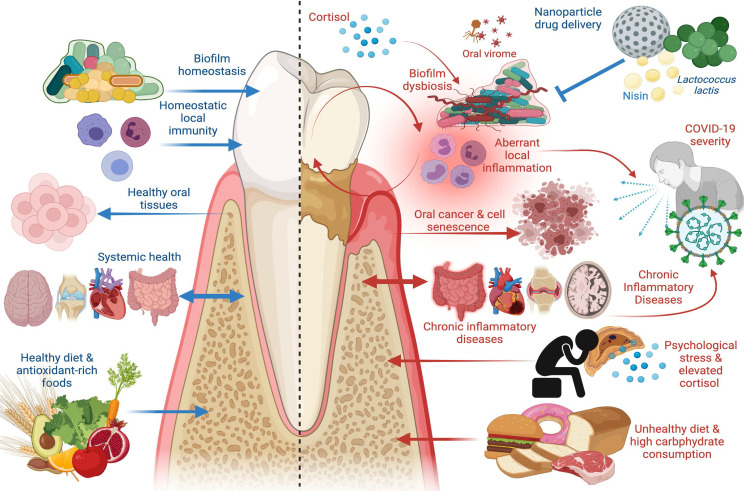
Figure 1.
The Good and the Bad in Periodontal Disease. Left panel: factors that promote periodontal health, including supra- and subgingival biofilm homeostasis, homeostatic immunity in gingival and periodontal tissues, healthy dietary constituents, and absence of chronic inflammatory disease at distant sites. Healthy periodontal tissues in turn reduce risk of oral carcinogenesis and bi-directionally affect systemic health such that chronic inflammatory disease risk is reduced. Right panel: factors that promote periodontal disease, including biofilm dysbiosis, uncontrolled gingival and periodontal inflammatory responses, psychological stress paralleled by elevated cortisol release, and unhealthy diets characterized by high carbohydrate consumption. Periodontal disease adversely affects oral tissue health and is a risk factor in oral carcinoma, induces cell senescence in healthy cells, promotes systemic inflammation, and is a risk factor in chronic inflammatory diseases including inflammatory bowel disease (IBD), cardiovascular disease, autoimmune conditions, and Alzheimer’s disease. Periodontal disease has emerged as a risk factor in COVID-19 severity and poor outcomes, as are other systemic chronic inflammatory diseases. New treatment modalities, such as oral probiotics including L. lactis and bacteriocins, such as nisin, that can be paired with nanoparticle drug delivery systems, have emerged as potential therapeutics to re-establish biofilm homeostasis and modulate aberrant inflammation. Image created with www.Biorender.com.