Abstract
The treatment of aortic valve disease in young patients is still a major clinical challenge, as the pre-eminent emphasis is on durability and long-term outcomes beyond 10 to 15 years, sometimes >20 to 30 years. The Ross procedure uses the autologous pulmonary valve as an aortic valve substitute and aims to improve valve durability while avoiding anticoagulation and therefore achieve a sustained long-term result with regard to survival, valve functionality, and quality of life. However, this procedure is technically demanding and only performed at a low frequency. Data investigating the Ross procedure are mostly limited to observational studies from single expert centers, while sufficient randomized data are almost completely lacking. Therefore, to create a clinically relevant database of this therapy, the multicenter Ross Registry was founded in 2001. New patients were included, follow-up of past patients continuously updated, and outcomes regularly reported. Throughout recent years, numerous analyses have been performed to characterize this patient population, surgical techniques, risk factors for morbidity and mortality, and most importantly survival outcomes. Currently, more than 2500 patients are included, and the long-term follow-up has reached >25 years in the very first patients who were included. In the most recent study, 2444 adult patients with a mean age of 44.1 ± 11.7 years were analyzed, and it showed that excellent mid-term survival is maintained after 25 years. In addition, the rate of reintervention was lower than reported in patients with xenografts and anticoagulation-related morbidity lower than reported in patients with mechanical valves. In the absence of robust randomized controlled trials, registry data are very important to monitor outcomes and mirror the quality of current practice. Therefore, the Ross Registry provides a unique and important data base regarding treatment of aortic valve disease in young patients.
Key Words: aortic stenosis, aortic regurgitation, pulmonary autograft, Ross procedure, SAVR, young patients

Schematic depiction of the Ross procedure and its surgical techniques.
Central Message.
Data regarding the Ross procedure are mostly limited to relatively small observational analyses. The Ross Registry provides a unique database to scientifically evaluate the Ross procedure.
See Commentary on page 401.
The Ross procedure uses the autologous pulmonic valve to replace the aortic valve (Figure 1, D) and is characterized by distinct differences compared with conventional prosthetic valves, as patients require no anticoagulation while showing excellent long-term outcomes with a relatively low risk for reoperation.1 In addition, past reports suggest that this procedure is associated with excellent hemodynamics, low incidence of thromboembolism/bleeding, and a good quality of life.1, 2, 3 Nevertheless, the Ross procedure is still not in widespread use compared with conventional prosthetic valve replacement.4 This is related to the complexity of the procedure but also to the lack of randomized data and therefore a solid recommendation for this procedure in guidelines.5,6 Concerns have been raised that a “1-valve disease” turns into a “2-valve procedure” and the risk for reintervention for the right ventricular outflow tract (RVOT). The controversy of this procedure has continued to this day. To fill this knowledge gap, the Ross Registry was initiated in 2001, which has become the largest one of this kind worldwide. This manuscript provides an overview of the history of the Ross Registry, its structure, important lessons learned from the past, and future directions.
Figure 1.
Schematic depiction of the Ross procedure and its surgical techniques. A, Subcoronary technique. B, Root-replacement technique. C, Root replacement + reinforcement technique. D, View of the aortic and pulmonic valve, both replaced by semilunar valves.
The Ross Registry—How Does It Work and Why Is It Important?
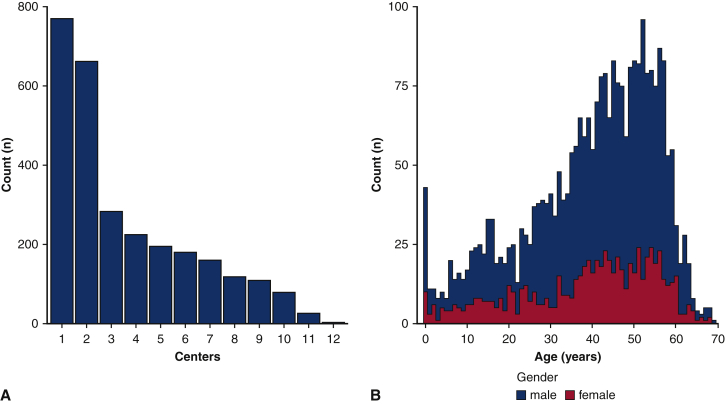
The Ross Registry was initiated in Lübeck, Germany, in 2001. Retrospective baseline data were obtained for patients treated between 1988 and 2001, and a prospective registry was begun in 2001. The Registry did not have any exclusion criteria, nor did it require a certain case load of the contributing center. However, we do require new centers to be actively performing Ross procedures to depict current practice. It was designed as an observational “all-comers” registry that aimed to continuously include patients of any age. The primary goal was to establish a multicenter registry to allow for longitudinal follow-up of these patients and regular critical scientific review of this procedure. This seemed very important, particularly due to the absence of robust randomized trials. To date, only 2 randomized controlled trials (RCTs) that included a treatment arm for the Ross procedure have been conducted.7,8 In addition, although RCTs are considered the best type of study design to investigate the role of a specific treatment modality, such trials also have significant limitations, such as low patient numbers, limited follow-up, and investigation of highly selected patient groups that are treated by a small number of centers. Large registry data can overcome these limitations and have become an inevitable data source to guide clinical decision-making, even in the presence of RCTs.9,10 Another advantage of a large multicenter registry is the evaluation of a procedure across different surgeons and centers. Although some reports have investigated the long-term results after the Ross procedure, these data are usually derived from single expert centers. For a specific and complex procedure such as the Ross procedure, it is particularly important to evaluate the feasibility and success rates not only in expert centers but in as many centers as possible to realistically depict clinical practice. To date, the registry has culminated data on almost 3000 patients from 12 European centers (8 from Germany, and 1 from the Netherlands, Ukraine, Czech Republic, and Austria) (Figure 2, A). The median age of the current registry population is 43 years (25th and 75th percentile: 30 and 52 years) (Figure 2, B). Therefore, the registry represents mostly “nonelderly adults” (n > 2400) but also includes >350 patients younger than 18 years of age.
Figure 2.
Characteristics of the Ross Registry. A, Cases per contributing center. B, Age and sex distribution of currently enrolled patients.
All contributing data are self-reported by the centers and are not audited. Initial data are collected at the time of surgery, which include demographic data, comorbidities, echocardiographic data, anatomical findings, surgical details, and information on the postoperative course until discharge including echocardiography and perioperative complications. Follow-up data are collected regarding mortality status, cause of death, New York Heart Association status, presence of symptoms, redo surgery or reintervention on the autograft or RVOT graft, autograft and RVOT graft function, occurrence of complications (such as stroke, bleeding, thromboembolism, endocarditis, rhythm disorders, etc), and echocardiographic data.
The Ross Registry—Lessons Learned From the Past
Surgical Technique of Autograft Insertion
It soon became clear that one cannot speak of “the” Ross procedure, as over time several modifications of the surgical technique have been introduced (Figure 1). The original subcoronary inclusion technique (SC) is technically demanding, as autograft inclusion inside the aortic annulus may lead to distortion of the valvular geometry, increased gradients, or regurgitation (Figure 1, A). This led to the introduction of the total root replacement technique (RR), which was then adopted by most of the surgeons performing the Ross procedure (Figure 1, B). RR is performed similar to a Bentall procedure, with reinsertion of the coronary ostia. Böhm and colleagues11 compared these 2 techniques with regard to hemodynamic results after a follow-up of 2.8 years. It was demonstrated that RR performed slightly but statistically significantly worse than SC in terms of the transvalvular gradient and the orifice area of the autograft.11 Interestingly, the rate of autograft regurgitation >I was low but greater after RR (RR 2.8% vs SC 1.5%).11 Subsequent clinical reports on longer-term outcomes raised concerns over an increased risk for reintervention on the autograft after RR, which was to be mainly due to progressive autograft dilatation.12,13 Pure aortic regurgitation and a large annular diameter at the time of the Ross procedure were consistently shown to be risk factors for future autograft dilatation and thus the risk for autograft failure. As a failure mechanism, the sudden exposure of the pulmonic autograft to systemic pressures seemed a plausible explanation. As a consequence, the procedure was modified by adding 1 or more reinforcement components to counteract this phenomenon (root replacement + reinforcement [RR + R]) (Figure 1, C). Data on 1335 patients showed that RR without reinforcement was associated with a 6-fold increased rate of autograft reoperation compared with RR + R.14 Furthermore, we observed excellent outcomes using mainly the SC technique at our institution.15, 16, 17 However, in our latest work comprising 2444 patients, the surgical technique (SC, RR, and RR + R) was not independently related to long-term survival outcomes.18 Collectively, there is no compelling evidence that clearly suggests the superiority of one technique over the other. This is also reflected by worldwide clinical practice in which different centers favor different approaches.
RVOT—Replacement Substitutes
Another technical aspect concerns the substitute for the RVOT. Surgery on the RVOT in patients with a healthy pulmonary valve is a major point of criticism regarding the use of the Ross procedure in patients with aortic stenosis. Therefore, a key to long-term success is to achieve a good hemodynamic result with a low risk of RVOT reintervention. RVOT replacement failure can occur due to valve regurgitation and/or stenosis. Although most of the functional valve deterioration was found to happen within 2 years of the Ross procedure, the incidence of significant failure requiring reintervention in the long term was low.19,20 Unlike the pulmonary autograft in aortic position, factors associated with RVOT reintervention are mainly related to “external” factors that facilitate degeneration rather than technical aspects. The use of a biological valve prosthesis (xenograft) was shown to be associated with a shorter time to reintervention, mainly due to tissue ingrowth at the proximal anastomosis site causing valve stenosis.21 With homografts, our group and others observed significantly better results with an estimated freedom from reintervention rate of 92.3% at 15 years.22 Patient-related factors such as younger age or sex have been suggested as risk factors as well. In our most recent analysis, the use of a biological valve prosthesis was significantly associated with a shorter time to RVOT reintervention compared with homografts.18 Therefore, at our institution, homografts are currently the RVOT substitute of choice. However, we consider the limited availability of homografts a significant limitation for the Ross procedure. Currently, the waiting time for a homograft in Germany is >3 weeks, which is not sufficient for some patient cases. Therefore, further improvement of RVOT substitutes in our view bears potential to improve outcomes even more.
The Ross Registry—Perspective
So far, the Ross registry has provided unique long-term follow-up data up to 25 years. The latest analysis was recently published and showed excellent long-term results with regard to survival as well as the risk of reintervention, thromboembolism, bleeding, and endocarditis.18 Despite these achievements, many questions remain open. The optimal surgical technique and RVOT substitute of choice are still a matter of debate, and number of patients who have reached follow-up >15 to 20 years is still low. Therefore, obtained results are estimates with variable accuracy. One of the most important aspects and challenges for the future will be to maximize inclusion of patient numbers and complete follow-up data to further increase the scientific and clinical value of this registry. At this stage, we would warmly welcome any Ross Center worldwide to participate in this registry.
Another remaining question is whether single-arm registry data are suitable for comparison with external data from patients with other aortic valve replacement (AVR) substitutes (ie, mechanical AVR). Although one RCT including patients who underwent the Ross procedure has compared the Ross procedure with aortic homograft replacement,7 the other RCT is limited by a low patient number (n = 20).8 A large RCT that compares the Ross procedure with AVR using contemporary prosthetic valves is needed, but it is highly questionable if such a trial can be conducted due to significant challenges. First, the Ross procedure is performed by a relatively small number of centers and limited number of surgeons. Second, young and middle-aged patients undergoing AVR are typically otherwise healthy; therefore, a long follow-up period would be required to detect any significant difference in outcomes. Third, implications of each treatment arm on the patient's life are dramatically different (eg, lifelong anticoagulation, etc). As a result, patients and physicians often have strong biases in favor or against different AVR options, and patients are not willing to participate in randomization. Therefore, in the foreseeable future, the Ross registry will remain an important data source of patients who underwent the Ross procedure, and continued follow-up of these will be critical to evaluate outcomes into the third decade after the initial operation. In addition, long-term functionality and durability for newer RVOT substitutes, such as cell free homografts, will be evaluated, and the database has been extended to also incorporate data of an increasing number of interventional therapies (eg, transcatheter aortic valve replacement) in the context of the Ross procedure.
Conclusions
Data from the multicenter Ross Registry have given answers to some important aspects regarding the Ross procedure. Past analyses indicate that this operation seems to hold its promise with regard to a sustained long-term result characterized by excellent survival and low valve-related morbidity. The Ross procedure is the only treatment option for aortic stenosis that has shown the potential to restore life expectancy, matching that of the age- and sex-matched general population. Nevertheless, there is a certain risk of reoperation and a late decline in valve performance in some patients, indicating that the Ross procedure does not entirely match normal aortic valve conditions. For further quality improvement, a high degree of standardization using modern technology such as artificial intelligence would be an interesting approach. All efforts have to be undertaken to maintain the high-quality level of the procedure and further improve outcomes while regularly reviewing contemporary outcomes by providing scientific reports. This should always be performed taking into account “competing” therapeutic options and the development of innovations in this field. This is the only way to increase acceptance of this procedure among physicians, which will translate to an increased interest in patients as well. The goal of the Ross Registry is not to promote the use of the Ross procedure but to optimize patient care for patients with aortic valve disease.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
References
- 1.David T.E., Ouzounian M., David C.M., Lafreniere-Roula M., Manlhiot C. Late results of the Ross procedure. J Thorac Cardiovasc Surg. 2019;157:201–208. doi: 10.1016/j.jtcvs.2018.06.037. [DOI] [PubMed] [Google Scholar]
- 2.Andreas M., Seebacher G., Reida E., Wiedemann D., Pees C., Rosenhek R., et al. A single-center experience with the Ross procedure over 20 years. Ann Thorac Surg. 2014;97:182–188. doi: 10.1016/j.athoracsur.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 3.Franke U.F.W., Ursulescu A., Göbel N., Nagib R., Hansen M., Yadav R., et al. Results and quality of life after minimally invasive Ross procedure. J Heart Valve Dis. 2015;24:295–301. [PubMed] [Google Scholar]
- 4.Yacoub M.H., El-Hamamsy I., Sievers H.-H., Carabello B.A., Bonow R.O., Stelzer P., et al. Under-use of the Ross operation—a lost opportunity. Lancet. 2014;384:559–560. doi: 10.1016/S0140-6736(14)61090-4. [DOI] [PubMed] [Google Scholar]
- 5.Nishimura R.A., O'Gara P.T., Bonow R.O. Guidelines update on indications for transcatheter aortic valve replacement. JAMA Cardiol. 2017;2:1036–1037. doi: 10.1001/jamacardio.2017.2546. [DOI] [PubMed] [Google Scholar]
- 6.Baumgartner H., Falk V., Bax J.J., De Bonis M., Hamm C., Holm P.J., et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739–2791. doi: 10.1093/eurheartj/ehx391. [DOI] [PubMed] [Google Scholar]
- 7.El-Hamamsy I., Eryigit Z., Stevens L.-M., Sarang Z., George R., Clark L., et al. Long-term outcomes after autograft versus homograft aortic root replacement in adults with aortic valve disease: a randomised controlled trial. Lancet. 2010;376:524–531. doi: 10.1016/S0140-6736(10)60828-8. [DOI] [PubMed] [Google Scholar]
- 8.Doss M., Wood J.P., Martens S., Wimmer-Greinecker G., Moritz A. Do pulmonary autografts provide better outcomes than mechanical valves? A prospective randomized trial. Ann Thorac Surg. 2005;80:2194–2198. doi: 10.1016/j.athoracsur.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Fujita B., Ensminger S., Bauer T., Möllmann H., Beckmann A., Bekeredjian R., et al. GARY Executive Board Trends in practice and outcomes from 2011 to 2015 for surgical aortic valve replacement: an update from the German Aortic Valve Registry on 42 776 patients. Eur J Cardiothorac Surg. 2018;53:552–559. doi: 10.1093/ejcts/ezx408. [DOI] [PubMed] [Google Scholar]
- 10.Tam D.Y., Rocha R.V., Wijeysundera H.C., Austin P.C., Dvir D., Fremes S.E. Surgical valve selection in the era of transcatheter aortic valve replacement in the Society of Thoracic Surgeons Database. J Thorac Cardiovasc Surg. 2020;159:416–427.e8. doi: 10.1016/j.jtcvs.2019.05.081. [DOI] [PubMed] [Google Scholar]
- 11.Böhm J.O., Botha C.A., Hemmer W., Schmidtke C., Bechtel J.F.M., Stierle U., et al. Hemodynamic performance following the Ross operation: comparison of two different techniques. J Heart Valve Dis. 2004;13:174–180. discussion 180-1. [PubMed] [Google Scholar]
- 12.Klieverik L.M.A., Takkenberg J.J.M., Bekkers J.A., Roos-Hesselink J.W., Witsenburg M., Bogers A.J.J.C. The Ross operation: a Trojan horse? Eur Heart J. 2007;28:1993–2000. doi: 10.1093/eurheartj/ehl550. [DOI] [PubMed] [Google Scholar]
- 13.Juthier F., Vincentelli A., Pinçon C., Banfi C., Ennezat P.V., Maréchaux S., et al. Reoperation after the Ross procedure: incidence, management, and survival. Ann Thorac Surg. 2012;93:598–604. doi: 10.1016/j.athoracsur.2011.06.083. discussion 605. [DOI] [PubMed] [Google Scholar]
- 14.Charitos E.I., Hanke T., Stierle U., Robinson D.R., Bogers A.J.J.C., Hemmer W., et al. Autograft reinforcement to preserve autograft function after the ross procedure: a report from the German-Dutch Ross registry. Circulation. 2009;120(11 suppl):S146–S154. doi: 10.1161/CIRCULATIONAHA.108.843391. [DOI] [PubMed] [Google Scholar]
- 15.Sievers H.-H., Stierle U., Charitos E.I., Hanke T., Gorski A., Misfeld M., et al. Fourteen years’ experience with 501 subcoronary Ross procedures: surgical details and results. J Thorac Cardiovasc Surg. 2010;140:816–822. doi: 10.1016/j.jtcvs.2009.11.042. 822.e1-5. [DOI] [PubMed] [Google Scholar]
- 16.Charitos E.I., Stierle U., Hanke T., Schmidtke C., Sievers H.-H., Richardt D. Long-term results of 203 young and middle-aged patients with more than 10 years of follow-up after the original subcoronary Ross operation. Ann Thorac Surg. 2012;93:495–502. doi: 10.1016/j.athoracsur.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Sievers H.H. Ross procedure. HSR Proc Intensive Care Cardiovasc Anesth. 2012;4:119–123. [PMC free article] [PubMed] [Google Scholar]
- 18.Aboud A., Charitos E., Fujita B., Stierle U., Reil J.C., Voth V., et al. Long-term outcomes of patients undergoing the Ross procedure. J Am Coll Cardiol. 2021;77:1412–1422. doi: 10.1016/j.jacc.2021.01.034. [DOI] [PubMed] [Google Scholar]
- 19.Mokhles M.M., Charitos E.I., Stierle U., Rajeswaran J., Blackstone E.H., Bogers A.J., et al. The fate of pulmonary conduits after the Ross procedure: longitudinal analysis of the German-Dutch Ross registry experience. Heart. 2013;99:1857–1866. doi: 10.1136/heartjnl-2013-304425. [DOI] [PubMed] [Google Scholar]
- 20.Charitos E.I., Takkenberg J.J.M., Hanke T., Gorski A., Botha C., Franke U., et al. Reoperations on the pulmonary autograft and pulmonary homograft after the Ross procedure: an update on the German Dutch Ross registry. J Thorac Cardiovasc Surg. 2012;144:813–821. doi: 10.1016/j.jtcvs.2012.07.005. discussion 821-3. [DOI] [PubMed] [Google Scholar]
- 21.Weimar T., Charitos E.I., Liebrich M., Roser D., Tzanavaros I., Doll N., et al. Quo vadis pulmonary autograft—the Ross procedure in its second decade: a single-center experience in 645 patients. Ann Thorac Surg. 2014;97:167–174. doi: 10.1016/j.athoracsur.2013.07.078. [DOI] [PubMed] [Google Scholar]
- 22.Sievers H.-H., Stierle U., Charitos E.I., Takkenberg J.J.M., Hörer J., Lange R., et al. A multicentre evaluation of the autograft procedure for young patients undergoing aortic valve replacement: update on the German Ross registry. Eur J Cardiothorac Surg. 2016;49:212–218. doi: 10.1093/ejcts/ezv001. [DOI] [PubMed] [Google Scholar]