Abstract
Background
The short form, 17-item version of the Pediatric Symptom Checklist-Youth Self-Report (PSC-17-Y) is a validated measure that assesses psychosocial problems overall (OVR) and in 3 major psychopathological domains (internalizing, externalizing, and attention-deficit/hyperactivity disorder), taking 5-10 min to complete. Prior research has established sound psychometric properties of the PSC-17-Y for English speakers.
Objective
This study extends psychometric evidence for the acceptability of the PSC-17-Y in a large sample of Spanish adolescents, providing proof of its reliability and structure, convergent and discriminant validity, and longitudinal and gender invariance.
Methods
Data were collected on 5430 adolescents, aged 12-18 years, who filled out the PSC-17-Y twice during 2018-2019 (7-month interval). We calculated the Cronbach alpha and the McDonald omega coefficients to test reliability, the Pearson correlation for convergent (distress) and criterion validity (well-being, quality of life, and socioemotional skills), confirmatory factor analysis (CFA) for structure validity, and multigroup and longitudinal measurement invariance analysis for longitudinal and gender stability.
Results
Within structural analysis for the PSC-17-Y, CFA supported a correlated 3-factor solution, which was also invariant longitudinally and across gender. All 3 subscales showed evidence of reliability, with coefficients near or above .70. Moreover, scores of PSC-17-Y subscales were positively related with convergent measures and negatively related with criterion measures. Normative data for the PSC-17-Y are presented in the form of percentiles (75th and 90th).
Conclusions
This work provides the first evidence of the reliability and validity of the Spanish version of the PSC-17-Y administered over the internet to assess mental health problems among adolescents, maintaining the same domains as the long version.
Keywords: PSC-17-Y, psychometric properties, screening, mental problems, adolescents, adolescent health, adolescent medicine, psychiatry, psychology, psychosocial issues
Introduction
According to Polanczyk et al [1], the most common mental health disorders among children and adolescents include anxiety or depression, behavioral disorders, and attention-deficit/hyperactivity disorder (ADHD). Emotional and behavioral symptoms at the subclinical level raise the risk of subsequent development of mental disorders [2]. Moreover, the COVID-19 pandemic has provoked a considerable increase in mental health problems among children and adolescents [3-5].
National and international policies and strategies globally recommend that young people attending primary care should be routinely screened for psychosocial problems [6]. Despite this, such screening occurs in less than 50% of primary care visits of adolescents, meaning that more than half of adolescent mental health problems go undetected [7,8]. Although several screening tools exist for psychosocial problems in young people, most cover a single domain [9] and can be time consuming to administer and interpret [10]. Primary care clinicians can often be unsure of which screening tools are appropriate for their clinical context. In addition, many tools rely on the provider having the skills, knowledge, expertise, and experience to initiate screening, interpret results, and provide appropriate interventions [8]. Providers often describe a lack of resources in terms of the availability of time, appropriate tools, training, and experience in youth health [11].
A recent review of “Self-Report Rating Scales to Guide Measurement-Based Care in Child and Adolescent Psychiatry” [12] highlights that the Pediatric Symptom Checklist (PSC) is 1 of the most widely used measures to screen psychosocial problems in primary care units and school settings. This statement is supported for all parent and youth reports and for long and short forms (parent- and youth-reported long form [PSC-35]; parent- and youth-reported short form [PSC-17]) [13-23].
The short form, 17-item version of the PSC-Y (PSC-17-Y) [16] is used to assess self-reported general psychosocial functioning among youth above 11 years old, taking only 5-10 min to be completed, and is statistically equivalent to the short form of the parent version (PSC-17) [16] and to the longer youth report form (PSC-35-Y [19-21]).
Three studies of the parent report PSC-17 (Gardner et al [16,17] and Murphy et al [18]) have confirmed the existence of the 3 original subscales for internalizing (INT) symptoms, externalizing (EXT) symptoms, and ADHD symptoms (ATT) and provided evidence of the reliability of the overall (OVR) scale. Two studies with the youth-reported short form have been published. On the one hand, Bergman et al [22] found that the PSC-17-Y is equivalent to the parent-reported form of the PSC-17, indicating that a 3-factor short form with 17 items meets the criteria for scalar invariance across gender. On the other hand, Parker et al [23] examined the screening validity of the PSC-17-Y in a child welfare population. Youth with any lifetime mental health diagnosis scored significantly higher on the PSC ATT and INT subscales. The ATT, INT, and OVR subscale scores were significantly correlated with psychosis, depression, and anxiety disorder scores. ADHD was associated with ATT, OVR, and EXT scores. Only bipolar disorder was weakly associated with PSC subscale scores (EXT and OVR). This study provides support for the convergent and discriminant validity of the PSC-17-Y.
Despite PSC-17-Y’s potential, however, there is limited evidence of some of its relevant psychometric properties (eg, longitudinal measurement invariance and other reliability coefficients different from the Cronbach alpha [α]), and to the best of our knowledge from the scientific literature review, none of these psychometric analyses are in languages other than English (ie, none on Spanish populations).
Thus, this work aimed to extend the psychometric evidence for the acceptability of the PSC-17-Y in a large sample of Spanish adolescents, providing different sources of reliability and validity. This research could facilitate the use of the PSC -17-Y in more contexts and for more possible applications in youth mental health settings. Overall, we expected that the PSC-17-Y would show that it is a valid and reliable ultrabrief screening measure that can be administered over the internet to detect mental health problems in Spanish adolescents.
Methods
Sample
The final sample consisted of 5430 adolescents (2769 [51%] females) at time 0 and 2117 (1109 [52.4%] females) at time 1 (approximately 7 months later). The participants were enrolled in Spanish secondary education grades, equivalent to US middle and high school, from grades 7 (12-13 years) to 12 (17-18 years). The average age of the sample at time 0 was 14.17 years (SD 1.50) and of the sample that participated at time 0 and time 1 was 13.99 years (SD 1.39).
Measures
PSC-17-Y
The PSC-17-Y [16] consists of 17 items and 3 factors to assess 3 types of problems: INT symptoms (ie, depression and anxiety), EXT symptoms (ie, disruptive behavior), and ATT, as well as an OVR score. The Spanish version of the PSC-17-Y was developed in accordance with the guidelines of the International Test Commission [24], using an iterative translation method that began with several independent translations. The item translations were then reviewed by a joint committee comprising translators with knowledge of the Spanish language and culture and specialists in the field of assessment who analyzed the adequacy of the adapted version. To be sure that adolescents properly understood all items, interviews asking about the comprehension of the items were conducted. In addition, in 2018, we had conversations with colleagues who had worked on the translation of the PSC for parents in Chile [25,26] in order to obtain an adequate cross-cultural adaptation into the European Spanish language of the PSC-17-Y.
Social-Emotional Distress Survey-Secondary
The Social-Emotional Distress Survey-Secondary (SEDS-S) [27] is a 10-item behavioral screening questionnaire designed to measure INT distress. The reliability of the 1-factor total scale was α=.91. In their study, Dowdy et al [27] found a significant positive association of the SEDS-S distress factor with symptoms of anxiety and depression and a significant negative association with life satisfaction and strength scores.
Mental Health Continuum-Short Form
The Mental Health Continuum-Short Form (MHC-SF) [28] is the reduced version of the MHC Long Form. This measure provides self-reported well-being, divided into 3 subfactors: psychological (6 items), emotional (3 items) and social well-being (5 items). In this study, we used the Spanish version of the MHC-SF recently adapted by our team. The MHC-SF has received psychometric support for use with adolescents across many different countries, including Spain [29,30], showing excellent internal consistency (Cronbach α>.80) and discriminant validity in adolescents.
KIDSCREEN-10 Index
The KIDSCREEN-10 Index [30] is a unidimensional scale that measures health-related quality of life (HRQoL) in healthy and chronically ill children and adolescents. It was developed to specifically identify children at risk in terms of subjective health and suggest appropriate early interventions. The instrument provides an overall HRQoL index covering the physical, psychological, and social facets of the HRQoL. Internal consistency values (Cronbach α) reach .82, and test-retest reliability within 2 weeks reaches .55 [31].
Social-Emotional Health Survey-Secondary
The Social-Emotional Health Survey-Secondary (SEHS-S) [32] was developed to measure the components of the covitality latent construct among youth. We used the Spanish version of the SEHS-S, which is appropriate for adolescents aged 12-18 years [33]. The SEHS-S includes 36 items for the assessment of core psychosocial assets based on a higher-order model comprising 12 first-order, grouped into 4 second-order, latent traits (3 each) and a higher-order general factor (covitality). The first domain, called belief-in-self, measures self-efficacy, self-awareness, and persistence. The domain belief-in-others comprises school support, peer support, and family support. The domain emotional competence considers emotion regulation, empathy, and behavioral self-control. Engaged living, which is the final domain, comprises 3 subscales: gratitude, zest, and optimism.
Procedure
This research used a non-experimental, transversal/longitudinal, quantitative, and descriptive-correlational design [34,35]. The UMH Project Evaluation Committee approved the study (reference no. DPS.JPR.02.17). Once the project was approved, quota sampling was carried out in 2 areas of southeastern Spain: the province of Alicante (PA) belonging to the Valencian Community, and the Autonomous Community of the Region of Murcia (RM), making a random selection of secondary schools based on ownership (public/nonpublic schools) and regional geographical areas (9 areas in PA and 21 in RM). After 100 schools were contacted, 13 from PA and 21 from RM agreed to participate, resulting in a total of 34 secondary schools (22 [65.2%] public and 12 [34.8%] nonpublic schools; 30 [87%] secular and 4 [13%] catholic schools).
Once the schools agreed to participate, signed informed consent was requested in writing from the parents/legal guardians of the adolescent participants and from the adolescents themselves, accepting participation in the research. The data collection was carried out in the schools and supervised by the research staff in person. The self-reporting assessment protocol was individually applied through the online survey tool LimeSurvey (LimeSurvey GmbH, Hamburg, Germany). Participation was voluntary, and the adolescents did not receive any incentive for their collaboration, while each school received a feedback report, including results by class group.
Data Analysis
All analyses were conducted using IBM SPSS Statistics version 25 and Mplus 8.4 (Muthén & Muthén). Confirmatory factor analysis (CFA) was conducted to test the structural validity. Figure 1 represents the correlated 3-factor solution tested. We used a diagonally weighted least squares means and variance adjusted (WLSMV) model estimator due to a number of alternative responses and the nonnormality distribution [36]. We tested the model’s goodness of fit using the comparative fit index (CFI), the Tucker-Lewis index (TLI), and the root-mean-square error of approximation (RMSEA). A CFI of >0.90 and a TLI of >0.95 indicate an acceptable and an optimal fit, respectively [37], and RMSEA values of ≤0.10 indicate an acceptable fit [38].
Figure 1.
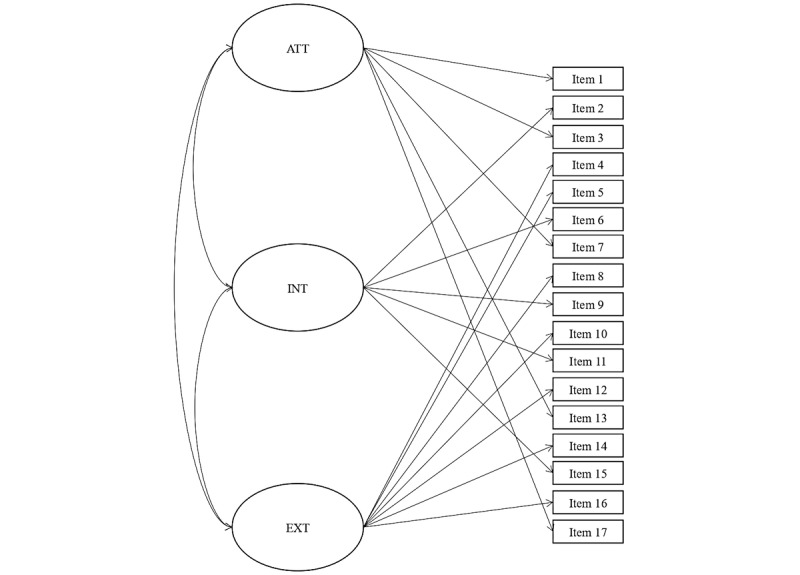
Visual representation of the 17-item, 3-factor solution of the PSC-17-Y. ATT: attention-deficit/hyperactivity disorder symptoms; EXT: externalizing; INT: internalizing; PSC-17-Y: Pediatric Symptom Checklist-Youth Self-Report.
Later, we tested whether the PSC-17-Y exhibits an invariant structure across gender and across time through longitudinal and multigroup measurement invariance analysis. In particular, 3 levels of invariance were tested: (1) configural (test whether all items load on the proposed factor), (2) metric (test whether item-factor loadings are similar across groups), and (3) scalar (test whether unstandardized item thresholds are similar across groups). In addition, within longitudinal measurement, invariance residuals covariances between the same item over time (eg, time 0 with time 1) were included. Thus, to indicate a significant decrement in fit when testing for measurement invariance, we used model comparison criteria of ΔCFI/ΔTFI ≥ 0.01 (ie, a decrease indicating the worst fit) [39] and ΔRMSEA ≥ 0.015 (ie, an increase indicating the worst fit) [40].
When there is scalar measurement invariance, the comparison of factor means across groups is permissible [41]. Consequently, we calculated gender differences. We also estimated the Cohen d index (standardized mean difference), which allows evaluating the effect size (ES) of the obtained differences [42].
The Cronbach α and the McDonald omega (ω) [43] were used to estimate the internal consistency of the PSC-17-Y since the McDonald ω is a better estimator of reliability than the Cronbach α [44].
Convergent and criterion validity was evaluated by calculating the correlation coefficients between the scores on the PSC-17-Y and different, well-established measures. Specifically, we tested the convergent validity with measures of distress (SEDS-S) and criterion validity with measures of well-being, QoL, and socioemotional skills (MHC-SF, KIDSCREEN-10 Index, SEHS-S). The Cohen criteria were used to estimate the ES of the correlations [42,45].
Finally, normative data for the PSC-17-Y were presented in the form of percentiles (75th and 90th). We also calculated the cut-off point of 15 for OVR, 5 for INT symptoms, 7 for EXT symptoms, and 7 for ATT, as proposed by Gardner et al [16,17], because these scores have not received evidence-based support in Spanish adolescents.
As the sample size determination for psychometric validation studies lacks clear recommendations [46], we determined the required sample size by allocating several observations 5-10 times greater than the variables [47]. Accordingly, the sample size needed ranged between 85 and 170 participants based on the number of items in the PSC-17-Y. Furthermore, according to the subject-to-item ratio method, a sample size of ≥1000 to perform exploratory factor analysis (EFA) or CFA would be excellent [46].
Results
Confirmatory Factor Analysis and Measurement Invariance
Findings of CFA and measurement invariance over time and across gender groups are summarized in Table 1. Since item 13 (“Me cuesta mucho cansarme”/“Acts as if driven by a motor”) had a low loading at the ATT subscale (0.127), we also tested the 16-item model, which slightly improved the fit. An optimal fit index was observed for both the 17- and 16-item models, with loadings from 0.348 (item 5) to 0.858 (item 6) and from 0.346 (item 5) to 0.859 (item 6), respectively. Longitudinal and multigroup measurement invariance was found for the 17- and 16-item models, which means that the structure, loadings, and intercepts of the PSC-17-Y were invariant over time and across gender groups. Although the 16-item version was slightly stronger than the 17-item version, we concluded that the minimal improvement in accuracy was less important than being able to use the 17-item model, which is the internationally recognized version and facilitates comparisons with other studies. For this reason, subsequent analyses were performed with a 17-item version.
Table 1.
Goodness of fit for baseline models and measurement invariance of the 3-factor solution.
| Number | Items, n | Overall goodness of fit | Comparative goodness of fit | |||||||
|
|
|
χ2a (df) | CFIb | TLIc | RMSEAd (90% CI) | Model comparison | ΔCFI | ΔTLI | ΔRMSEA | |
| Baseline model | ||||||||||
|
|
1 | 17 | 1462.63 (116) | 0.961 | 0.954 | 0.046 (0.044-0.048) | —e | — | — | — |
|
|
2 | 16 | 1105.35 (101) | 0.970 | 0.965 | 0.043 (0.041-0.045) | 1 vs 2 | 0.009 | 0.010 | –0.003 |
| Longitudinal measurement configural invariance | ||||||||||
|
|
3 | 17 | 2814.41 (496) | 0.956 | 0.950 | 0.029 (0 .028-0.030) | — | — | — | — |
|
|
4 | 16 | 1957.05 (433) | 0.970 | 0.966 | 0.025 (0 .024-0.027) | — | — | — | — |
| Longitudinal measurement metric invariance | ||||||||||
|
|
5 | 17 | 2395.55 (505) | 0.964 | 0.960 | 0.026 (0 .025-0.027) | 3 vs 5 | 0.008 | 0.010 | –0.003 |
|
|
6 | 16 | 1845.45 (443) | 0.973 | 0.969 | 0.024 (0 .023-0.025) | 4 vs 6 | 0.003 | 0.003 | –0.001 |
| Longitudinal measurement scalar invariance | ||||||||||
|
|
7 | 17 | 2538.15 (522) | 0.961 | 0.958 | 0.027 (0 .026-0.028) | 5 vs 7 | –0.003 | –0.002 | 0.001 |
|
|
8 | 16 | 1969.06 (459) | 0.970 | 0.968 | 0.025 (0 .024-0.026) | 6 vs 8 | –0.003 | –0.001 | 0.001 |
| Gender configural invariance | ||||||||||
|
|
9 | 17 | 2573.15 (990) | 0.968 | 0.964 | 0.024 (0 .023-0.025) | — | — | — | — |
|
|
10 | 16 | 2110.28 (866) | 0.974 | 0.971 | 0.023 (0 .022-0.024) | — | — | — | — |
| Gender metric invariance | ||||||||||
|
|
11 | 17 | 2777.51 (1018) | 0.965 | 0.961 | 0.025 (0 .024-0.026) | 9 vs 11 | –0.003 | –0.003 | 0.001 |
|
|
12 | 16 | 2342.64 (892) | 0.970 | 0.967 | 0.024 (0 .023-0.026) | 10 vs 12 | –0.004 | –0.004 | –0.001 |
| Gender scalar invariance | ||||||||||
|
|
13 | 17 | 3068.45 (1046) | 0.959 | 0.956 | 0.027 (0 .026-0.028) | 11 vs 13 | –0.006 | –0.005 | 0.002 |
|
|
14 | 16 | 2460.40 (918) | 0.968 | 0.966 | 0.025 (0 .024-0.026) | 12 vs 14 | –0.002 | –0.001 | 0.001 |
aP<.001.
bCFI: comparative fit index.
cTLI: Tucker-Lewis index.
dRMSEA: root-mean-square error of approximation.
eNot applicable.
The correlation matrix of the items can be seen in Table 2.
Table 2.
Correlation matrix of the items.
| Items | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 |
| 1 | —a | — | — | — | — | — | — | — | — | — | — | — | — | — | — | — |
| 2 | 0.15 | — | — | — | — | — | — | — | — | — | — | — | — | — | — | — |
| 3 | 0.28 | 0.33 | — | — | — | — | — | — | — | — | — | — | — | — | — | — |
| 4 | 0.14 | 0.16 | 0.19 | — | — | — | — | — | — | — | — | — | — | — | — | — |
| 5 | 0.15 | 0.10 | 0.15 | 0.32 | — | — | — | — | — | — | — | — | — | — | — | — |
| 6 | 0.10 | 0.73 | 0.33 | 0.25 | 0.17 | — | — | — | — | — | — | — | — | — | — | — |
| 7 | 0.29 | 0.38 | 0.49 | 0.20 | 0.20 | 0.41 | — | — | — | — | — | — | — | — | — | — |
| 8 | 0.21 | 0.39 | 0.28 | 0.24 | 0.16 | 0.36 | 0.32 | — | — | — | — | — | — | — | — | — |
| 9 | 0.13 | 0.52 | 0.27 | 0.16 | 0.08 | 0.56 | 0.32 | 0.33 | — | — | — | — | — | — | — | — |
| 10 | 0.18 | 0.30 | 0.25 | 0.36 | 0.22 | 0.32 | 0.30 | 0.35 | 0.31 | — | — | — | — | — | — | — |
| 11 | 0.13 | 0.58 | 0.25 | 0.18 | 0.155 | 0.60 | 0.35 | 0.28 | 0.45 | 0.28 | — | — | — | — | — | — |
| 12 | 0.31 | 0.30 | 0.40 | 0.29 | 0.227 | 0.32 | 0.41 | 0.44 | 0.23 | 0.38 | 0.27 | — | — | — | — | — |
| 13 | 0.22 | –0.04 | 0.05 | 0.07 | 0.105 | 0.06 | 0.06 | 0.06 | –0.01 | 0.05 | –0.01 | 0.16 | — | — | — | — |
| 14 | 0.26 | 0.24 | 0.34 | 0.31 | 0.256 | 0.24 | 0.33 | 0.41 | 0.20 | 0.41 | 0.19 | 0.48 | 0.14 | — | — | — |
| 15 | 0.13 | 0.42 | 0.20 | 0.07 | 0.026 | 0.41 | 0.30 | 0.23 | 0.47 | 0.18 | 0.36 | 0.17 | 0.07 | 0.14 | — | — |
| 16 | .15 | .24 | .24 | .29 | .174 | .28 | .25 | .37 | .13 | .34 | .16 | .43 | .11 | .42 | .07 | — |
| 17 | 0.33 | 0.31 | 0.576 | 0.178 | 0.187 | 0.34 | 0.69 | 0.33 | 0.27 | 0.28 | 0.28 | 0.44 | 0.07 | 0.37 | 0.26 | 0.30 |
aNot applicable.
As can be seen in Tables 3 and 4, the reliability coefficients for all measures ranged from .64 to .76 (McDonald ω). Regarding gender differences among total scores, females showed significantly higher scores on general social-emotional distress (d=0.34) and INT (d=0.42) scales than males, with a small-to-medium ES. Concerning the differences in the EXT scale, males showed more symptoms of EXT problems than females, with a small ES (d=0.12). Although the scores for well-being and socioemotional competencies were lower in females than in males, the ESs were low (d ranged from 0.08 to 0.15). Finally, males showed higher HRQoL levels than females, with an ES of 0.35.
Table 3.
Descriptive analysis for males and females and reliability coefficients of the PSC-17-Ya.
| PSC-17-Y Subscales | Cronbach α (95% CI) | Interitem correlations | McDonald ω (95% CI) | Score, mean (SD) | Effect size (d) | |||||
|
|
Female | Male | Mean | Min | Max | Female | Male | Female (x) | Male (y) | d = x – y (P value) |
| ATTb | .61 (0.59-0.63) |
.63 (0.61-0.65) |
0.306 | 0.050 | 0.686 | .65 (0.63-0.67) |
.64 (0.62-0.66) |
4.45 (1.98) |
4.46 (2.07) |
0.01 (.76) |
| INTc symptoms | .76 (0.75-0.78) |
.73 (0.71-0.74) |
0.510 | 0.412 | 0.730 | .76 (0.75-0.78) |
.72 (0.70-0.74) |
3.74 (2.37) |
2.79 (2.17) |
0.42 (<.001) |
| EXTd symptoms | .65 (0.63-0.67) |
.67 (0.65-0.68) |
0.327 | 0.161 | 0.348 | .66 (0.64-0.68) |
.67 (0.65-0.69) |
2.54 (2.07) |
2.80 (2.15) |
–0.12 (<.001) |
aPSC-17-Y: short form of the Pediatric Symptom Checklist-Youth Self-Report.
bATT: attention-deficit/hyperactivity disorder symptoms.
cINT: internalizing.
dEXT: externalizing.
Table 4.
Descriptive analysis for males and females and reliability coefficients of study measures.
| Measures | Cronbach α (95% CI) | McDonald ω (95% CI) | Score, mean (SD) | Effect size (d) | |||
|
|
Female | Male | Female | Male | Female (x) | Male (y) | d = x – y (P value) |
| Emotional | .80 (0.79-0.81) | .77 (0.75-0.78) | .82 (0.80- 0.83) | .79 (0.77-0.81) | 13.84 (3.29) | 14.31 (3.06) | –0.15 (<.001) |
| Social | .85 (0.84-0.86) | .83 (0.82-0.84) | .86 (0.85-0.86) | .83 (0.82-0.84) | 19.67 (5.60) | 20.36 (5.50) | –0.12 (<.001) |
| Psychological | .86 (0.86-0.87) | .86 (0.85-0.87) | .91 (0.85-0.87) | .86 (0.85-0.87) | 28.04 (5.74) | 28.51 (5.58) | –0.08 (.003) |
| HRQoLa | .86 (0.85-0.86) | .83 (0.82-0.84) | .86 (0.85-0.86) | .83 (0.82-0.84) | 37.39 (7.36) | 39.81 (6.44) | –0.35 (<.001) |
| Socioemotional skills | .91 (0.91-0.92) | .90 (0.90-0.91) | .91 (0.91-0.92) | .90 (0.90-0.91) | 110.69 (14.72) | 112.28 (14.04) | –0.12 (<.001) |
aHRQoL: health-related quality of life.
According to Table 5, the intercorrelation between the PSC-17-Y subscales was moderate, indicating that this measure is composed of 3 differentiated and mutually associated factors. Regarding the relationship between PSC-17-Y subscales and the remaining measures, the highest positive correlations were between the INT subscale and the measure of distress (large ES), while the association of the ATT and EXT subscales with distress was medium. Similarly, the correlation was higher (and negative) between the INT subscale and the HRQoL (large ES) than between different types of well-being and socioemotional competencies (moderate to large). However, the correlation between ATT and measures of well-being, socioemotional competencies, and the HRQoL was significant and negative, with a small-to-medium magnitude. Finally, the EXT subscale presented a small-to-medium association with the different positive measures.
Table 5.
Correlations between the PSC-17-Ya, distress, and well-being measures.
| PSC-17-Y Subscales – Measures | ATTb | INTc symptoms |
EXTd symptoms |
Distress | Emotional well-being |
Social well-being |
Psychological well-being |
HRQoLe | Socioemotional skills |
| ATT | 1 | —f | — | — | — | — | — | — | — |
| INT symptoms | 0.35g | 1 | — | — | — | — | — | — | — |
| EXT symptoms | 0.46g | 0.36g | 1 | — | — | — | — | — | — |
| Distress | 0.35g | 0.67g | 0.35g | 1 | — | — | — | — | — |
| Emotional well-being | –0.19g | –0.51g | –0.24g | –0.44g | 1 | — | — | — | — |
| Social well-being | –0.21g | –0.46g | –0.26g | –0.38g | 0.65g | 1 | — | — | — |
| Psychological well-being | –0.23g | –0.50g | –0.31g | –0.42g | 0.70g | 0.72g | 1 | — | — |
| HRQoL | –0.30g | –0.67g | –0.34g | –0.60g | 0.66g | 0.63g | 0.72g | 1 | — |
| Socioemotional skills | –0.31g | –0.45g | –0.41g | –0.39g | 0.60g | 0.61g | 0.70g | 0.67g | 1 |
aPSC-17-Y: short form of the Pediatric Symptom Checklist-Youth Self-Report.
bATT: attention-deficit/hyperactivity disorder symptoms.
cINT: internalizing.
dEXT: externalizing.
eHRQoL: health-related quality of life.
fNot applicable.
gP<.001.
Concerning normative information for PSC-17-Y subscales, each subscale is scored by the sum of its items. The adolescent’s score on the scale can then be used to obtain the corresponding percentile score. The normative information for each of the 3 PSC-17-Y subscales and total scores for the whole sample are shown in Table 6. We also included percentile scores for PSC-17-Y OVR scores to facilitate international comparisons.
Table 6.
Normative information about PSC-17-Ya scales for adolescents (percentile scores); N=5430 (boys and girls 12-18 years old).
| Percentile | PSC-17-Y ATTb | PSC-17-Y INTc symptoms | PSC-17-Y EXTd symptoms | PSC-17-Y totale |
| 1 | 0 | 0 | 0 | 0 |
| 5 | 1 | 0 | 0 | 3 |
| 10 | 2 | 1 | 0 | 4 |
| 15 | 2 | 1 | 0 | 5 |
| 20 | 3 | 1 | 1 | 6 |
| 25 | 3 | 1 | 1 | 7 |
| 30 | 3 | 2 | 1 | 8 |
| 35 | 4 | 2 | 2 | 8 |
| 40 | 4 | 2 | 2 | 9 |
| 45 | 4 | 3 | 2 | 10 |
| 50 | 5 | 3 | 2 | 10 |
| 55 | 5 | 3 | 3 | 11 |
| 60 | 5 | 4 | 3 | 12 |
| 65 | 5 | 4 | 3 | 12 |
| 70 | 5 | 4 | 4 | 13 |
| 75 | 6 | 5 | 4 | 14 |
| 80 | 6 | 5 | 4 | 15 |
| 85 | 7 | 6 | 5 | 16 |
| 90 | 7 | 7 | 6 | 17 |
| 95 | 8 | 8 | 7 | 19 |
| 99 | 9 | 10 | 8 | 23 |
aPSC-17-Y: short form of the Pediatric Symptom Checklist-Youth Self-Report.
bATT: attention-deficit/hyperactivity disorder symptoms. Rating anchor: ATT=0-10 (5 items).
cINT: internalizing. Rating anchor: INT symptoms=0-10 (5 items).
dEXT: externalizing. Rating anchor: EXT symptoms=0-14 (7 items).
eRating anchor: total score=0-34 (17 items).
The values obtained in our study using the international cut-off point of 15 for OVR, 7 for ATT, 5 for INT symptoms, and 7 for EXT symptoms, as proposed by Gardner et al [24], were 20.7%, 15.1%, 29.7%, and 5.1%, respectively. The 90th percentile indicated that 11.6% of the sample scored above this cut-off point of 17 for OVR on the PSC-17-Y, 26.3% of the participants exceeded the 75th percentile for the PSC-17-Y total score. Regarding specific symptoms, 15.1%, 10.2%, and 10.6% of the participants scored above the 90th percentile on ATT, INT symptoms, and EXT symptoms, respectively. The data at the 75th percentile or quartile 1 indicated that 29.1%, 28.7%, and 32.0% of the participants exceeded the cut-off points for ATT, INT symptoms, and EXT symptoms, respectively.
Discussion
Principal Findings
This study aimed to delineate the psychometric properties of the PSC-17-Y in Spanish adolescents. As expected, this study found evidence of a 3-factor solution, as in the original English version, and also gave evidence of reliability and validity (structural, convergent, and criterion) to assess several psychopathology symptoms among adolescents. However, item 13 showed a lower loading (0.127) than the remaining items. This finding is consistent with Bergmann et al. [22], who validated the PSC-17-Y in English and reported a relatively low factor loading (0.233) for this item. Following the same logic as these authors, we maintained item 13 in the final set of items for the PSC-17-Y in Spanish, since it is important to keep the measure as simple as possible for respondents and clinicians to complete, score, and interpret and since the parent- and youth-reported short forms were identical except for this 1 item. We found that the inclusion of item 13 had a negligible impact on the psychometric properties of the PSC-17-Y in Spanish. As a result, we elected to add item 13 to the 16-item model and recommend a 17-item short form of the PSC-Y that uses the same 17 items on the same 3 subscales as the parent-reported PSC-17. Furthermore, we hypothesized that the problem with this item could be the wording and that future studies might review it to improve the saturation in the factor. The PSC-17-Y also showed an invariant structure across both genders, again consistent with Bergman et al [22].
Additionally, our study provided the first evidence, as far we know, for longitudinal invariance, indicating that the PSC-17-Y in Spanish adolescents is stable over time. This finding implies that it is reasonable to conclude that growth or development in observed scores over time can be attributed to actual development or changes in the construct under investigation, not measurement problems [48]. Further studies that replicate our study over more extended periods are, of course, needed.
Once gender and longitudinal invariance were tested, this study provided new evidence on gender-attributable differences in the PSC-Y scales. The gender differences found in this study were consistent with the overwhelming prior research establishing that females are more likely to express INT symptoms and males are more likely to express EXT symptoms [49-51]. Furthermore, the small ES found in these gender differences is also consistent with other ones, which highlighted the small magnitude of gender differences in INT problems among children and adolescents [52]. These findings suggest that gender differences should be considered when pediatric and mental health professionals interpret PSC-17-Y results. Furthermore, gender is a crucial variable in the relationship between INT symptoms and suicide among adolescents, increasing this risk in females [53].
Regarding reliability evidence, our study showed McDonald ω values between .64 and .76, which are slightly lower than those shown by previous studies. Gardner et al [16] reported high internal consistency (.79 for INT symptoms, .83 for EXT symptoms, and .83 for ATT), and in the same order, Bergmann et al [22], with 16 items, found consistency values of .81, .74, and .69, respectively. The lowest internal consistency value was ATT (.65 and .64 for females and males, respectively). The removal of item 13 could improve the internal consistency of the ATT subscale slightly to values of .70 and .71 for females and males, respectively but at the cost of losing the original 17-item structure of the questionnaire.
Concerning other sources of convergent and criterion validity evidence of the PSC-17-Y, all 3 subscales correlated positively with the measure of distress and negatively with well-being, HRQoL, and social-emotional competencies, indicating a higher correlation between PSC-17-Y INT problems and the remaining convergent and criterion validity measures. This finding is consistent with previous studies on the PSC-17-Y, such as Parker et al [23], who reported screening validity of the PSC-17-Y in terms of higher scores on the PSC ATT and INT subscales among youth with any lifetime mental health diagnosis, as well as that ATT and INT subscale scores (but not EXT) are significantly correlated with psychosis, depression, and anxiety disorders. Thus, both our study and Parker et al’s [23] provide support for the convergent and discriminant validity of the PSC-17-Y.
Finally, regarding percentile scores, score distributions showed a positive asymmetric distribution, but these normative data can help locate specific and general psychopathological problems among adolescents. Our rates would be suggestive of adolescents presenting scores compatible with mental health symptoms likely being in the clinical range. These data are equivalent to those reported in previous studies using different versions and cut-off scores for the PSC, PSC-17, and PSC-17-Y: 5%-25% of children were screened positive [15,16,54-56]. For example, a study using the 90th percentile score on the PSC found that 10.4% of children had problems on the OVR scale [54]. Additionally, the prevalence rates found in our study are consistent with wide international reviews on estimates of mental health prevalence among adolescents [1].
Limitations
The absence of an equivalent, well-established measure of INT, EXT, and ADHD measures; the absence of data on the area under the curve at optimal cut-off points in this study; and the sample's representativeness because we recruited the sample from the southeast of Spain exclusively were limitations of this study. In addition, there were only 2 waves of assessment in a short period of time (7 months), so it is recommended that future studies replicate the longitudinal invariance findings over longer intervals.
Conclusion
This study showed that the PSC-17-Y is a useful, reliable, and valid ultrabrief screening measure for detecting mental health problems in adolescents and can be administered over the internet. More specifically, this study provided evidence of the reliability and validity (structural and convergent-discriminant) of the Spanish version of the PSC-17-Y for adolescents.
Finally, these findings are significant for the scientific community. Therefore, this work has allowed us to extend the evidence of the validity of the PSC-17-Y to another language and country (Spain) in a large sample of adolescents, where scores were invariant over time irrespective of gender. This is a requirement that few instruments meet or for which evidence has been provided. All of this supports the reliability of the PSC-17-Y’s assessments and its use in clinical contexts, such as monitoring the development of symptomatology. The fact that the PSC-17-Y is a tool that is easy to administer is another support for its use in clinical contexts.
Having instruments such as the PSC-17-Y with established reliability meets an especially important need during COVID-19 times, which have been characterized by an increase in mental health problems among children and adolescents [3-5] and a possibly greater need for case identification and outcome measurement.
Lastly, the results also support the use of the PSC-17-Y in longitudinal research, for example, for the study of the temporal trajectories of psychopathology in children, facilitating, among other things, reliability in the evaluation of the effectiveness of treatments. In addition to its usefulness in research, the PSC-17-Y is an instrument with applicability in the clinical setting, specifically in both primary care and specialty mental health units, as a screening tool for mental health problems in children and adolescents that is valid for monitoring changes in functioning over time.
Acknowledgments
We would like to thank collaboration and support by the Dirección General de Atención a la Diversidad y Calidad Educativa de la Consejería de Educación, Juventud y Deportes de la Región de Murcia (General Department for Attention to Diversity and Educational Quality of the Regional Ministry of Education, Youth and Sports of the Region of Murcia, Spain) and the Secretaría Autonómica de Educación e lnvestigación de la Conselleria de Educación, Investigación, Cultura y Deporte de la Generalitat Valenciana (Regional Secretariat of Education and Research of the Regional Ministry of Education, Research, Culture and Sport of the Generalitat Valenciana, Spain), as well as to the educational centers, the authorization of parents and legal guardians, and especially the students, in the completion of the psychological assessment protocol, which made this study possible. We would also like to thank Javier Guzman (University of Desarrollo, Chile) for his assistance in adapting the PSC-17-Y into European Spanish.
This research was supported by a grant for I+D+i projects under award number PSI2017-88280-R (AEI/FEDER, UE) and 2 grants for Research Networks (PSI2015-70943-REDT and PSI2017-90650-REDT) from the Ministry of Economy, Industry and Competitiveness of the Spanish Government, as well as 3 predoctoral fellowships cofinanced by the European Social Fund and the Regional Ministry of Education, Research, Culture and Sport from the Generalitat Valenciana (RF: ACIF/2019/052; BM-A: ACIF/2019/055). VV-A is supported by a scholarship from the Universitat Jaume I (PREDOC/18/12); JMH and MM receive salary support from the Fuss Family Fund.
Abbreviations
- ADHD
attention deficit hyperactivity disorder
- ATT
attention deficit hyperactivity disorder symptoms
- CFA
confirmatory factor analysis
- CFI
comparative fit index
- ES
effect size
- EXT
externalizing
- HRQoL
health-related quality of life
- INT
internalizing
- MHC-SF
Mental Health Continuum-Short Form
- OVR
overall
- PSC-17-Y
Short Form of the Pediatric Symptom Checklist-Youth Self-Report
- PSC-17
Pediatric Symptom Checklist-Parent Version
- PSC
Pediatric Symptom Checklist
- RMSEA
root-mean-square error of approximation
- SEDS-S
Social-Emotional Distress Survey-Secondary
- SEHS-S
Social-Emotional Health Survey-Secondary
- TLI
Tucker-Lewis index
- WLSMV
weighted least squares means and variance adjusted
Footnotes
Authors' Contributions: JAP is principal investigator 1 of the funded project. He participated in the design of the psychological assessment protocol, collaborated in the conceptualization of this study by providing theoretical knowledge and professional and research background, and drafted the initial manuscript. VV-A participated in the conceptualization of the study by providing an analytical-methodological perspective, undertook the analysis of the data that made up the results of the study, and carried out a review of the statistical content. RF participated in the conceptualization of the study and in the design of the assessment protocol, coordinated and supervised the data collection, managed the database, reviewed the contents and terminology of the manuscript, and adapted its presentation format to the formatting requirements. BM-A participated in the design of the assessment protocol, coordinated and supervised the data collection, managed the online survey, collaborated in the selection and adaptation of the instruments, assisted in literature review tasks, and carried out a general review of contents. JCM is principal investigator 2 of the funded project. He participated in the design of the psychological assessment protocol, in the review and editing of the theoretical-methodological content, and in the adaptation of the manuscript to the formatting requirements. JH collaborated in the review of English editing and the final version of the manuscript. MM is the cocreator of the Pediatric Symptom Checklist (PSC). He consulted on the adaptation of the PSC into European Spanish and reviewed the final revision of the manuscript. All the authors approved the final manuscript, as submitted, and agree to be accountable for all aspects of the work.
Conflicts of Interest: None declared.
References
- 1.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015 Mar 03;56(3):345–65. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- 2.Fonseca-Pedrero E, Ortuño-Sierra J, Pérez-Albéniz A. Emotional and behavioural difficulties and prosocial behaviour in adolescents: a latent profile analysis. Rev Psiquiatr Salud Ment (Engl Ed) 2020;13(4):202–212. doi: 10.1016/j.rpsm.2020.01.002.S1888-9891(20)30021-5 [DOI] [PubMed] [Google Scholar]
- 3.Francisco R, Pedro M, Delvecchio E, Espada JP, Morales A, Mazzeschi C, Orgilés Mireia. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Front Psychiatry. 2020 Dec 3;11:570164. doi: 10.3389/fpsyt.2020.570164. doi: 10.3389/fpsyt.2020.570164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Espada J, Orgilés M, Piqueras J, Morales A. Good practices in child and adolescent psychological care before COVID-19. Clínica y Salud 2020. 2020 Jul 01;31(2):109–113. doi: 10.5093/clysa2020a14. [DOI] [Google Scholar]
- 5.Tamarit A, de la Barrera U, Monaco E, Schoeps K, Montoya-Castilla I. Psychological impact of COVID-19 pandemic in Spanish adolescents: risk and protective factors of emotional symptoms. Rev Psicol Clínica con Niños y Adolesc. 2020 Sep 01;7(3):73–80. doi: 10.21134/rpcna.2020.mon.2037. [DOI] [Google Scholar]
- 6.World Health Organization . Global Accelerated Action for the Health of Adolescents (AA-HA!): Guidance to Support Country Implementation. Geneva: WHO; 2017. p. 176. [Google Scholar]
- 7.Brown J, Wissow L. Screening to identify mental health problems in pediatric primary care: considerations for practice. Int J Psychiatry Med. 2010 May 6;40(1):1–19. doi: 10.2190/PM.40.1.a. [DOI] [PubMed] [Google Scholar]
- 8.Wissow L, Brown J, Fothergill K, Gadomski A, Hacker K, Salmon P, Zelkowitz R. Universal mental health screening in pediatric primary care: a systematic review. J Am Acad Child Adolesc Psychiatry. 2013 Nov;52(11):1134–1147.e23. doi: 10.1016/j.jaac.2013.08.013. http://europepmc.org/abstract/MED/24157388 .S0890-8567(13)00549-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Webb MJ, Kauer SD, Ozer EM, Haller DM, Sanci LA. Does screening for and intervening with multiple health compromising behaviours and mental health disorders amongst young people attending primary care improve health outcomes? A systematic review. BMC Fam Pract. 2016 Aug 04;17:104. doi: 10.1186/s12875-016-0504-1. https://bmcfampract.biomedcentral.com/articles/10.1186/s12875-016-0504-1 .10.1186/s12875-016-0504-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Connors E, Arora P, Blizzard A, Bower K, Coble K, Harrison J, Pruitt D, Steinberg J, Wissow L. When behavioral health concerns present in pediatric primary care: factors influencing provider decision-making. J Behav Health Serv Res. 2018 Jul;45(3):340–355. doi: 10.1007/s11414-017-9580-9. doi: 10.1007/s11414-017-9580-9.10.1007/s11414-017-9580-9 [DOI] [PubMed] [Google Scholar]
- 11.Ham P, Allen C. Adolescent health screening and counseling. Am Fam Physician. 2012 Dec 15;86(12):1109–16. https://www.aafp.org/link_out?pmid=23316983 .d10497 [PubMed] [Google Scholar]
- 12.Jeffrey J, Klomhaus A, Enenbach M, Lester P, Krishna R. Self-report rating scales to guide measurement-based care in child and adolescent psychiatry. Child Adolesc Psychiatr Clin N Am. 2020 Oct;29(4):601–629. doi: 10.1016/j.chc.2020.06.002.S1056-4993(20)30042-0 [DOI] [PubMed] [Google Scholar]
- 13.Jellinek M, Murphy JM. Psychosocial problems, screening, and the Pediatric Symptom Checklist. Dev Behav News. 1999 Jan;8(1):6–10. [Google Scholar]
- 14.Jellinek MS, Murphy JM, Burns BJ. Brief psychosocial screening in outpatient pediatric practice. J Pediatr. 1986 Aug 01;109(2):371–378. doi: 10.1016/s0022-3476(86)80408-5.S0022-3476(86)80408-5 [DOI] [PubMed] [Google Scholar]
- 15.Jellinek MS, Murphy JM, Robinson J, Feins A, Lamb S, Fenton T. Pediatric Symptom Checklist: screening school-age children for psychosocial dysfunction. J Pediatr. 1988 Feb;112(2):201–209. doi: 10.1016/s0022-3476(88)80056-8.S0022-3476(88)80056-8 [DOI] [PubMed] [Google Scholar]
- 16.Gardner W, Murphy M, Childs G, Kelleher K, Pagano M, Jellinek M, McInerny TK, Wasserman RC, Nutting P, Chiappetta L. The PSC-17: a brief pediatric symptom checklist with psychosocial problem subscales. A report from PROS and ASPN. Ambul Child Heal. 1999;5(3):225–236. [Google Scholar]
- 17.Gardner W, Lucas A, Kolko DJ, Campo JV. Comparison of the PSC-17 and alternative mental health screens in an at-risk primary care sample. J Am Acad Child Adolesc Psychiatry. 2007 May;46(5):611–618. doi: 10.1097/chi.0b013e318032384b. http://paperpile.com/b/BDqXMb/5aWh .S0890-8567(09)61720-2 [DOI] [PubMed] [Google Scholar]
- 18.Murphy JM, Bergmann P, Chiang C, Sturner R, Howard B, Abel MR, Jellinek M. The PSC-17: subscale scores, reliability, and factor structure in a new national sample. Pediatrics. 2016 Sep 12;138(3):e20160038. doi: 10.1542/peds.2016-0038. http://europepmc.org/abstract/MED/27519444 .peds.2016-0038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pagano ME, Cassidy LJ, Little M, Murphy JM, Jellinek AMS. Identifying psychosocial dysfunction in school-age children: The Pediatric Symptom Checklist as a self-report measure. Psychol Sch. 2000 Mar 01;37(2):91–106. doi: 10.1002/(SICI)1520-6807(200003)37:2<91::AID-PITS1>3.0.CO;2-3. http://europepmc.org/abstract/MED/22328794 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gall G, Pagano M, Desmond M, Perrin J, Murphy J. Utility of psychosocial screening at a school-based health center. J Sch Health. 2000 Sep 01;70(7):292–8. doi: 10.1111/j.1746-1561.2000.tb07254.x. http://europepmc.org/abstract/MED/10981284 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy JM, Nguyen T, Lucke C, Chiang C, Plasencia N, Jellinek M. Adolescent self-screening for mental health problems; demonstration of an internet-based approach. Acad Pediatr. 2018;18(1):59–65. doi: 10.1016/j.acap.2017.08.013.S1876-2859(17)30478-3 [DOI] [PubMed] [Google Scholar]
- 22.Bergmann P, Lucke C, Nguyen T, Jellinek M, Murphy JM. Identification and utility of a short form of the Pediatric Symptom Checklist-Youth Self-Report (PSC-17-Y) Eur J Psychol Assess. 2020 Jan;36(1):56–64. doi: 10.1027/1015-5759/a000486. [DOI] [Google Scholar]
- 23.Parker EM, Jacobson J, Pullmann MD, Kerns SEU. Identifying psychosocial problems among children and youth in the child welfare system using the PSC-17: exploring convergent and discriminant validity with multiple informants. Child Psychiatry Hum Dev. 2019 Feb;50(1):108–120. doi: 10.1007/s10578-018-0824-6.10.1007/s10578-018-0824-6 [DOI] [PubMed] [Google Scholar]
- 24.Muñiz J, Elosua P, Hambleton RK, International Test Commission International Test Commission Guidelines for test translation and adaptation: second edition. Psicothema. 2013;25(2):151–7. doi: 10.7334/psicothema2013.24.4093 [DOI] [PubMed] [Google Scholar]
- 25.Guzmán J, Kessler RC, Squicciarini AM, George M, Baer L, Canenguez KM, Abel MR, McCarthy A, Jellinek MS, Murphy JM. Evidence for the effectiveness of a national school-based mental health program in Chile. J Am Acad Child Adolesc Psychiatry. 2015 Oct;54(10):799–807.e1. doi: 10.1016/j.jaac.2015.07.005.S0890-8567(15)00481-5 [DOI] [PubMed] [Google Scholar]
- 26.Leiva L, Rojas R, Peña F, Vargas B, Scquicciarini A. Detectando las dificultades emocionales y conductuales en la escuela: validación de PSC-17. REV IBEROAM DIAGN EV. 2019 Jan;50(4):95–105. doi: 10.21865/ridep50.1.08. http://repositorioslatinoamericanos.uchile.cl/handle/2250/3031003#.YA5Wj90bQjk.mendeley . [DOI] [Google Scholar]
- 27.Dowdy E, Furlong MJ, Nylund-Gibson K, Moore S, Moffa K. Initial validation of the Social Emotional Distress Survey–Secondary to support complete mental health screening. Assess Eff Interv. 2018 Jan 05;43(4):241–248. doi: 10.1177/1534508417749871. [DOI] [Google Scholar]
- 28.Keyes CLM, Wissing M, Potgieter JP, Temane M, Kruger A, van Rooy S. Evaluation of the mental health continuum-short form (MHC-SF) in setswana-speaking South Africans. Clin Psychol Psychother. 2008;15(3):181–92. doi: 10.1002/cpp.572. [DOI] [PubMed] [Google Scholar]
- 29.Reinhardt M, Horváth Z, Morgan A, Kökönyei G. Well-being profiles in adolescence: psychometric properties and latent profile analysis of the mental health continuum model: a methodological study. Health Qual Life Outcomes. 2020 Apr 06;18(1):95. doi: 10.1186/s12955-020-01332-0. https://hqlo.biomedcentral.com/articles/10.1186/s12955-020-01332-0 .10.1186/s12955-020-01332-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Piqueras JA, Vidal-Arenas V, Falco R, Moreno-Amador B, Marzo JC, Keyes C. Validation of the Mental Health Continuum-Short Form (MHC-SF) for multidimensional assessment of subjective well-being in Spanish adolescents. Psicothema. 2021 Nov 18;:1–15. doi: 10.7334/psicothema2021.240. (forthcoming) [DOI] [PubMed] [Google Scholar]
- 31.Ravens-Sieberer U, Erhart M, Rajmil L, Herdman M, Auquier P, Bruil J, Power M, Duer W, Abel T, Czemy L, Mazur J, Czimbalmos A, Tountas Y, Hagquist C, Kilroe J, European KIDSCREEN Group Reliability, construct and criterion validity of the KIDSCREEN-10 score: a short measure for children and adolescents' well-being and health-related quality of life. Qual Life Res. 2010 Dec;19(10):1487–500. doi: 10.1007/s11136-010-9706-5. http://europepmc.org/abstract/MED/20668950 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Furlong MJ, You S, Renshaw TL, Smith DC, O’Malley MD. Preliminary development and validation of the Social and Emotional Health Survey for secondary school students. Soc Indic Res. 2013 Jun 27;117(3):1011–1032. doi: 10.1007/s11205-013-0373-0. [DOI] [Google Scholar]
- 33.Piqueras JA, Rodriguez-Jimenez T, Marzo JC, Rivera-Riquelme M, Martinez-Gonzalez AE, Falco R, Furlong MJ. Social Emotional Health Survey-Secondary (SEHS-S): a universal screening measure of social-emotional strengths for Spanish-speaking adolescents. Int J Environ Res Public Health. 2019 Dec 07;16(24):4982. doi: 10.3390/ijerph16244982. https://www.mdpi.com/resolver?pii=ijerph16244982 .ijerph16244982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ato M, López-García JJ, Benavente A. Un sistema de clasificación de los diseños de investigación en psicología. Anal Psicol. 2013 Oct 01;29(3):1038–1059. doi: 10.6018/analesps.29.3.178511. [DOI] [Google Scholar]
- 35.Montero I, León O. A guide for naming research studies in psychology. Int J Clin Heal Psychol. 2007;7(3):847–862. https://www.redalyc.org/articulo.oa?id=33770318 . [Google Scholar]
- 36.Li C. Confirmatory factor analysis with ordinal data: comparing robust maximum likelihood and diagonally weighted least squares. Behav Res Methods. 2016 Sep;48(3):936–49. doi: 10.3758/s13428-015-0619-7.10.3758/s13428-015-0619-7 [DOI] [PubMed] [Google Scholar]
- 37.Marsh HW, Hau K, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler's (1999) findings. Struct Equ Model. 2004 Jul;11(3):320–341. doi: 10.1207/s15328007sem1103_2. [DOI] [Google Scholar]
- 38.Weston R, Gore PA. A brief guide to structural equation modeling. Couns Psychol. 2016 Jun 30;34(5):719–751. doi: 10.1177/0011000006286345. [DOI] [Google Scholar]
- 39.Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model. 2002 Apr;9(2):233–255. doi: 10.1207/S15328007SEM0902_5. [DOI] [Google Scholar]
- 40.Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Model. 2007 Dec 05;14(3):464–504. doi: 10.1080/10705510701301834. [DOI] [Google Scholar]
- 41.Dimitrov D. Statistical Methods for Validation of Assessment Scale Data in Counseling and Related Fields. Alexandria, VA: American Counseling Association; 2012. [Google Scholar]
- 42.Cohen J. Statistical Power Analysis for the Behavioural Sciences. Hillside, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 43.McDonald R. Test Theory: A Unified Treatment. Hillside, NJ: Lawrence Erlbaum Associates; 1999. [Google Scholar]
- 44.Dunn TJ, Baguley T, Brunsden V. From alpha to omega: a practical solution to the pervasive problem of internal consistency estimation. Br J Psychol. 2014 Aug;105(3):399–412. doi: 10.1111/bjop.12046. [DOI] [PubMed] [Google Scholar]
- 45.Lipsey M, Wilson D. Practical Meta-Analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- 46.Anthoine E, Moret L, Regnault A, Sébille Véronique, Hardouin J. Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures. Health Qual Life Outcomes. 2014 Dec 09;12:176. doi: 10.1186/s12955-014-0176-2. https://hqlo.biomedcentral.com/articles/10.1186/s12955-014-0176-2 .s12955-014-0176-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tabachnick B, Fidell L, Ullman J. Using Multivariate Statistics (7th Ed.) Boston, MA: Pearson; 2019. [Google Scholar]
- 48.Millsap R, Cham H. Investigating factorial invariance in longitudinal data. In: Laursen B, Little TD, Card NA, editors. Handbook of Developmental Research Methods. New York, NY: Guilford Press; 2012. pp. 109–126. [Google Scholar]
- 49.Jacobson JH, Pullmann MD, Parker EM, Kerns SEU. Measurement based care in child welfare-involved children and youth: reliability and validity of the PSC-17. Child Psychiatry Hum Dev. 2019 Apr 27;50(2):332–345. doi: 10.1007/s10578-018-0845-1.10.1007/s10578-018-0845-1 [DOI] [PubMed] [Google Scholar]
- 50.Lewis AJ, Sae-Koew JH, Toumbourou JW, Rowland B. Gender differences in trajectories of depressive symptoms across childhood and adolescence: a multi-group growth mixture model. J Affect Disord. 2020 Jan 01;260:463–472. doi: 10.1016/j.jad.2019.09.027.S0165-0327(19)30790-6 [DOI] [PubMed] [Google Scholar]
- 51.Rocchino GH, Dever BV, Telesford A, Fletcher K. Internalizing and externalizing in adolescence: the roles of academic self-efficacy and gender. Psychol Sch. 2017 Aug 06;54(9):905–917. doi: 10.1002/pits.22045. [DOI] [Google Scholar]
- 52.Piqueras JA, Garcia-Olcina M, Rivera-Riquelme M, Martinez-Gonzalez AE, Cuijpers P. DetectaWeb-Distress Scale: a global and multidimensional web-based screener for emotional disorder symptoms in children and adolescents. Front Psychol. 2021 Feb 15;12:627604. doi: 10.3389/fpsyg.2021.627604. doi: 10.3389/fpsyg.2021.627604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Soto-Sanz V, Castellví P, Piqueras JA, Rodríguez-Marín J, Rodríguez-Jiménez T, Miranda-Mendizábal A, Parés-Badell O, Almenara J, Alonso I, Blasco MJ, Cebrià A, Gabilondo A, Gili M, Lagares C, Roca M, Alonso J. Internalizing and externalizing symptoms and suicidal behaviour in young people: a systematic review and meta-analysis of longitudinal studies. Acta Psychiatr Scand. 2019 Jul;140(1):5–19. doi: 10.1111/acps.13036. [DOI] [PubMed] [Google Scholar]
- 54.Bala G, Golubović S, Milutinović D, Katić R. Psychometric properties of the Pediatric Symptom Checklist in preschool children in Serbia. Med Glas (Zenica) 2012 Aug;9(2):356–62. [PubMed] [Google Scholar]
- 55.Reijneveld SA, Vogels AG, Hoekstra F, Crone MR. Use of the Pediatric Symptom Checklist for the detection of psychosocial problems in preventive child healthcare. BMC Public Health. 2006 Jul 27;6(1):197. doi: 10.1186/1471-2458-6-197. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-6-197 .1471-2458-6-197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lowenthal E, Lawler K, Harari N, Moamogwe L, Masunge J, Masedi M, Matome B, Seloilwe E, Jellinek M, Murphy M, Gross R. Validation of the Pediatric Symptom Checklist in HIV-infected Batswana. J Child Adolesc Ment Health. 2011 Jan 01;23(1):17–28. doi: 10.2989/17280583.2011.594245. http://europepmc.org/abstract/MED/22685483 . [DOI] [PMC free article] [PubMed] [Google Scholar]


