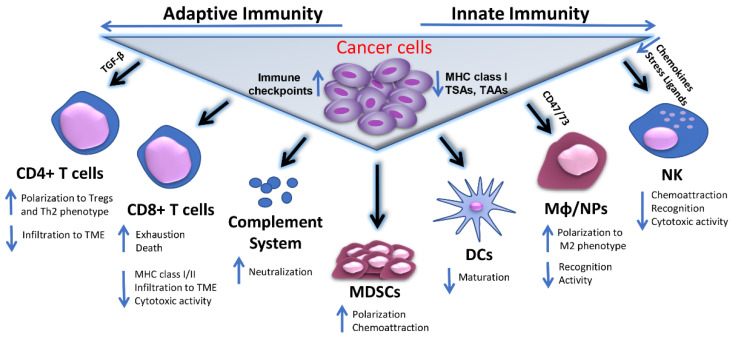
Figure 1.
Mechanisms of tumor immune evasion. Cancer cells escape host immunosurveillance by multiple mechanisms associated either with their phenotypic characteristics or with different immune cell populations of adaptive and innate immunity involved in the induction or suppression of a successful anti-tumor immune response. These mechanisms may include reduced expression of MHC class I, TAA, TSAs in cancer cells and/or upregulation of inhibitory immune checkpoint molecules on their surface. Alternatively, tumor cells may affect CD4+ and CD8+ T cell infiltration to TME by secreting factors, like TGF-β, while they can trigger the polarization of effector CD4+ T cells to Treg and/or Th2 phenotypes. In parallel, they can promote CTL exhaustion and apoptosis, accompanied by reduced CTL-associated expression of MHC class I/II complexes and cytotoxic activities. Concomitantly, the functions of innate immune cell populations, including Mφ, NPs and NK cells are significantly diminished, either due to accumulation of suppressing molecules like CD47 and CD73, or lack of potent chemoattractors and stress-related ligands, or inefficient target recognition. Cancer cells may also negatively interfere with DC maturation and complement dependent cytotoxicity (CDC), mainly by expression of neutralizing complement regulatory proteins. The immunosuppressive effects in TME are further augmented by cancer cell-mediated MDSCs recruitment and polarization to immunosuppressive cell phenotypes. Abbreviations used: MHC I/II, Major histocompatibility complex classI/or classII; TAA, Tumor associated antigens; TSA, Tumor specific antigens; MDSCs, Myeloid-derived suppressor cells; DCs, Dendritic cells; Mφ, Macrophages; NPs, Neutrophils; NK, Natural killers; TME, Tumor microenvironment; Tregs, T regulatory cells; Th2, Type 2 helper; CTL, Cytotoxic T lymphocyte; TGF-β, transforming growth factor beta.