Abstract
Background
This study examines the patterns and predictors of depression and anxiety trajectories among adolescents during COVID-19 lockdown in China.
Methods
A total of 35,516 college students were followed from the pandemic outbreak period, initial remission period, and control period. Participants completed the Patient Heath Questionnaire, Generalized Anxiety Disorder Scale, Perceived Social Support Scale, the Simplified Coping Style Questionnaire, and APGAR-family scale. Distinct patterns of depression and anxiety trajectories were established through grouping participants based on time-varying changes of the cut-off score. Multivariate logistic regressions were used to examine predictors for trajectory membership.
Results
Depression and anxiety prevalence during the COVID-19 outbreak were 21.3% and 11.5% respectively, and symptoms worsened as the lockdown time increased. Five depression/anxiety trajectories were observed: resistance, recovery, relapsing/remitting, delayed-dysfunction and chronic-dysfunction. Gender, academic year, residence location, history of mental health, and COVID-19 community exposure were significant predictors of distinct trajectories for depression or anxiety. Less social support or positive coping, more negative coping, and poorer family function were also risk predictors for not developing delayed or chronic dysfunction.
Conclusions
Although most adolescents remain euthymic or recover over time, some adolescents, especially those with the risk factors noted above, exhibit delayed or chronic symptoms. Thus, the need for individualized intervention with these adolescents is indicated.
Keywords: Longitudinal studies, Depression, Anxiety, Trajectories, COVID-19
1. Introduction
Substantial evidence indicates that the coronavirus disease 2019 (COVID-19) pandemic has alarming implications for global mental health. Depression and anxiety symptoms are the most likely mental health problems after the pandemic outbreak. An increasing number of studies suggested that a higher proportion of depression and anxiety persisted, and symptoms sharply increased during the pandemic outbreak (Feter et al., 2021; Wang et al., 2020a).
Several two-wave studies have attempted to investigate changes in individual depression and anxiety during the pandemic. For example, one study in U.S. adults showed that high rates of depression and anxiety began emerging in May 2020 but then began decreasing 1 month later (Kujawa et al., 2020). Data form Spain showed depression increased significantly over time (within one month of a pandemic outbreak), while anxiety did not show significant changes (Gonzalez-Sanguino et al., 2021). Given the ongoing pandemic, long-term longitudinal studies on mental health over time and an analysis of depression and anxiety development following a pandemic are needed.
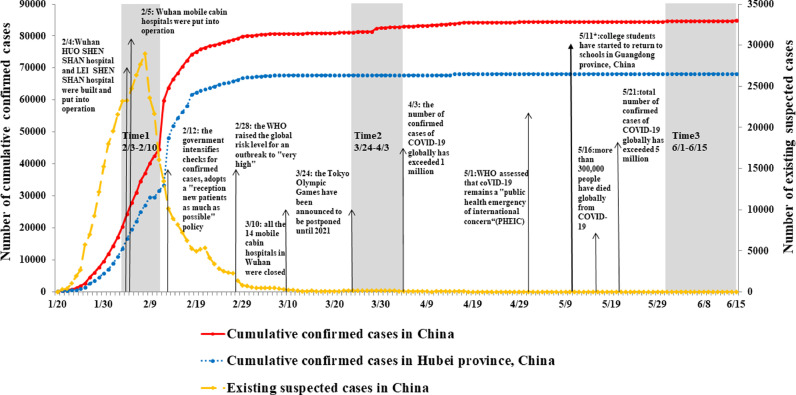
In China, the COVID-19 outbreak suddenly began in the winter of 2019 in the Wuhan city of Hubei Province. Subsequently, the pandemic had spread across China during the rapid initial outbreak phase from January 23 to March 10, 2020. At this time, the total number of confirmed cases of COVID-19 in China increased to 80, 905. Due to rising concerns about the pandemic, China has taken confinement measures, including contact restrictions, self-isolation, and closure of schools, colleges/ universities, and other educational institutions. Students were required to pursue their studies online at home. Since March 10, 2020, the pandemic in China has been basically under control, with newly confirmed cases in the Hubei Province near zero, and newly confirmed cases nationwide showing a consistent downward trend (Li et al., 2021). Since May, there has been very low newly confirmed cases per day, with a clear downward trend nationwide (The State Council Information Office of the People's Republic of China, 2020). Hence, many colleges/universities started to re-open and allowed students to return to school in batches. However, a longitudinal study of depression and anxiety in students during COVID-19 lockdown has not been well-documented.
Previous studies have suggested that students are a demographic that has experienced a greater psychological impact from the pandemic (Wang et al., 2020b), revealing that the prevalence of adolescents’ depression and anxiety was higher than in the general population in China in the early and peak periods of COVID-19 (Zhou et al., 2020). It is, however, noteworthy that little is known about trajectories of depression and anxiety in students over course of the COVID-19. Accordingly, we focused on depression and anxiety symptoms for college students during COVID-19 lockdown. This study had two main aims: first, to explore trajectories of depressive and anxiety symptoms over the quarantine period; and second, to identify those who were at highest risk of showing exacerbating trajectories of mental health problems across the lockdown period.
2. Methods
2.1. Participant and procedure
During the COVID-19 pandemic, our team organized three large-scale cross-sectional online surveys during the outbreak period (Time 1, T1: February 3 to 10, 2020), the initial remission period (Time 2, T2: March 24 to April 3, 2020), and the control period (Time 3, T3: June 1 to 15, 2020). Groups of college students from 22 colleges/ universities in Guangzhou Province volunteered to participate in our survey. For Guangdong Province, the cumulative COVID-19 confirmed cases ranged from 1000 to 9999, which were pandemic moderate-risk areas as assessed by the World Health Organization in early 2020 (WHO, 2020). The trend of the COVID-19 pandemic in China and detailed sample procedures are shown in Fig. 1 . Through data integration, a total of 35,516 college students participated in all three online surveys and provided complete data on all measures.
Fig. 1.
The national pandemic trend of the 2019 coronavirus disease (COVID-19) in China and sampling time windows.
The survey was highly supported by the local education bureau, and each school sent a survey invitation letter to students and their parents via electronic text messages before the survey. All participants gave electronic informed consent before starting the online survey. The data in this study were collected and managed using the “Survey Star” system, which is a convenient, web-based software platform designed to support data collection for research. Participants accessed each wave of web-based survey by scanning the Quick Response (QR) code of the questionnaire with mobile phones at home. Responses to the survey were kept confidential, with right to withdraw freely during test period. The detailed investigation process has been described in previous studies (Li et al., 2021; Ma et al., 2020; Wang et al., 2021)
The investigation was carried out in accordance with the Helsinki Declaration as revised 1989 and approved by the Ethics Committees of South China Normal University (Ethics_No._SCNU-PSY-2020–01–001). We also opened a free psychological hotline (the ‘Xinqing’ hotline) to provide free psychological assistance services to participants.
2.2. Measures
In this study, college students completed the Patient Health Questionnaire (PHQ-9) (Kroenke et al., 2001), Generalized Anxiety Disorder (GAD-7) (Spitzer et al., 2006), Perceived Social Support Scale (PSSS) (Zimet et al., 1990), Simplified Coping Style Questionnaire (SCSQ) (Xie, 1998), and APGAR-family scale (Smilkstein, 1993). In additional, a questionnaire was developed to obtain socio-demographic and COVID-19 pandemic and lockdown related data.
The PHQ-9 (9 items, range, 0–27) and GAD-7 (7 items, range, 0–21) were used to assess to students’ depressive and anxiety symptoms over past two weeks. Each item rated from 0 (not at all) to 3 (nearly every day), with both maintaining a cut-off total score of 7 to suggest probable clinical depression (Wang et al., 2014) or anxiety (Tong et al., 2016) in the Chinese sample. For current sample, Cronbach's alpha were high at all three timepoints (PHQ-9: 0.87, 0.90, 0.91, respectively; GAD-7: 0.91, 0.93, 0.94, respectively).
Meanwhile, we also focused on some psychosocial factors of interest in this study, including social support, copying styles, and family function. Social support was measured at T1 through Perceived Social Support Scale (PSSS) (Zimet et al., 1990). PSSS is a 12-item scale, with each item scored from 0 (very strongly disagree) to 7 (strongly agree), and a higher total score indicate a greater level of perceived social support. Its Cronbach's alpha was 0.94 in this study. Copying style was assessed by Simplified Coping Style Questionnaire (SCSQ) (Xie, 1998) at T1. The SCSQ consists of 12 items, with two subscales: positive coping (12 items); and negative coping (8 items). Responses to items range from 0-never, to 3-often, and a higher score indicates more frequent use of the coping style. Acceptable reliability (Cronbach's alpha for positive/negative coping=0.90/0.78) was found in the current sample. Social support and coping style were recoded into three categories, with low and high categories defined by the 27th and 73rd percentile. Family function was assessed by the APGAR-family scale (Smilkstein, 1993) at T2, which asks students to report the level of agreement with 5 items on a 3-point scale (form 0- never or rarely to 2-most or all of the time). A total score of 7–10 indicates a good family function, 4–6 indicates a fair family function and 0–3 indicates poor family function. This scale had a good internal consistency in this sample, and Cronbach's α was 0.90.
In addition, gender was defined as a binary variable for male or female. Academic year was defined as a categorical variable with 5 groups: freshman, sophomore, junior, senior, postgraduate. Residence location was defined as a categorical variable with 2 groups: rural and urban. Participants also self-reported their number of family members (only child status) and whether they have a history of mental illness. COVID-19 related factors mainly examined whether there are confirmed or suspected cases in the community/ village where the participant is located, and whether the participant's relatives or friends were infected with COVID-19.
2.3. Statistical analysis
The non-parametric test was used to compare the three timepoints. We also compared the depression and anxiety prevalence rates among different groups of demographic characteristics and pandemic related factors provided from each survey. Different patterns of depression and anxiety trajectories were established through grouping participants based on time-varying changes of developing depression and anxiety (reaching a cut-off point of 7). We expected to detect five trajectories that were commonly observed in previous research (Fan et al., 2015), i.e., resistance, recovery, chronic-dysfunction, delayed-dysfunction, and relapsing/remitting. Multivariate logistic regressions were used to examine predictors for the occurrence and trajectory of depression and anxiety symptoms. All of the statistical analyses were performed using SPSS 23.0, and the level of significance was set to P < 0.05.
3. Results
3.1. Sample characteristics
Among 35,516 participants, 9244 were male and 26,272 were female, and the mean (SD) age was 20.29 (1.85) years. This survey included data from 2352 students (6.6%) living in communities or villages with confirmed cases of COVID-19, 400 (1.1%) participants reported relatives or friends being infected with COVID-19. Other demographic characteristics are shown in Table 1 .
Table 1.
Prevalence of depression and anxiety at three surveys by demographics and pandemic related factors (N = 35,516).
| Depression (%) | Anxiety (%) | |||||
|---|---|---|---|---|---|---|
| Characteristics (n) | T1 | T2 | T3 | T1 | T2 | T3 |
| Gender | ||||||
| Male (9244) | 19.4 | 25.0 | 30.9 | 10.9 | 14.5 | 18.6 |
| Female (26,272) | 22.6 | 26.6 | 33.5 | 11.7 | 14.4 | 18.2 |
| χ2 | 39.40*** | 8.63** | 20.58*** | 4.22* | 0.09 | 0.70 |
| Grade | ||||||
| Freshman (12,726) | 20.2 | 23.9 | 32.8 | 12.3 | 16.5 | 20.0 |
| Sophomore (10,447) | 22.3 | 26.0 | 34.6 | 13.0 | 18.6 | 20.0 |
| Junior (7258) | 22.9 | 28.3 | 35.1 | 12.7 | 15.7 | 19.8 |
| Senior (3147) | 24.4 | 30.7 | 33.6 | 11.8 | 13.9 | 18.6 |
| Postgraduate (1938) | 20.5 | 26.5 | 30.6 | 10.0 | 12.8 | 16.5 |
| χ2 | 39.18*** | 84.18*** | 53.22*** | 49.30*** | 92.28*** | 49.00*** |
| Residence location | ||||||
| Rural (14,347) | 20.9 | 26.6 | 33.5 | 11.7 | 14.5 | 18.5 |
| Urban (21,169) | 22.3 | 25.6 | 32.0 | 11.2 | 14.3 | 18.0 |
| χ2 | 9.37** | 4.64* | 8.93** | 2.43 | 0.29 | 1.42 |
| Only-children family | ||||||
| Yes (7266) | 20.8 | 25.3 | 31.7 | 11.4 | 13.8 | 17.9 |
| No (28,250) | 22.0 | 26.4 | 33.2 | 11.5 | 14.6 | 18.4 |
| χ2 | 5.27* | 3.56 | 5.57* | 0.02 | 3.11 | 0.92 |
| History of mental illness | ||||||
| Yes (296) | 51.4 | 51.4 | 55.7 | 30.7 | 28.4 | 34.5 |
| No (35,220) | 21.5 | 26.0 | 32.7 | 11.3 | 14.3 | 18.2 |
| χ2 | 153.75*** | 97.89*** | 70.88*** | 109.01*** | 47.22*** | 52.07*** |
| Confirmed COVID-19 cases in the community or village | ||||||
| Yes (2352) | 29.8 | 34.8 | 40.3 | 16.2 | 19.7 | 23.7 |
| No (33,164) | 21.2 | 25.6 | 32.3 | 11.1 | 14.0 | 17.9 |
| χ2 | 95.13*** | 97.40*** | 64.11*** | 55.21*** | 57.74*** | 48.65*** |
| Relatives or friends being infected with COVID-19 | ||||||
| Confirmed/suspected (400) | 35.0 | 37.5 | 45.0 | 20.5 | 21.3 | 26.8 |
| No (35,116) | 21.6 | 26.0 | 32.7 | 11.4 | 14.3 | 18.2 |
| χ2 | 41.77*** | 26.84*** | 27.05*** | 32.40*** | 15.34*** | 19.28*** |
T1 = measured at Time 1, T2 = measured at Time 2, T3 = measured at Time 3.
*p < 0.05
**p < 0.01.
**p < 0.001.
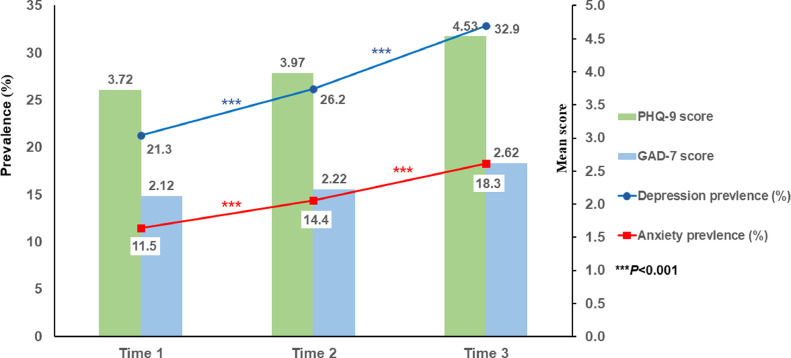
3.2. Prevalence of depression/ anxiety
The prevalence rates of depression at three time points were 21.3%, 26.2%, and 32.9% respectively, and the prevalence rates for anxiety were 11.5%, 14.4%, and 18.3% respectively. Overall, the detection rate of depression and anxiety increases significantly with the increase in home-isolation time (see Fig. 2 ). Table 1 presents the differences in depression and anxiety prevalence at each survey time point between different groups of demographic characteristics and pandemic related factors.
Fig. 2.
The prevalence rates of depression and anxiety at three timepoints.
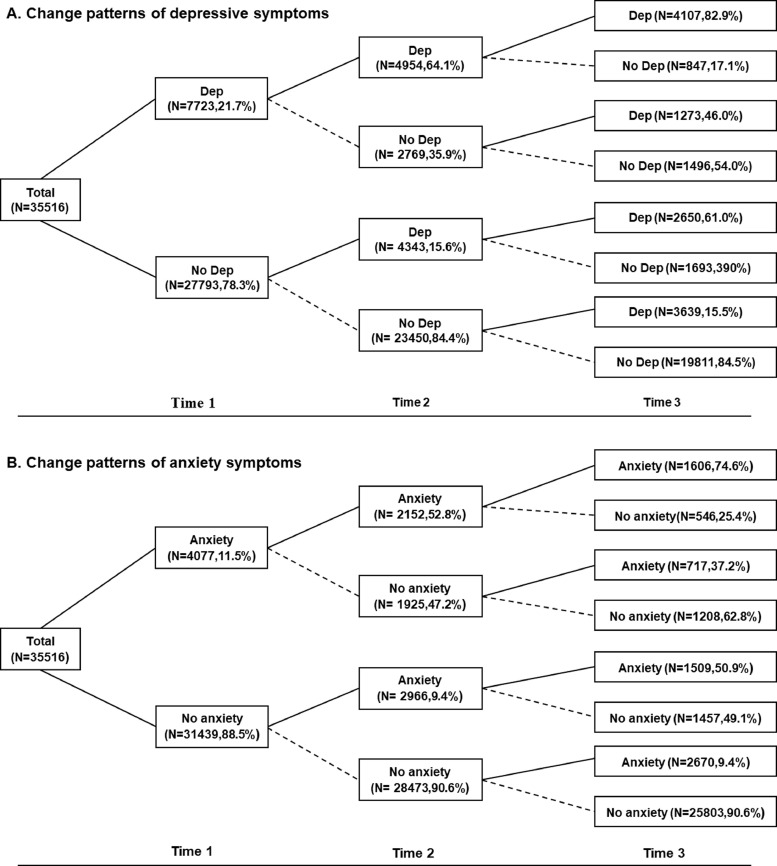
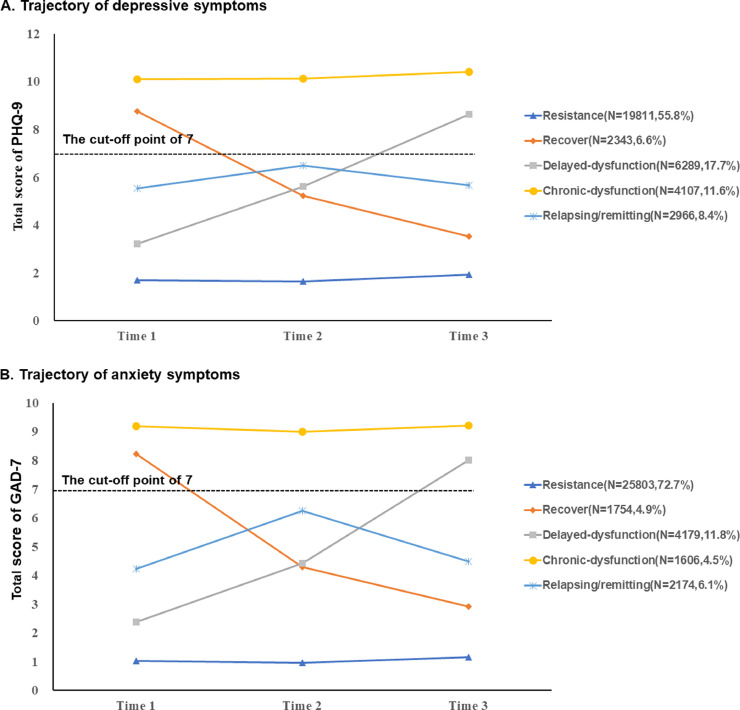
3.3. Trajectories of depression and anxiety symptoms
The overall trajectories of depression were presented in Fig. 3 A, and we also identified five groups of depression trajectory in Fig. 4. A, i.e., resistance, recovery, delayed-dysfunction, chronic-dysfunction, and relapsing/ remitting. 55.8% (N = 19,811) of the cohort did not meet criteria for depression (reaching a cut-off point of 7) during the three waves, and these students were classified as resistance group. 11.6% (N = 4107) met criteria at all three waves and classified as chronic-dysfunction group. The delayed-dysfunction group, comprising 17.7% of the sample, was characterized by students’ depression being negative at Time 1 and/ or Time 2 but positive at Time 3. The recovery group (6.6% of the sample) was characterized by students’ depression being positive at Time 1 and/ or Time 2 but negative at Time 3. The relapsing/remitting group (8.4% of the sample) was characterized by students’ depression fluctuating across the follow-up period. Among these students in relapsing/remitting group, 4.8% (n = 1496) showed no depression at Time 1 and onset at Time 2, while remission at Time 3. 3.6% (n = 1273) showed depression at Time 1 and remission at Time 2, while relapse at Time 3.
Fig. 3.
Change patterns of depression and anxiety Fig. 3A Change patterns of depression. Fig. 3B Change patterns of anxiety.
Fig. 4.
Trajectory of depression and anxiety. Fig. 4.A Trajectory patterns of depression. Fig. 4.B Trajectory patterns of anxiety.
To maintain consistency with the approach as stated above, the same change patterns were also selected for anxiety (see Fig. 3B). Fig. 4B also showed the five trajectories of anxiety: resistance (72.7%), recovery (4.9%), delayed-dysfunction (11.8%), chronic-dysfunction (4.5%), and relapsing/ remitting (6.1%).
3.4. Predictors of depression/anxiety trajectory membership
Our major interest was to explore the factors associated with increased likelihood of developing delayed-dysfunction and chronic-dysfunction. We first set the resistance group as the reference group and compared it with delayed-dysfunction group, and then set the recovery group as the reference group and compared it with chronic dysfunction group. As shown in Table 2 , the likelihood of developing depression in a delayed-dysfunction group increased if the college students were females, higher academic year, living in urban areas, had a history of mental illness, and living in the community or village with confirmed cases of COVID-19. Lower social support or positive coping, higher negative coping, and poorer family function were associated with depression of new onset or persistent course during lockdown.
Table 2.
Risk and protective factors of depression or anxiety symptom trajectory groups.
| Depression | Anxiety | ||||
|---|---|---|---|---|---|
| Delay v. Resis | Chron v. Recov | Delay v. Resis | Chron v. Recov | ||
| Gender (Male as Ref.) | |||||
| Female | 1.18(1.10,1.26)*** | 1.10(0.98,1.25) | 1.02(0.95,1.10) | 1.11(0.95,1.31) | |
| Grade (Freshman as Ref.) | |||||
| Sophomore | 1.14(1.06,1.23)*** | 1.09(0.96,1.24) | 1.13(1.04,1.23)** | 0.98(0.82,1.16) | |
| Junior | 1.31(1.21,1.42)*** | 1.06(0.91,1.21) | 1.29(1.18,1.42)*** | 0.96(0.79,1.16) | |
| Senior | 1.36(1.22,1.52)*** | 1.09(0.90,1.31) | 1.45(1.28,1.64)*** | 1.09(0.86,1.40) | |
| Postgraduate | 1.57(1.38,1.79)*** | 1.18(0.92,1.50) | 1.89(1.63,2.20)*** | 0.89(0.65,1.22) | |
| Residence location (Rural as Ref.) | |||||
| Urban | 1.11(1.04,1.18)** | 0.96(0.86,1.08) | 1.04(0.97,1.12) | 1.04(0.90,1.20) | |
| Only-children family (No as Ref.) | |||||
| Yes | 0.98(0.91,1.06) | 1.07(0.94,1.23) | 1.03(0.94,1.12) | 1.00(0.84,1.20) | |
| History of mental illness (No as Ref.) | |||||
| Yes | 1.52(1.05,2.20)* | 1.47(0.98,2.19) | 1.37(0.96,1.95) | 1.37(0.86,2.19) | |
| Confirmed COVID-19 cases in the community or village (No as Ref.) | |||||
| Yes | 1.29(1.15,1.45)*** | 1.18(0.99,1.42) | 1.37(1.20,1.55) *** | 0.96(0.76,1.21) | |
| Relatives or friends being infected with COVID-19 (No as Ref.) | |||||
| Confirmed/suspected | 1.30(0.98,1.73) | 1.39(0.92,2.10) | 1.32(0.98,1.78) | 1.11(0.68,1.83) | |
| Social support at T1(Low as Ref.) | |||||
| Medium | 0.79(0.73,0.85)*** | 0.77(0.68,0.87)*** | 0.64(0.59,0.69)*** | 0.72(0.61,0.84) ** | |
| High | 0.55(0.49,0.61)*** | 0.64(0.53,0.78)*** | 0.49(0.43,0.56)*** | 0.70(0.49,1.00) * | |
| Positive coping at T1 (Low as Ref.) | |||||
| Medium | 0.81(0.75,0.88)** | 0.83(0.73,0.95)** | 0.76(0.70,0.84)*** | 0.96(0.82,1.14) | |
| High | 0.71(0.64,0.79)*** | 0.70(0.59,0.83)*** | 0.69(0.61,0.77)*** | 0.88(0.67,1.15) | |
| Negative coping at T1 (Low as Ref.) | |||||
| Medium | 1.81(1.66,1.97)*** | 1.84(1.50,2.27)*** | 1.72(1.54,1.91)*** | 1.32(0.96,1.80) | |
| High | 3.02(2.72,3.34)*** | 2.55(2.04,3.18)*** | 3.14(2.78,3.54)*** | 1.77(1.28,2.44)** | |
| Family function at T2 (Poor as Ref.) | |||||
| Fair | 0.69(0.62,0.78)*** | 0.77(0.65,0.91)*** | 0.80(0.71,0.90)*** | 1.05(0.86,0.63) | |
| Good | 0.36(0.32,0.41)*** | 0.42(0.35,0.50)*** | 0.38(0.34,0.43)*** | 0.50(0.40,0.63)*** | |
OR = odds ratio, CI = confidence interval.
Resis = resistance group, Recov = recovery group, Delay = delayed dysfunction group, Chron = chronic dysfunction group.
T1 = measured at Time 1, T2 = measured at Time 2.
*p < 0.05, **p < 0.01, *** p < 0.001.
For anxiety, the likelihood of developing delayed dysfunction was greater, as compared with the resistance group, for those reporting higher academic year, COVID-19 community exposure, a lower level of social support or positive coping, a higher level of negative coping, or poorer family function. Meanwhile, lower level of social support, higher level of negative coping, or poorer family function increased the likelihood of depression persisting during lockdown.
4. Discussion
The current study found that the overall severity of depression and anxiety increased during pandemic lockdown. Our findings also revealed five trajectories of PTSD symptoms, i.e. resistance, recovery, delayed-dysfunction, chronic-dysfunction, and relapsing/remitting. More importantly, this study suggests that female, higher academic year, residence in urban areas, a history of mental illness, and living in the community or village with confirmed cases of COVID-19 are associated with depression or anxiety onset, whereas lower social support or positive coping, higher negative coping, or poorer family function are associated with increased risks of depression or anxiety persistence and new onset.
Our data show that about 21.3% and 11.5% of college students experienced probable clinical depression and anxiety during the pandemic outbreak. The prevalence is similar to the results of previous studies with a larger sample. Ma and her colleagues found that about 21.1% and 11.1% of college students had probable depression and anxiety respectively among 746,217 college students assessed by the same measures (Ma et al., 2020). Meanwhile, we found that depression and anxiety increased to 32.5%% and 18.3% respectively after 4-month home isolation. This is contrary to the results of an adult study in England (Fancourt et al., 2021), suggesting depression and anxiety both declined across the first 20 weeks following the introduction of lockdown. This difference may be due to the relatively poorer adaptability of college students to circumstances than the general adult population. Majumdar et al. illustrated that prolonged home-isolation had a negative effect on students’ mental well-being, and possible reasons include physical inactivity, lack of academic schedule, increased reliance on digital use and so on (Majumdar et al., 2020).
Several demographics and pandemic related factors have been found to be related to changes in depression and anxiety. In line with previous studies (Tang et al., 2020), female students may be more likely to present with an onset of depression during COVID-19. Students with higher academic year showed a higher risk in developing depression and anxiety. It is well-documented that final year or graduate students report more psychological distress, possibly due to uncertainty about the pandemic's effect on their graduation and future employment (Cao et al., 2020; Cornine, 2020; Wang et al., 2021). Meanwhile, college students living in urban areas are more likely to report delayed depression dysfunction. A possible explanation for these results is that urban communities are more densely populated and thus exert higher risk of community infection. The United Nations also reported that urban areas may have poorer environment and infrastructure for the prevention of COVID-19 in many countries (United Nations, 2020). Our data revealed that a history of depression was associated with an elevated level of risk of being categorized in the delayed dysfunction group. Much literature has identified that people with a previous history of mental illness are more likely to experience more psychological symptoms during the pandemic (Goularte et al., 2021; McCracken et al., 2020). In additional, our observed positive association between COVID-19 community exposure and higher odds of depression or anxiety was consistent with results from 1487 Chinese adolescents from public schools (Ren et al., 2021). Another large sample survey also suggested that college students who lived in communities with confirmed cases were 1.55–1.59 times more likely than other students to develop depressive and anxiety symptoms (Ma et al., 2020).
The protective role of social support and family function in the mental health status of adolescents has already been evidenced in previous COVID-19 studies (Li et al., 2021; Ma et al., 2020). Our findings confirmed the role of social support in response to the long-term lockdown, showing that perceived greater levels of social support were common protective factors for depression and anxiety trajectories. Similarly, a dysfunctional family was also a vital psychosocial factor that increased the risk of developing mental health problems (Li et al., 2021). Better family function was found to increase the likelihood of the recovery trajectory relative to the outcome of chronic dysfunction. We speculated that students with better family functioning may get more family support, facilitating college students’ positive adaptation to public health emergencies. Furthermore, our findings are also consistent with a body of literature (Fu et al., 2020; Lew et al., 2019) showing that fewer positive coping and higher negative coping are associated with the persistence of mental health problems or their new occurrence. Specifically, positive coping was found to increase the likelihood of depression resistance. In contrast with the protective effect of positive coping, negative coping was a significant risk factor for depression and anxiety. These results highlighted the crucial role of integrating coping mechanism training into post-pandemic psychological interventions.
There are several strengths in our study. Longitudinal study was conducted with a large sample size in adolescents. Meanwhile, the three waves of the survey during pandemic lockdown provided an opportunity to explore the change of depressive and anxiety symptoms among adolescents after exposure to a special public health emergency. To the best of our knowledge, this is the first study showing the trajectories of mental health problems in adolescents across different stages of the COVID-19 pandemic. This study will help elucidate the links between the mechanisms of pandemic and mental health.
Despite these important findings, some limitations should be considered. First, due to the development of the COVID-19 pandemic, the interval between each survey was only about two months, this short follow-up interval may limit the understanding of the trajectory changes of mental health problems. Second, depression and anxiety relied on self-report questionnaires, which may have led to reporting bias caused by individuals’ own psychiatric states. Third, a repeated cross-sectional research design was used in this survey, so the sample loss rate was relatively high, which may lead to selection bias. Finally, the confounding factors caused by measurement at different time points may bring some bias to the results, such as seasonality.
5. Conclusion
In conclusion, this study makes a unique contribution to the literature by examining depression and anxiety developmental trajectories and related predictors in a large sample of college students during COVID-19 pandemic. The prevalence of mental health problems increased during home quarantine. Five trajectories were found: resistance, recovery, delayed-dysfunction, chronic-dysfunction, and relapsing/remitting. Gender, academic year, residence location, history of mental health, COVID-19 community exposure, social support, coping style, and family function were significant predictors of distinct trajectories for symptoms of depression or anxiety. These findings could inform mental health professionals regarding how to provide individualized and appropriate interventions for college students post-pandemic.
CRediT authorship contribution statement
Dongfang Wang: Conceptualization, Data curation, Formal analysis, Writing – original draft. Jingbo Zhao: Resources, Supervision, Writing – review & editing. Brendan Ross: Writing – review & editing. Zijuan Ma: Investigation, Formal analysis. Jinfang Zhang: Investigation, Formal analysis. Fang Fan: Supervision, Project administration, Writing – original draft. Xianchen Liu: Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare no conflicts of interest regarding data and materials presented in this paper.
Acknowledgments
Role of the founding source
The present study was funded by National Natural Science Foundation of China (Grant 31871129); Research on the Processes and Repair of Psychological Trauma in Youth, Project of Key Institute of Humanities and Social Sciences, MOE (Grant No. 16JJD190001); Guangdong Province Universities and Colleges Pearl River Scholar Funded Scheme (GDUPS 2016); and Graduate Research and Innovation Project of School of Psychology, South China Normal University (PSY-SCNU202017).
Acknowledgements
The authors want to express their sincere appreciation to all people who involved in the study and the partner schools.
Availability of data and materials
Please contact PhD Fang Fan at fangfan@scnu.edu.cn for data supporting the findings of the current study
References
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornine A. Reducing nursing student anxiety in the clinical setting: an integrative review. Nurs. Educ. Perspect. 2020;41:229–234. doi: 10.1097/01.NEP.0000000000000633. [DOI] [PubMed] [Google Scholar]
- Fan F., Long K., Zhou Y., Zheng Y., Liu X. Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China. Psychol. Med. 2015;45:2885–2896. doi: 10.1017/S0033291715000884. [DOI] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiat. 2021;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feter N., Caputo E.L., Doring I.R., Leite J.S., Cassuriaga J., Reichert F.F., Da S.M., Coombes J.S., Rombaldi A.J. Sharp increase in depression and anxiety among Brazilian adults during the COVID-19 pandemic: findings from the PAMPA cohort. Public Health. 2021;190:101–107. doi: 10.1016/j.puhe.2020.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu W., Wang C., Zou L., Guo Y., Lu Z., Yan S., Mao J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan. China. Transl. Psychiatry. 2020;10:225. doi: 10.1038/s41398-020-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Sanguino C., Ausin B., Castellanos M.A., Saiz J., Munoz M. Mental health consequences of the Covid-19 outbreak in Spain. A longitudinal study of the alarm situation and return to the new normality. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2020.110219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goularte J.F., Serafim S.D., Colombo R., Hogg B., Caldieraro M.A., Rosa A.R. COVID-19 and mental health in Brazil: psychiatric symptoms in the general population. J. Psychiatr. Res. 2021;132:32–37. doi: 10.1016/j.jpsychires.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kujawa A., Green H., Compas B.E., Dickey L., Pegg S. Exposure to COVID-19 pandemic stress: associations with depression and anxiety in emerging adults in the United States. Depress. Anxiety. 2020;37:1280–1288. doi: 10.1002/da.23109. [DOI] [PubMed] [Google Scholar]
- Lew B., Huen J., Yu P., Yuan L., Wang D., Ping F., Abu Talib M., Lester D., Jia C. Associations between depression, anxiety, stress, hopelessness, subjective well-being, coping styles and suicide in Chinese university students. PLoS ONE. 2019;14 doi: 10.1371/journal.pone.0217372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Zhao J., Ma Z., McReynolds L.S., Lin D., Chen Z., Wang T., Wang D., Zhang Y., Zhang J., Fan F., Liu X. Mental health among college students during the COVID-19 Pandemic in China: a 2-wave longitudinal survey. J. Affect. Disord. 2021;281:597–604. doi: 10.1016/j.jad.2020.11.109. [DOI] [PubMed] [Google Scholar]
- Ma Z., Zhao J., Li Y., Chen D., Wang T., Zhang Z., Chen Z., Yu Q., Jiang J., Fan F., Liu X. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020;29:e181. doi: 10.1017/S2045796020000931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majumdar P., Biswas A., Sahu S. COVID-19 pandemic and lockdown: cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol. Int. 2020;37:1191–1200. doi: 10.1080/07420528.2020.1786107. 1-10. [DOI] [PubMed] [Google Scholar]
- McCracken L.M., Badinlou F., Buhrman M., Brocki K.C. Psychological impact of COVID-19 in the Swedish population: depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur. Psychiatry. 2020;63:e81. doi: 10.1192/j.eurpsy.2020.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren H., He X., Bian X., Shang X., Liu J. The protective roles of exercise and maintenance of daily living routines for Chinese adolescents during the COVID-19 quarantine period. J. Adolesc. Health. 2021;68:35–42. doi: 10.1016/j.jadohealth.2020.09.026. [DOI] [PubMed] [Google Scholar]
- Smilkstein G. Family APGAR analyzed. Fam. Med. 1993;25:293–294. [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Lwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The State Council Information Office of the People's Republic of China, 2020. Fighting Covid-19: china in Action.
- Tong X., An D., Mcgonigal A., Park S., D Z. Validation of the generalized anxiety disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy. Res. 2016;120:31–36. doi: 10.1016/j.eplepsyres.2015.11.019. [DOI] [PubMed] [Google Scholar]
- United Nations, 2020. Policy Brief: COVID-19 in an Urban World.
- Wang X., Hegde S., Son C., Keller B., Smith A., Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J. Med. Internet. Res. 2020;22:e22817. doi: 10.2196/22817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Chen H., Zhai S., Zhu Z., Huang S., Zhou X., Pan Y., Meng D., Yang Z., Zhao J., Fan F., Liu X. Is returning to school during the COVID-19 pandemic stressful? A study on immediate mental health status of Chinese college students. J. Affect. Disord. 2021;287:261–267. doi: 10.1016/j.jad.2021.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Bian Q., Zhao Y., Li X., Wang W., Du J., Zhang G., Zhou Q., Zhao M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry. 2014;36:539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- WHO, 2020. Coronavirus disease (COVID-2019) situation reports 2020.
- Xie Y.N. Reliability and validity of the simplified coping style questionnaire (SCSQ) Chin. J. Clin. Psychol. 1998;6:114–115. [Google Scholar]
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., Liu M., Chen X., Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child. Adolesc. Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet G.D., Powell S.S., Farley G.K., Werkman S., Berkoff K.A. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Please contact PhD Fang Fan at fangfan@scnu.edu.cn for data supporting the findings of the current study