.72, p = .00, and R2= .60]. Benevolent ageism [b = −.15 and p = .00] and benefits [b = .70 and p = .00] uniquely contributed to the overall effect on behavioral intent, but the interaction [b = −.003 and p = .88] did not significantly contribute to the model.
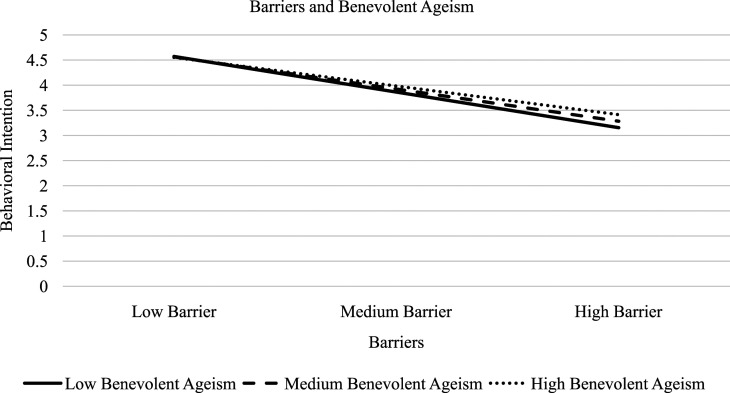
Barriers
In the equation examining whether benevolent ageism moderated the effects of barriers on behavioral intent, an omnibus effect was detected [F(6, 937) = 226.74, p = .00, and R2= .59]. Benevolent ageism [b = .04 and p = .00], barriers [b = −.66 and p = .00], and the interaction [b = .05 and p = .00] uniquely contributed to the overall effect on behavioral intent (see Figure 2 for the interaction of barriers and benevolent ageism). By examining the conditional effects, it was found that at low levels of benevolent ageism for a one unit increase in barriers there is a −.73 decrease in behavioral intention, b = −.73, t(937) = −21.51, and p < .00. At average levels of benevolent ageism, for a one unit increase in barriers, there is a −.66 decrease in behavioral intention, b = −.66, t(937) = −29.22, and p < .00. At high levels of benevolent ageism, for a one unit increase in barriers, there is a −.59 decrease in behavioral intention, b = −.59, t(937) = −28.21, and p < .00.
Figure 2.
Graph of the interaction between barriers and benevolent ageism on behavioral intent.
Hostile Ageism
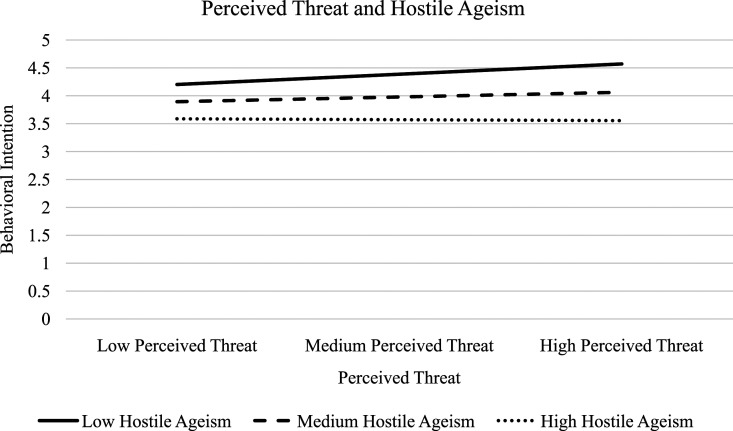
Perceived threat
In the equation examining whether hostile ageism moderated the effects of perceived threat on behavioral intent, an omnibus effect was detected [F(6, 938) = 82.15, p = .00, and R2= .34]. Hostile ageism [b = −.26 and p = .00], perceived threat [b = .11 and p = .00], and the interaction [b = −.08 and p = .00] all uniquely contributed to the overall effect on behavioral intent (see Figure 3 for the interaction of perceived threat and hostile ageism). By examining the conditional effects, it was found that at low levels of hostile ageism, for a one unit increase in perceived threat, there is a .24 increase in behavioral intention, b = .24, t(938) = 7.02, and p < .00. At average levels of hostile ageism, for a one unit increase in perceived threat, there is a .11 increase in behavioral intention, b = .11, t(938) = 4.11, and p < .00. At high levels of hostile ageism, there is no significant relationship between perceived threat and behavioral intention, b = −.02, t(938) = −.52, and p = .60.
Figure 3.
Graph of the interaction between perceived threat and hostile ageism on behavioral intent.
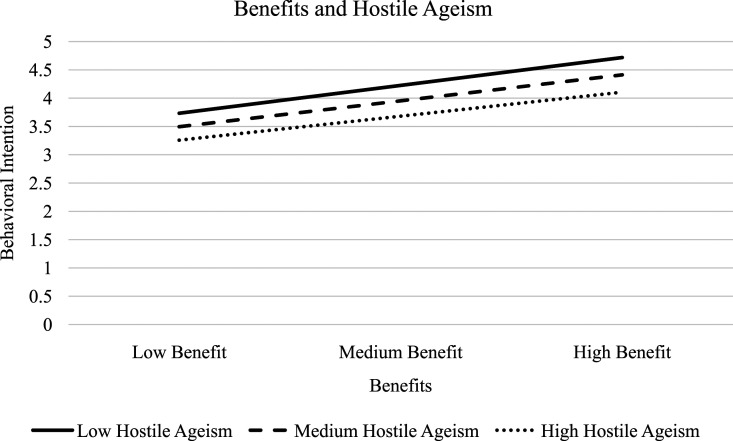
Benefits
In the equation examining whether hostile ageism moderated the effects of benefits on behavioral intent, an omnibus effect was detected [F(6, 939) = 280.99, p = .00, and R2= .64]. Hostile ageism [b = −.17 and p = .00], and benefits [b = .64 and p = .00], and the interaction [b = −.03 and p = .03] all uniquely contributed to the overall effect on behavioral intent (see Figure 4 for the interaction of benefits and hostile ageism). By examining the conditional effects, it was found that at low levels of hostile ageism, for a one unit increase in benefits, there is a .69 increase in behavioral intention, b = .69, t(939) = 21.17, and p < .00. At average levels of hostile ageism, for a one unit increase in benefits, there is a .64 increase in behavioral intention, b = .64, t(939) = 29.54, and p < .00. At high levels of hostile ageism, for a one unit increase in benefits, there is a .60 decrease in behavioral intention, b = .60, t(939) = 20.53, and p < .00.
Figure 4.
Graph of the interaction between benefits and hostile ageism on behavioral intent.
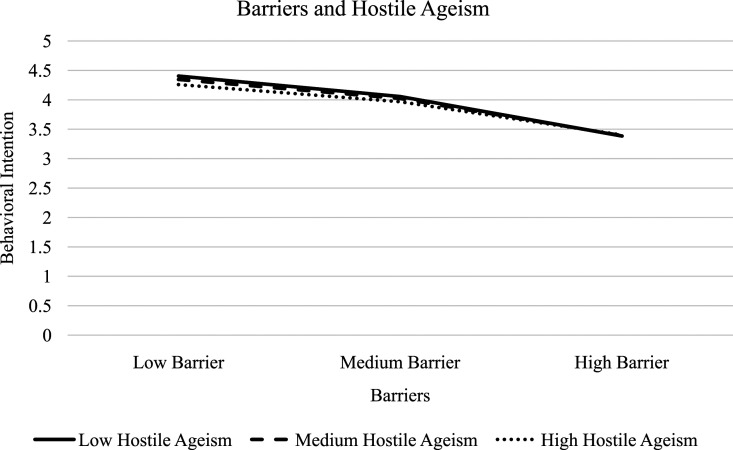
Barriers
In the equation examining whether hostile ageism moderated the effects of barriers on behavioral intent, an omnibus effect was detected [F(6, 939) = 222.63, p = .00, and R2= .59]. Hostile ageism [b = −.03 and p = .01], barriers [b = −.58 and p = .00], and the interaction [b = .03 and p = .01] uniquely contributed to the overall effect on behavioral intent (see Figure 5 for the interaction of barriers and hostile ageism). By examining the conditional effects, it was found that at low levels of hostile ageism, for a one unit increase in barriers, there is a −.63 decrease in behavioral intention, b = −.63, t(939) = −17.75, and p < .00. At average levels of hostile ageism, for a one unit increase in barriers, there is a −.58 decrease in behavioral intention, b = −.58, t(939) = −23.76, and p < .00. At high levels of hostile ageism, for a one unit increase in barriers, there is a −.53 decrease in behavioral intention, b = −.53, t(939) = −23.12, and p < .00.
Figure 5.
Graph of the interaction between barriers and hostile ageism on behavioral intent.
Age as a Modifier
Because ageism may vary by age (Cherry et al., 2016; Kite et al., 2005), age was explored in the moderation analyses to determine its impact on the relation of the health belief variables, ageism, and behavioral intention. Moderated moderation analyses were conducted to determine the effects of age. When age was added as a moderator, two analyses showed significance.
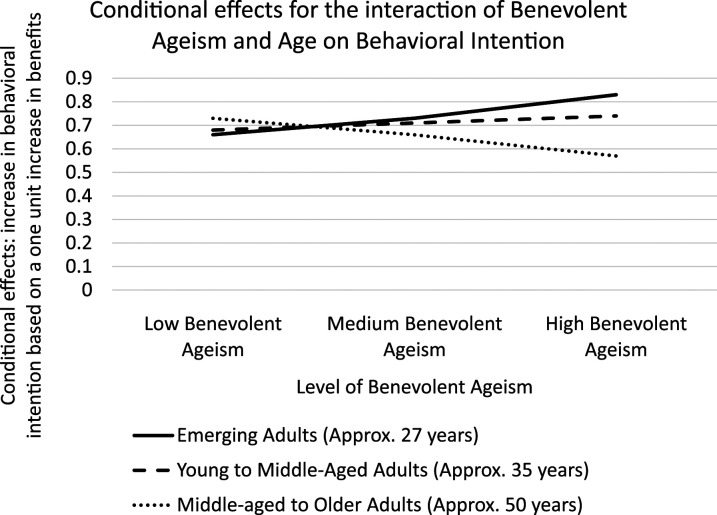
Benefits
In the equation examining whether age moderated benevolent ageism’s moderation on the relation of benefits on behavioral intent, an omnibus effect was detected [F(9, 934) = 161.18, p = .00, and R2= .61]. Benevolent ageism [b = −.15 and p = .00], benefits [b = .70 and p = .00], age [b = −.003 and p = .04], and the three-way interaction of benevolent ageism, age, and benefits [b = −.005 and p = .00] all uniquely contributed to the overall effect on behavioral intent. By examining the conditional effects, it was found that all conditional effects were significant [p = .00]. For a one unit increase in benefits, all conditional effects show an increase in behavioral intention, see Figure 6 for condition effects.
Figure 6.
Graph of the conditional effects of the interaction between benevolent ageism and age, as a function of the change in benefits, on behavioral intention.
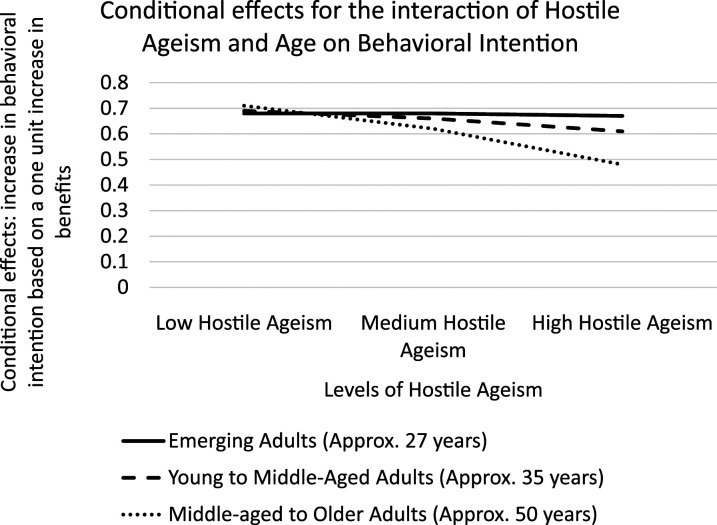
In the equation examining whether age moderated hostile ageism’s moderation on the relation of benefits on behavioral intent, an omnibus effect was detected [F(9, 936) = 189.79, p = .00, and R2= .65]. Hostile ageism [b = −.17 and p = .00], benefits [b = .64 and p = .00], age [b = −.004 and p = .01], the two-way interaction of hostile ageism and benefits [b = −.03, p = .04], and the three-way interaction of hostile ageism, age, and benefits [b = −.003, and p = .02] all uniquely contributed to the overall effect on behavioral intent. By examining the conditional effects, it was found that all conditional effects were significant [p = .00]. For a one unit increase in benefits, all conditional effects show an increase in behavioral intention, see Figure 7 for condition effects.
Figure 7.
Graph of the conditional effects of the interaction between hostile ageism and age, as a function of the change in benefits, on behavioral intention.
Discussion
In the current study, the HBM was used to organize the factors influencing intention to socially distance among a convenience sample of adults at the rise of the COVID-19 curve in the United States. In each of our models, perceived threat (a combination of severity and susceptibility), perceived benefits, and perceived barriers independently contributed to behavioral intentions with the strongest associations between behavioral beliefs (benefits and barriers) and intention. Age, gender, and race/ethnicity were controlled for in all models. Although not the focus of the current investigation, sociodemographic similarities and differences are important for contextualization. We found that as age increased so did behavioral intentions, also that identifying as female and white corresponded with higher intention to social distance. These findings are consistent with previous research (e.g., Durham et al., 2012).
Given the initial presentation of COVID-19 as a primary concern for older adults, we also wanted to examine the moderating influence of ageism, separating the influence of hostile and benevolent forms. Independently, hostile and benevolent ageism were correlated with behavioral intentions such that as endorsement of ageist beliefs increased, behavior intentions decreased. In interaction with the HBM variables, ageism modified the relationship to behavioral intention for both perceived threat and barriers, but only hostile ageism moderated the influence of benefits. Recognizing the centrality of age to ageism, we explored further to determine whether age altered these relations. A significant three-way interaction was identified for both benevolent and hostile ageism with age and perceived benefits on behavioral intentions. These findings are discussed below.
Health Belief Model and Intention to Social Distance
Consistent with previous research, the variables of perceived threat (a combination of susceptibility and severity) and perceived benefits and barriers of the preventative behavior related directly to intention to social distance. Specifically, higher levels of perceived benefits were related with higher intention to social distance and higher perceived barriers with a lower intention to social distance. Perceived threat, while not significantly related to behavioral intentions at the bivariate level, was significant in the multivariate models with age, gender, and race controlled; greater perceived threat was associated with greater intention to social distance. These findings are consistent with the HBM theoretical model in general (e.g., Rosenstock et al., 1988). Studies focusing on prevention behaviors during a pandemic, mainly vaccinations, also had similar findings (e.g., Ashbaugh et al., 2013; Fall et al., 2018; Huang et al., 2012; Kan & Zhang, 2018). In comparison to the other known study to focus on applying HBM to understanding social distancing (“crowd avoidance,” Durham et al., 2012), both perceived benefits and perceived severity were significantly related in univariate analyses, and only perceived benefits in multivariate models. Therefore, the current study provides additional support for the utility of the HBM as a guiding framework for understanding behavioral intentions during a pandemic. Specifically, perceived barriers and benefits should be the target of interventions trying to influence social distancing, given the strong and consistent associations observed.
Ageism and Intention to Social Distance
Although the two forms of ageism were highly, positively correlated (as has been reported in other studies looking at hostile and benevolent forms of prejudice (see Cary et al., 2017; Glick & Fiske, 2001)), we examined the influence of these forms of ageism as moderators, independently, with the rationalization that the mechanisms underlying these beliefs might translate differently to behavior. In light of initial communication emphasizing COVID-19 as particularly problematic for older adults and recommendations emphasizing the need for this particular population to social distance, someone high on hostile ageism may not see the necessity to bear the personal burden to social distance if they are not personally at risk, and the behavior is only to protect older adults. Someone high on benevolent ageism may be more likely to social distance, already viewing older adults as vulnerable and in need of protection.
As a predictor
At the bivariate level, both hostile and benevolent ageism related to behavioral intentions negatively such that higher levels of ageism corresponded with lower expressed intentions to social distance with hostile ageism showing the stronger association. It may be possible at the point of data collection that people were not aware of the impact that their own social distancing behavior could have on others (Qazi et al., 2020). Those high on benevolent ageism may stress the importance of older adults’ social distancing but may not see how their own behavior influences older adults. The question was not specific enough to inquire about social distancing from particular populations, so it could be possible that those high on benevolent ageism may be more likely to social distance from older adults than in general.
In multivariate models with other predictors of intention to social distance, benevolent ageism remained a significant predictor of behavioral intentions. In the model including perceived barriers of social distancing, the direction of the relationship changed such that those high on benevolent ageism reported greater intention to social distance. For multivariate models containing hostile ageism and other predictors of intention to social distance, hostile ageism was a significant predictor in all models. These findings indicate that both benevolent and hostile ageism are contributing unique variance in predicting likelihood to social distance during a pandemic. While our intention was to examine ageism as a moderator, the implications of ageism contributing uniquely to behavioral intentions are important in recognizing the pervasive ways in which ageist beliefs may influence behavior within a multigenerational world (Nelson, 2016; Swift et al., 2017).
As modifying factor
A goal of the current study was to understand how ageist beliefs interact with other known predictors of behavioral intentions. The results indicate that both hostile and benevolent ageism modify the relationships for perceived threat and perceived barriers with behavioral intentions, and only hostile ageism interacts with perceived benefits. The lack of moderating effects of benevolent ageism on the relationship between perceived benefits and social distancing is likely due to the weaker relationship between benevolent ageism and behavioral intention; although in this model, benevolent ageism still contributed uniquely, albeit comparatively more weakly to intention to social distance.
Specifically, low and even moderate levels of ageism (hostile or benevolent) interacted with perceived threat in such a way that intention to social distance was still in the intended direction, albeit moving from low to average ageism dampened the influence of perceived threat on intention to social distance. We would have expected this effect to also be seen at high levels of ageism, but there was not a significant moderation effect at this level; regardless of level of perceived threat, those high in ageism did not differ significantly in their intention to social distance. Given that older adults and those with preexisting health conditions are at greater risk for complications from COVID-19 (Rahman & Jahan, 2020), this may reflect a desire to psychologically distance oneself as an older, and thus, an even more vulnerable individual. Internalization is one of the identified mechanisms that disrupt healthy aging (Levy, 2009; Swift et al., 2017). More research is needed to clarify this finding.
The significant moderation effect of hostile ageism with perceived benefits produces an interpretable effect. With increases in hostile ageism, the association between perceived benefits and intention to social distance is dampened. Although the effect is small, the implications are that hostile ageism produces a climate wherein individuals may be less willing to engage even in perceived beneficial behaviors if it is for the purpose of aiding or protecting the aging population. More research is needed to investigate whether these underlying motivations exist at either a conscious or unconscious level.
The moderating effect of ageism with perceived barriers is somewhat confusing. Increasing levels of ageism, regardless of whether benevolent or hostile, dampen the influence of perceived barriers on likelihood to social distance. This dampening effect makes sense for benevolent ageism in light of the originally posed mechanism. A high perception of barriers in combination with a high degree of benevolent ageism would result in a higher intention to social distance compared to someone with the same barrier perception, but a lower degree of benevolent ageism; benevolent ageism in the former case may be working to counteract those barriers. But seeing this same trend emerge for hostile ageism, wherein both high perception of barriers and high hostile ageism would be expected to correspond with the lowest intention to social distance, but instead resulted in the opposite, is difficult to interpret. One possible interpretation may reflect the high degree of correspondence between perceived barriers and both forms of ageism (r = .58 for benevolent and r = .68 for hostile). This may also be reflective of an underlying negative response style or characteristic, such as stress reactivity or negative emotionality (Allan et al., 2014), or internalization of a stigmatized identity as a barrier in response to both a pandemic and positive, healthy aging (Swift et al., 2017).
The covariates age, gender, and race were all comparably related to these variables, suggesting that there may be important group differences to explore in future research. It is important to note that in both models, the interactions are relatively small compared to the large influence of perceived barriers on likelihood to social distance and thus should be interpreted cautiously.
Age as a modifying influence on ageism
Given that ageism varies between age-groups both in terms of perception and impact (Cherry et al., 2016; Kite et al., 2005), we investigated the possibility of a moderated moderation with age altering the influence of ageism on the relation between HBM variables and intention to social distance. In our study, age was negatively related to both forms of ageism such that younger age corresponded with higher ageism. In the exploratory moderated moderation analyses, age was entered as a continuous moderator. The three-way interactions for each form of ageism with age and perceived benefits were the only significant findings to emerge from this exploration. The lack of significant findings with perceived barriers and threat suggest that the influence of age on ageism is consistent across age-groups as it relates to those variables.
Interestingly, it is through the incorporation of age as a modifier that benevolent ageism emerges as a modifying influence on the connection between perceived benefits and intention to social distance. Given that benevolent ageism is focused on seeing older adults as vulnerable and in need of care, it stands to reason that age may be how this form of ageism corresponds to perceptions and behavior. The conditional effects reveal that for younger participants, and to a lesser extent, middle-aged participants, each unit increase in benevolent ageism amplifies the influence of perceived benefits on intention to social distance. The same is not true for older participants, who for each increase in benevolent ageism experienced a dampening of the influence of perceived benefits on intention to social distance. This result may be a reflection of internalization and either embodying the stereotype (e.g., seeing oneself as vulnerable and resigned to ones’ fate; Levy, 2009) or subsequent distancing of oneself from being included in the older and vulnerable category (e.g., “I’m not like those other old people”; Zebrowitz & Montepare, 2000), whereas for younger participants this, may act as a motivation and may in itself be a perceived benefit (e.g., “I’m protecting my older loved ones by social distancing”).
For hostile ageism, the same pattern of dampening is observed for the older participants in the study where for each unit increase in ageism, the influence of perceived benefits on intention to social distance is dampened. This dampening influence appears for the middle-aged group, but to a lesser extent. Importantly, among the youngest participants, hostile ageism, regardless of level, has little to no impact on the relationship between perceived benefits and intention to social distance.
The implication of these exploratory results taken collectively is that age largely does not influence how ageism impacts the relation between HBM variables and intention to social distance. If anything, benevolent ageism among those in early adulthood and younger may amplify the perceived benefits of social distancing and increase intention. This is consistent with the idea of ageism producing a sense of intergenerational solidarity (Ayalon et al., 2020). High levels of ageism, whether benevolent or hostile, may be most problematic for adults nearing later life. More research is needed to determine the extent to which not just age, but age identity within this demographic group makes a difference. Furthermore, ageism may be experienced at the intersection of other identities (i.e., older black man), leading to further distinctions.
Limitations
Despite the strengths of the current study as a theoretically grounded, timely investigation of factors influencing behavioral intentions during a pandemic, there are limitations. The sample represents a snapshot of a single point, early in the pandemic in the United States. As Durham et al., 2012 expounded, the health belief variables are subject to change over the course of time and in response to changing contextual elements. Therefore, the application of these findings may not be applicable to other points throughout the pandemic. Additionally, generalization is limited by the sample, a convenience sample of adult participants on Amazon’s Mechanical Turk. Although MTurk has been demonstrated to be a quality source (see Follmer et al., 2017), caution is advised as to who is represented on MTurk. While the demographics of the current sample mimics patterns in the United States in terms of racial and ethnic breakdowns, the sample is more heavily weighted with male, young, and highly educated individuals. This also complicates the interpretation of our exploration of age as a moderator of ageism as some of these effects may be stronger at more advanced ages, despite the fact that people encounter unfair treatment based on age across the life span (Kite et al., 2005). The average age of our oldest age level in our analyses was around the age of 50, demonstrating the younger collective age of our sample. Furthermore, the characteristics of people with regular internet access, registered on a crowdsourcing website may be inherently different than the average person.
Measurement of health belief variables is a consistent problem as measures needed to be developed specific to the behavior (Champion & Skinner, 2008). Although an improvement over commonly employed single-item measures and tailored after other validated instruments representing the underlying constructs, the measures used in the current study were not validated with an independent sample. In addition to potential issues with the health belief measures, the ageism scales were global assessments of ageism and not specific to COVID-19. The analysis approach also focused on isolating the modifying role of ageism and therefore did not account for the interaction between HBM variables as has been suggested by others (Jones et al., 2015). Last, other variables that were not included in the current study, such as self-efficacy and cues to action (e.g., exposure to ageist messages on social media), may influence intention to social distance.
Conclusion
Research has shown that ageism disrupts healthy aging in a variety of ways (e.g., Swift et al., 2017). The current study results, based on a convenience sample of mostly younger and middle-aged adults in the United States, demonstrate how hostile and benevolent ageism, related but distinct constructs, may influence health beliefs and behavioral intentions during the early stages of a pandemic. The biggest takeaway points to perceived benefits and barriers as the strongest predictors of intention to social distance among the variables we studied; however, the small way in which ageism influences behavioral intentions directly and in altering the influence of other factors, alone and in interaction with age, may be important to consider. Future research may do well to look at these factors specifically within older adult populations, wherein the internalization of ageism may be a more prominent factor, or among those who provide care to older adults. Furthermore, with initial reports of COVID-19 focusing primarily on the vulnerabilities of older adults, it is essential to note that both forms of ageism negatively related to intention to social distance and thus do a disservice in portraying older adults as a homogenous segment of the population. Last, awareness and careful messaging are advised when calling attention to the needs of an already stigmatized population group, given the possibility that existing beliefs act as a lens through which new information is interpreted and decisions about ones’ own role are determined.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research was funded through faculty start-up funds provided by the first author’s institution: Northern Kentucky University, College of Arts and Sciences.
ORCID iD
Allyson S. Graf https://orcid.org/0000-0001-5282-830X
References
- Allan L. J., Johnson J. A., Emerson S. D. (2014). The role of individual difference variables in ageism. Personality and Individual Differences, 59, 32-37. doi: 10.1016/j.paid.2013.10.027 [DOI] [Google Scholar]
- Ashbaugh A. R., Herbert C. F., Saimon E., Azoulay N., Olivera-Figueroa L., Brunet A. (2013). The decision to vaccinate or not during the H1N1 pandemic: Selecting the lesser of two evils?. PLoS One, 8(3), e58852. doi: 10.1371/journal.pone.0058852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayalon L. (2020). There is nothing new under the sun: Ageism and intergenerational tension in the age of the COVID-19 outbreak. International Psychogeriatrics, 32(10), 1221-1224. doi: 10.1017/S1041610220000575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayalon L., Chasteen A., Diehl M., Levy B., Neupert S. D., Rothermund K., Tesch-Römer C., Wahl H. W. (2020). Aging in times of the COVID-19 pandemic: Avoiding ageism and fostering intergenerational solidarity. The Journals of Gerontology: Series B, 72(2), e49-e52. doi: 10.1093/geronb/gbaa051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker M. H., Radius S. M., Rosenstock I. M., Drachman R. H., Schuberth K. C., Teets K. C. (1978). Compliance with a medical regimen for asthma: A test of the health belief model. Public Health Reports, 93(3), 268-277. [PMC free article] [PubMed] [Google Scholar]
- Brooke J., Jackson D. (2020). Older people and COVID‐19: Isolation, risk and ageism. Journal of Clinical Nursing, 29(13-14), 2044-2046. doi: 10.1111/jocn.15274 [DOI] [PubMed] [Google Scholar]
- Butler R. N. (1969). Age-ism: Another form of bigotry. The Gerontologist, 9(4, Part 1), 243-246. doi: 10.1093/geront/9.4_Part_1.243 [DOI] [PubMed] [Google Scholar]
- Cary L. A., Chasteen A. L., Remedios J. (2017). The ambivalent ageism scale: Developing and validating a scale to measure benevolent and hostile ageism. The Gerontologist, 57(2), e27-e36. doi: 10.1093/geront/gnw118 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2020). Coronavirus disease 2019 (COVID-19): Situation summary. https://www.cdc.gov/coronavirus/2019-ncov/casesupdates/summary.html
- Cesari M., Proietti M. (2020). COVID-19 in Italy: Ageism and decision making in a pandemic. Journal of the American Medical Directors Association, 21(5), 576-577. doi: 10.1016/j.jamda.2020.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Champion V. L. (1993). Instrument refinement for breast cancer screening behaviors. Nursing Research, 42(3), 139-143. doi: 10.1097/00006199-199305000-00003 [DOI] [PubMed] [Google Scholar]
- Champion V. L., Skinner C. S. (2008). The health belief model. Health Behavior and Health Education: Theory, Research, and Practice, 4, 45-65. [Google Scholar]
- Cherry K. E., Brigman S., Lyons B. A., Blanchard B., Walker E. J., Smitherman E. A. (2016). Self-reported ageism across the lifespan: Role of aging knowledge. The International Journal of Aging and Human Development, 83(4), 366-380. doi: 10.1177/0091415016657562 [DOI] [PubMed] [Google Scholar]
- Colenda C. C., Reynolds C. F., Applegate W. B., Sloane P. D., Zimmerman S., Newman A. B., Meeks S., Ouslander J. G. (2020). COVID-19 pandemic and ageism: A call for humanitarian care. The American Journal of Geriatric Psychiatry, 28(8), 805-807. doi: 10.1016/j.jagp.2020.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durham D. P., Casman E. A., Albert S. M. (2012). Deriving behavior model parameters from survey data: Self‐protective behavior adoption during the 2009–2010 influenza a (H1N1) pandemic. Risk Analysis: An International Journal, 32(12), 2020-2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’cruz M., Banerjee D. (2020). ‘An invisible human rights crisis’: The marginalization of older adults during the COVID-19 pandemic – An advocacy review. Psychiatry Research, 292, 113369. doi: 10.1016/j.psychres.2020.113369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdfeld E., Faul F., Buchner A. (1996). Gpower: A general power analysis program. Behavior Research Methods, Instruments, & Computers, 28, 1-11. doi: 10.3758/BF03203630 [DOI] [Google Scholar]
- Fall E., Izaute M., Chakroun-Baggioni N. (2018). How can the health belief model and self-determination theory predict both influenza vaccination and vaccination intention? A longitudinal study among university students. Psychology & Health, 33(6), 746-764. doi: 10.1080/08870446.2017.1401623 [DOI] [PubMed] [Google Scholar]
- Follmer D. J., Sperling R. A., Suen H. K. (2017). The role of MTurk in education research: Advantages, issues, and future directions. Educational Researcher, 46(6), 329-334. doi: 10.3102/0013189X17725519 [DOI] [Google Scholar]
- Fraser S., Lagacé M., Bongué B., Ndeye N., Guyot J., Bechard L., Bergeron C. D. (2020). Ageism and COVID-19: What does our society’s response say about us?. Age and Ageing, 49(5), 692-695. doi: 10.1093/ageing/afaa097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick P., Fiske S. T. (2001). An ambivalent alliance: Hostile and benevolent sexism as complementary justifications for gender inequality. American psychologist, 56(2), 109-118. doi: 10.1037/0003-066X.56.2.109 [DOI] [PubMed] [Google Scholar]
- Gostin L.O., Wiley L.F. (2020). Governmental public health powers during the COVID-19 pandemic: Stay-at-home orders, business closures, and travel restrictions. JAMA, 323(21), 2137-2138. doi: 10.1001/jama.2020.5460 [DOI] [PubMed] [Google Scholar]
- Gözüm S., Aydin I. (2004). Validation evidence for Turkish adaptation of champion's health belief model scales. Cancer nursing, 27(6), 491-498. [PubMed] [Google Scholar]
- Hayes A. F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper]. Retrieved fromhttp://www.afhayes.com/ public/process2012.pdf
- Hochbaum G. M.Public participation in medical screening programs: A socio-psychological study. Washington, D.C: U.S. Dept. of Health, Education, and Welfare, 1958. [Google Scholar]
- Huang J. H., Miao Y. Y., Kuo P. C. (2012). Pandemic influenza H1N1 vaccination intention: Psychosocial determinants and implications from a national survey, Taiwan. The European Journal of Public Health, 22(6), 796-801. doi: 10.1093/eurpub/ckr167 [DOI] [PubMed] [Google Scholar]
- Hummert M. L. (1990). Multiple stereotypes of elderly and young adults: A comparison of structure and evaluations. Psychology and Aging, 5, 182-193. doi: 10.1037/0882-7974.5.2.182 [DOI] [PubMed] [Google Scholar]
- Janz N. K., Becker M. H. (1984). The health belief model: A decade later. Health Education Quarterly, 11(1), 1-47. doi: 10.1177/109019818401100101 [DOI] [PubMed] [Google Scholar]
- Jimenez‐Sotomayor M. R., Gomez‐Moreno C., Soto‐Perez‐de‐Celis E. (2020). Coronavirus, ageism, and twitter: An evaluation of tweets about older adults and COVID‐19. Journal of the American Geriatrics Society, 68(8), 1661-1665. doi: 10.1111/jgs.16508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones C. L., Jensen J.D., Scherr C. L., Brown N.R., Christy K., Weaver J. (2015). The health belief model as an explanatory framework in communication research: Exploring parallel, serial, and moderated mediation. Health Communication, 30, 566-576. doi: 10.1080/10410236.2013.873363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones C. J., Smith H., Llewellyn C. (2014). Evaluating the effectiveness of health belief model interventions in improving adherence: A systematic review. Health Psychology Review, 8(3), 253-269. doi: 10.1080/17437199.2013.802623 [DOI] [PubMed] [Google Scholar]
- Kan T., Zhang J. (2018). Factors influencing seasonal influenza vaccination behaviour among elderly people: A systematic review. Public Health, 156, 67-78. doi: 10.1016/j.puhe.2017.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kite M. E., Stockdale G. D., Whitley B. E., Johnson B. T. (2005). Attitudes toward younger and older adults: An updated meta‐analytic review. Journal of Social Issues, 61(2), 241-266. https://psycnet.apa.org/doi/10.1111/j.1540-4560.2005.00404.x [Google Scholar]
- Lamont R. A., Swift H. J., Abrams D. (2015). A review and meta-analysis of age-based stereotype threat: Negative stereotypes, not facts, do the damage. Psychology and Aging, 30(1), 180-193. doi: 10.1037/a0038586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Couteur D. G., Anderson R. M., Newman A. B. (2020). COVID-19 through the lens of gerontology. The Journals of Gerontology: Series A, 75(9), e119-e120. doi: 10.1093/gerona/glaa077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B. (2009). Stereotype embodiment: A psychosocial approach to aging. Current Directions in Psychological Science, 18(6), 332-336. doi: 10.1111/j.1467-8721.2009.01662.x 10.1111/j.1467-8721.2009.01662.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow-Howell N., Galucia N., Swinford E. (2020) Recovering from the COVID-19 pandemic: A focus on older adults. Journal of Aging & Social Policy, 32, 526-535. doi: 10.1080/08959420.2020.1759758 [DOI] [PubMed] [Google Scholar]
- Myers L. B., Goodwin R. (2011). Determinants of adults' intention to vaccinate against pandemic swine flu. BMC Public Health, 11(1), 15. doi: 10.1186/1471-2458-11-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson T. D. (2016). The age of ageism. Journal of Social Issues, 72(1), 191-198. doi: 10.1111/josi.12162 [DOI] [Google Scholar]
- North M. S., Fiske S. T. (2013). Subtyping ageism: Policy issues in succession and consumption. Social Issues and Policy Review, 7(1), 36-57. doi: 10.111/j.1751-2409.2012.01042.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick J. H., Nehrkorn A. M., Knepple Carney A. (2016). Crowd sourcing in aging research: Some cautions and best practices. Adult Development and Aging News; (Division 20 Newsletter). http://www.apadivisions.org/division-20/publications/newsletters/adultdevelopment/2016/04/crowd-sourcing.aspx [Google Scholar]
- Qazi A., Qazi J., Naseer K., Zeeshan M., Hardaker G., Maitama J.Z., Haruna K. (2020). Analyzing situational awareness through public opinion to predict adoption of social distancing amid pandemic COVID-19. Journal of Medical Virology, 92, 849-855. doi: 10.1002/jmv.25840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A., Jahan Y. (2020). Defining a ‘risk group’ and ageism in the era of COVID-19. Journal of Loss and Trauma, 25(8), 1-4. doi: 10.1080/15325024.2020.1757993 [DOI] [Google Scholar]
- Rosenstock I. M., Strecher V. J., Becker M. H. (1988). Social learning theory and the health belief model. Health Education Quarterly, 15(2), 175-183. doi: 10.1177/109019818801500203 [DOI] [PubMed] [Google Scholar]
- Setbon M., Raude J. (2010). Factors in vaccination intention against the pandemic influenza A/H1N1. European Journal of Public Health, 20(5), 490-494. doi: 10.1093/eurpub/ckq054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swift H. J., Abrams D., Lamont R. A., Drury L. (2017). The risks of ageism model: How ageism and negative attitudes toward age can be a barrier to active aging. Social Issues and Policy Review, 11(1), 195-231. doi: 10.1111/sipr.12031 [DOI] [Google Scholar]
- Tanner-Smith E. E., Brown T. N. (2010). Evaluating the health belief model: A critical review of studies predicting mammographic and pap screening. Social Theory & Health, 8(1), 95-125. doi: 10.1057/sth.2009.23 [DOI] [Google Scholar]
- Vernon S. W., Myers R. E., Tilley B. C. (1997). Development and validation of an instrument to measure factors related to colorectal cancer screening adherence. Cancer Epidemiology and Prevention Biomarkers, 6(10), 825-832. [PubMed] [Google Scholar]
- Zebrowitz L. A., Montepare J. M. (2000). Too young, too old: Stigmatizing adolescents and the elderly. In Heatherton T., Kleck R., Hull J.G., Hebl M. (Eds.), Stigma (pp. 334-373). New York: Guilford. [Google Scholar]