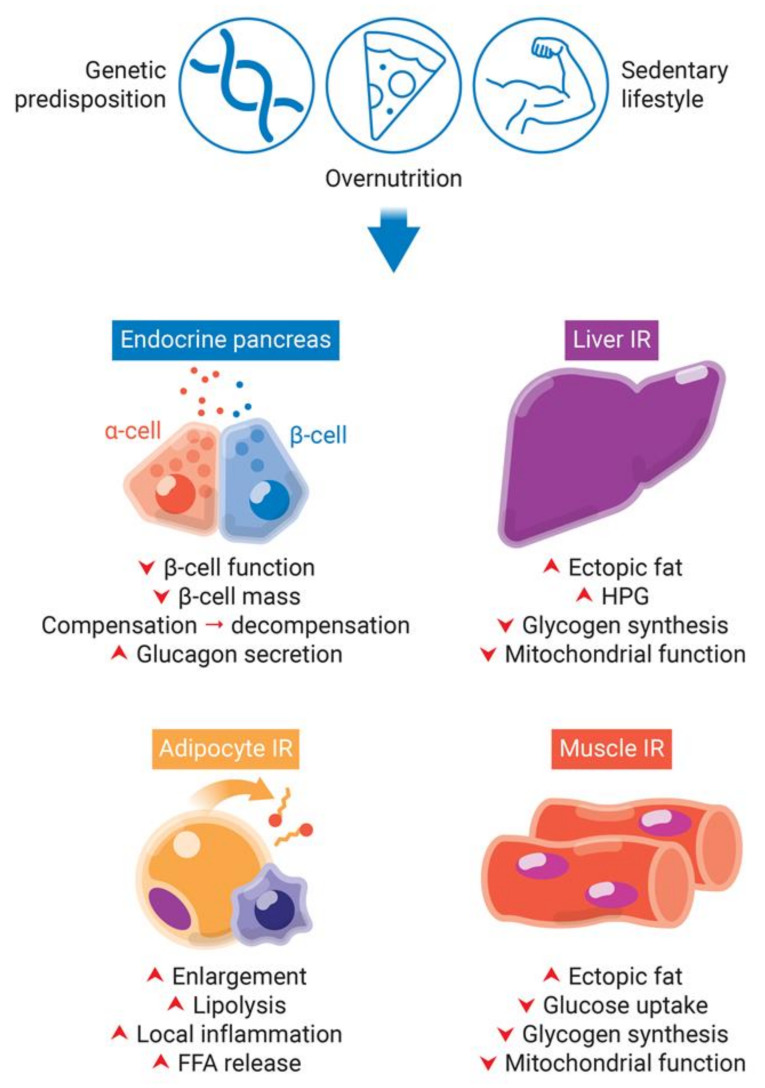
Figure 2.
Obesity-induced pancreatic β-cells dysfunction and insulin resistance (IR) in peripheral tissues. Genetic predisposition, overnutrition, and a sedentary lifestyle are involved in obesity and type 2 diabetes development. The lipotoxicity involved in chronic obesity and hyperglycemia leads to an increase of insulin demand due to IR in peripheral tissues. While in a first moment, β-cells try to compensate for IR by increasing insulin synthesis, they start to decompensate in late stages, with decrease of β-cell function and mass. IR in adipocytes eliminate insulin-induced repression of lipolysis. Impaired adipogenesis and dysfunctional hypertrophy of adipocytes increase plasma levels of free fatty acids (FFAs). Additionally, dysfunctional adipose tissue releases increased levels of insulin resistance-inducing pro-inflammatory adipokines, leading to local inflammation. The increased FFAs flux to the liver and skeletal muscle leads to increase of fat deposition, decrease of glycogen synthesis and mitochondrial dysfunction. Additionally, the hallmark of insulin resistance in the liver is increased hepatic glucose production (HPG).