Abstract
Background
The COVID-19 pandemic has had an adverse effect on the mental health of population worldwide. This study was conducted to systematically review the existing literature to identify the individuals at higher risk of anxiety with a view to provide targeted mental health services during this outbreak.
Methods
In this study, the studies focusing on anxiety prevalence among the general population during the COVID-19 pandemic were searched in the PubMed, EMBASE, Scopus, Web of Science (WoS) and Google Scholar from the beginning of Covid-19 pandemic to February 2021.
Results
103 studies constituting 140732 people included in the review. The findings showed that anxiety prevalence was 27.3% (95% CI, 23.7%; 31.2%) among general population while the prevalence in COVID-19 patients was 39.6% (95% CI, 30.1%; 50.1%). Anxiety was significantly higher among females and older adults (p≤0.05). In addition Europe revealed the highest prevalence of anxiety 54.6% (95% CI, 42.5%; 66.2%) followed by America 31.5% (95% CI, 19%; 47.5%) and Asia 28.3% (95% CI, 20.3%; 38%). In the general population the highest prevalence of anxiety was in Africa 61.8% (95% CI, 57%-66.4%) followed by America 34.9% (95% CI, 27.7%-42.9%), Europe 30.7% (95% CI, 22.8%-40%) and Asia 24.5% (95% CI, 20.7%-28.9%).
Conclusion
During the COVID-19 crisis, through identifying those who are more likely to be suffered from mental disorders at different layers of populations, it would be possible to apply appropriate supportive interventions with a view to provide targeted mental health services during the outbreak.
Keywords: Anxiety, People, Covid-19, Systematic review, Meta-analysis
1. Introduction
Given the growing COVID-19 pandemic almost all aspects of people's daily lives have been affected around the world in a dramatic way. The crisis presented an extraordinary challenge to healthcare industry, finance system, education, business and wider society (Stang, 2010). The devastating economic effects of COVID-19 created a disaster for the world population and put a considerable mental pressure on them. In fact, the pandemic is far from being just a medical phenomenon; rather it has negative impacts on the quality of life of people and their mental wellbeing (Cheung et al., 2012, Elbay et al., 2020). In face of these pressures, some of the individuals have experienced severe stress, fear of dying or getting sick (Beutel et al., 2017). Due to experiencing social distancing and quarantine they also reported significant levels of anxiety, irritation, uncertainty, insomnia and tension (Vardanjani et al., 2021, Tobaldini et al., 2017). Excessive social media use, low socioeconomic status, low resilience and lack of social support are other contributing factors that might enhance the risk of mental health disorders (Mallet et al., 2020).
Anxiety is a feeling of concern typically appeared as emotionally overreaction to situations that are only intuitively recognized as threatening. This feeling generally comes with muscular rigidity, agitation, exhaustion and attention deficit. Long-term effects of anxiety make chemical changes in the brain and release a surge of stress hormones which ultimately increase the symptoms of dizziness, headache, and depression in frequency or intensity (Cheng et al., 2020).
A study conducted in China among 1210 participants revealed that more than half of respondents reported a moderate or severe psychological impact of the COVID-19 crisis while 28.8% had moderate to severe level of anxiety symptoms (Zhang et al., 2020). Several studies also reported a high prevalence of psychological disorders in the general population during the pandemic (Louie et al., 2020, Huremović, 2019, Vindegaard and Benros, 2020, Cai et al., 2020, Pappa et al., 2020). Simultaneously, COVID-19 can result in some neurologic and mental health problems such as seizures, movement disorders, confusion, and stroke (da Silva and Neto, 2020). Furthermore, persistent anxiety weakens the immune system and increases vulnerability to illnesses, causing a greater risk of infection (Buselli et al., 2020).
Although the association between the COVID-19 pandemic and mental well-being has been researched in several studies it is still needed to comprehensively figure out the general statistics on the prevalence of anxiety globally and determine its main determinants in the general population and those infected with COVID-19 virus. Thus we conducted a systematic review of the existing literature conducted in different continents and the regions of World Health Organization (WHO) to provide useful data for health policymakers with a view to provide targeted mental health services during this outbreak. Furthermore, identification of individuals at higher risk of emotional suffering related to stressors can effectively play a key role in prevention and management of psychological distress.
2. Methods
2.1. Registration and reporting
The systematic review was registered with PROSPERO (CRD 42021238015) (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021238015) and was reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. (Moher et al., 2009)
2.2. Search terms
A comprehensive review of databases including EMBASE, Google Scholar, Scopus, PubMed and Web of Science was done between the beginning of Covid-19 pandemic and February 2021 to report the prevalence of anxiety in the general population. The search strategy included keywords of anxiety, population, patients, 2019-nCoV, SARS-CoV-2, COVID-19, Coronavirus, and all possible combinations explored from medical subject headings (MeSH). An example of complete search string in PubMed is (Angst [Title])) OR (Nervousness[Title])) OR (Hypervigilance[Title])) OR (Anxiousness[Title])) OR (social anxiety[Title])) OR (Anxiety[MeSH Terms])) OR (Anxiety[All Fields])) OR (Anxieties[All Fields])) AND (Social[Title])) OR (anxiety social[Title])) OR (social anxieties[Title])) AND (Covid-19[Title/Abstract])) OR (Covid 19[Title/Abstract])) OR (COVID-19 Virus Disease [Title/Abstract])) OR (COVID 19 Virus Disease [Title/Abstract])) OR (COVID-19 Virus Diseases [Title/Abstract])) OR (COVID-19 Virus Infection [Title/Abstract])) OR (COVID 19 Virus Infection [Title/Abstract])) OR (COVID-19 Virus Infections [Title/Abstract])) OR (2019-nCoV Infection [Title/Abstract])) OR (2019 nCoV Infection [Title/Abstract])) OR (2019-nCoV Infections [Title/Abstract])) OR (Coronavirus Disease-19 [Title/Abstract])) OR (Coronavirus Disease 19 [Title/Abstract])) OR (2019 Novel Coronavirus Disease [Title/Abstract])) OR (2019 Novel Coronavirus Infection [Title/Abstract])) OR (2019-nCoV Disease [Title/Abstract])) OR (2019 nCoV Disease [Title/Abstract])) OR (2019-nCoV Diseases [Title/Abstract])) OR (COVID19 [Title/Abstract])) OR (Coronavirus Disease 2019 [Title/Abstract])) OR (SARS Coronavirus 2 Infection [Title/Abstract])) OR (SARS-CoV-2 Infection [Title/Abstract])) OR (SARS CoV 2 Infection [Title/Abstract])) OR (SARS-CoV-2 Infections [Title/Abstract])) OR (COVID-19 Pandemic [Title/Abstract])) OR (COVID 19 Pandemic [Title/Abstract])) OR (COVID-19 Pandemics [Title/Abstract])). Through searching the databases 760 articles were found. After entering the records in to EndNote software and omitting the duplicates 617 Studies remained to be screened based on their title/ abstracts. To ensure the comprehensiveness of the search, the reference list of all included articles were reviewed.
2.2.1. Inclusion and exclusion criteria
Studies were included if they reported quantitative data on anxiety prevalence and its determining factors among the general population during the COVID-19 pandemic to find a set of articles based on the research keywords. Different types of observational studies including cross-sectional, prospective, case-study, and cohort were included. Furthermore articles with available full texts and English language published between the beginning Covid-19 pandemic and February 2021 were considered for further consideration. On the other hand, interventional studies, reviews, reports, letter to the editor, books, case-control, and commentaries were excluded from the review. Also studies with invalid methods and insufficient data, focusing on diagnostic approaches, treatment methods, and medication were kept out of review. Additionally, non-English papers published before the beginning Covid-19 pandemic or after February 2021 were not included.
2.2.2. Study selection
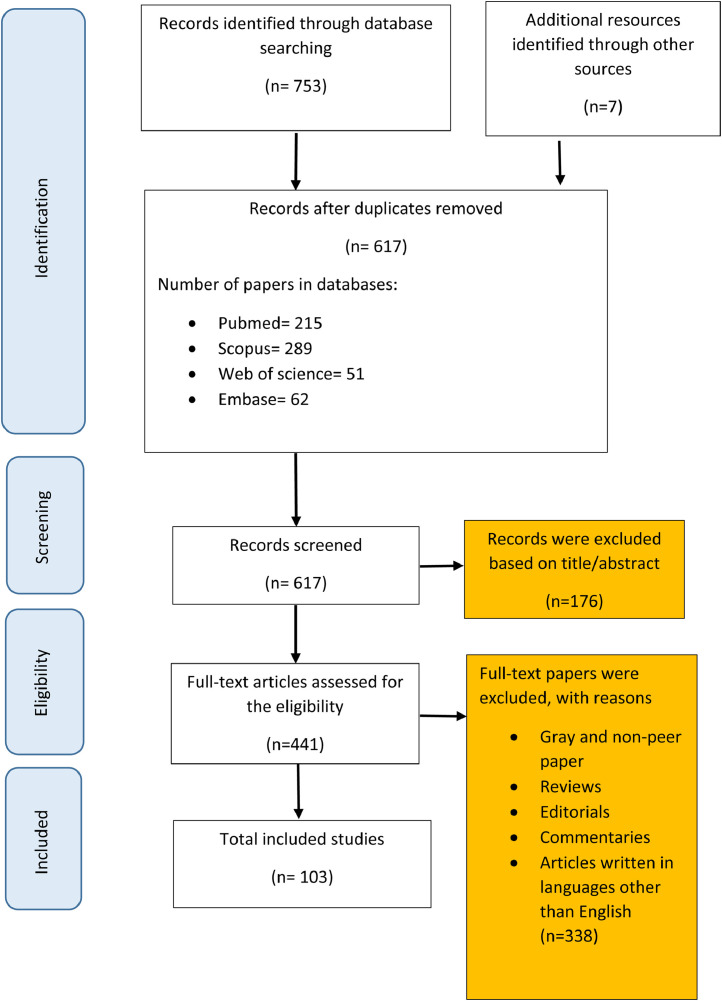
At the first step of searching process, 760 articles were found. After removing the duplicates the remaining 617 records were reviewed by two independent researchers according to their title/abstracts. Finally the full texts of 441 studies were systematically evaluated based on inclusion and exclusion criteria which consequently led to 103 records (Fig. 1 ).
Fig. 1.
Figure 1. Flow diagram of the review process (PRISMA)
2.2.3. Quality assessment
In order to evaluate the quality of the included articles in terms of methodological validity and robustness of findings Newcastle-Ottawa Scale (NOS) was used. The NOS consists of eight items categorized in to three subscales including selection, comparability, and outcome/ exposure with total maximum score of nine. A study with score≥7 has high quality while a record scored below 4 is considered to have low quality (Tan et al., 2020).Quality assessment was done by two independent reviewers and in case of any uncertainty the issue was resolved by a third investigator.
2.2.4. Data excretion
Data of included studies were entered in to a data extraction form by two independent investigators. The form items included author/ authors’ name, title of the study, year of publication, study setting, sample size, type of study, data collection tool, age, gender, occupation, the prevalence of anxiety, and contributing factors.
2.2.5. Statistical analysis
To estimate the pooled anxiety prevalence of included studies, random-effects model was used. The statistical heterogeneity was quantified by the I2 test. Furthermore due to the variability of estimates based on different study settings and socio-demographic characteristics of populations subgroup analyzes were used. Egger test was also applied to assess publication bias. Data was analyzed by Comprehensive Meta-Analysis and R software.
3. Results
Among 760 studies found in the initial search, 671 of them remained after removing the duplicates. After title and abstract analysis, we excluded 176 studies which following the review of remaining full text articles based on inclusion criteria, a total of 103 studies with the total sample size of 140732 included in the final review (Fig. 1).
3.1. Anxiety prevalence in infected and non-infected population
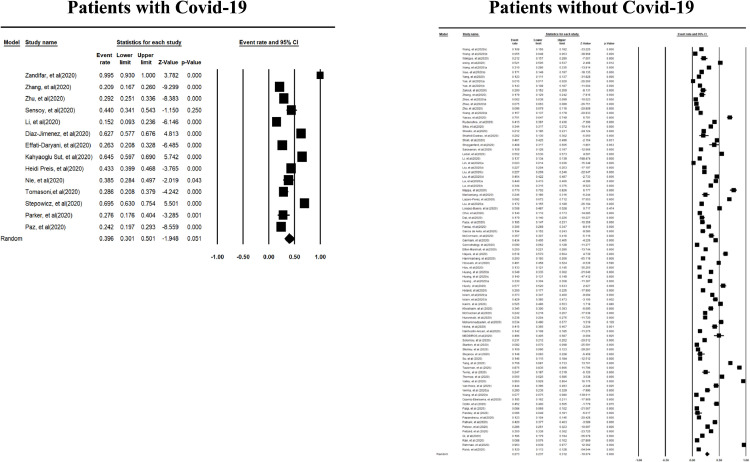
Meta-analysis of the point estimates of anxiety prevalence among general population was 27.3% (95% CI, 23.7%; 31.2%) while the prevalence in people infected by COVID-19 was 39.6% (95% CI, 30.1%; 50.1%) (Fig. 2 ).
Fig. 2.
Prevalence of anxiety among people with and without Covid-19.
3.2. Anxiety in infected people
3.2.1. Subgroup analysis for gender
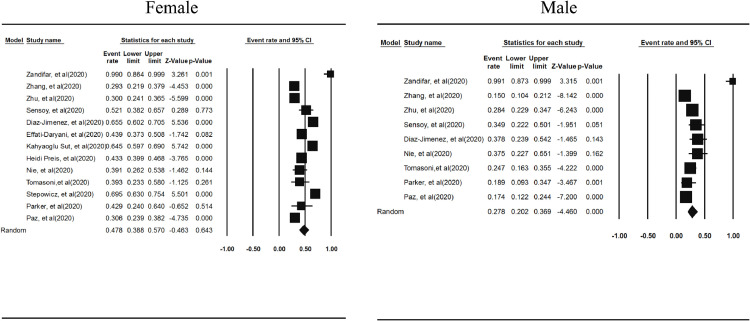
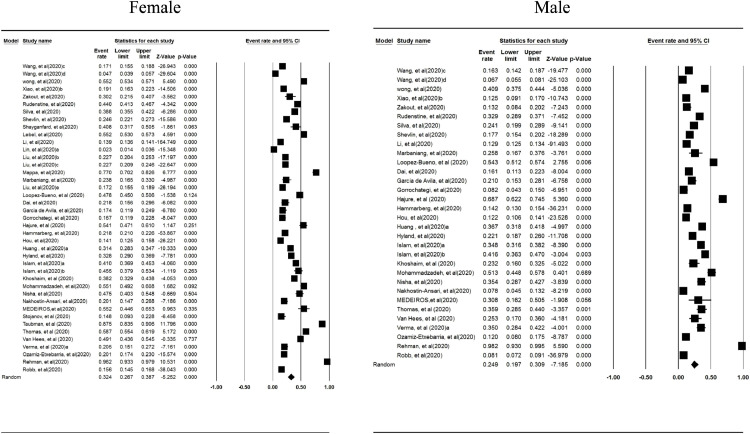
The subgroup analysis of the study population revealed that the prevalence of anxiety symptoms in females 47.8% (95% CI, 38.8%; 57%) was higher compared to men 27.8% (95% CI, 20.2%; 36.9%) (P-value<0.05) (Fig. 3 ).
Fig. 3.
Prevalence of anxiety among with Covid-19 based on gender.
3.2.2. Subgroup analysis for age
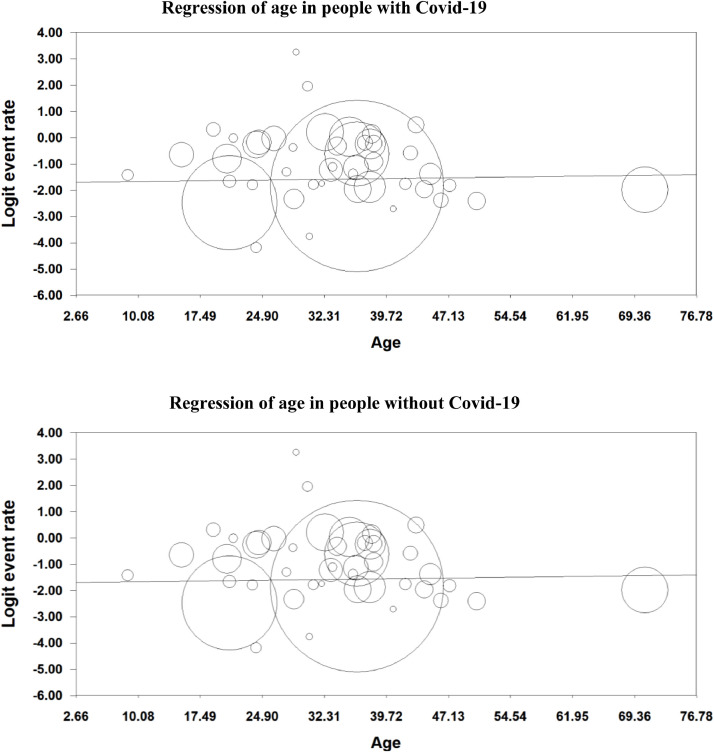
A meta-regression for age depicted that a unit of increase in patient's age decreased the prevalence of anxiety by -0.04% (95% CI, -0.05; -0.03). In fact a reverse relationship between anxiety in infected people and their age was affirmed in the review (P-value<0.05) (Fig. 4 ).
Fig. 4.
Meta-regression in people with and without Covid-19 based on age.
3.2.3. Subgroup analysis for continents and WHO regions
In subgroup comparisons based on continents Europe revealed the highest prevalence of anxiety 54.6% (95% CI, 42.5%; 66.2%) followed by America 31.5% (95% CI, 19%; 47.5%) and Asia 28.3% (95% CI, 20.3%; 38%). Furthermore, regarding WHO regions the highest prevalence of anxiety reported for EMRO 88.2% (95% CI, 1.4%; 10%) followed in descending order by EURO 28.3% (95% CI, 42.5%; 66.2%), PAHO 31.5% (95% CI, 19%; 47.5%) and WPRO 25.3% (95% CI, 18.2%; 33.9%) (Table 1 ).
Table 1.
Prevalence of Anxiety in People with and without Covid-19 based on Continents/WHO regions.
| Type of people | Continents/WHO regions | Effect size and 95% interval | Test of null (2-Tail) | ||||
|---|---|---|---|---|---|---|---|
| Prevalence | Lower limit | Upper limit | Z-value | P-value | |||
| Patients with Covid-19 | Continent | America | 0.315 | 0.190 | 0.475 | -2.257 | 0.024 |
| Asia | 0.283 | 0.203 | 0.380 | -4.147 | 0.000 | ||
| Europe | 0.546 | 0.425 | 0.662 | 0.743 | 0.458 | ||
| WHO | EMRO | 0.882 | 0.014 | 1.000 | 0.630 | 0.529 | |
| EURO | 0.546 | 0.425 | 0.662 | 0.743 | 0.458 | ||
| PAHO | 0.315 | 0.190 | 0.475 | -2.257 | 0.024 | ||
| WPRO | 0.253 | 0.182 | 0.339 | -5.102 | 0.000 | ||
| People without Covid-19 | Continent | Africa | 0.618 | 0.570 | 0.664 | 4.739 | 0.000 |
| America | 0.349 | 0.277 | 0.429 | -3.629 | 0.000 | ||
| Asia | 0.245 | 0.207 | 0.289 | -9.929 | 0.000 | ||
| Europe | 0.307 | 0.228 | 0.400 | -3.918 | 0.000 | ||
| WHO | AFRO | 0.618 | 0.570 | 0.664 | 4.739 | 0.000 | |
| EMRO | 0.423 | 0.312 | 0.543 | -1.252 | 0.210 | ||
| EURO | 0.359 | 0.261 | 0.470 | -2.468 | 0.014 | ||
| PAHO | 0.349 | 0.277 | 0.429 | -3.629 | 0.000 | ||
| SEARO | 0.373 | 0.311 | 0.439 | -3.690 | 0.000 | ||
| WPRO | 0.160 | 0.127 | 0.200 | -11.992 | 0.000 | ||
3.3. Anxiety in non-infected people
3.3.1. Subgroup analysis for gender
Findings revealed that the anxiety prevalence was higher among women 32.4% (95% CI, 26.7%-38.7%) compared to men 24.9% (95% CI, 19.7%-30.9%) (Fig. 5 ).
Fig. 5.
Prevalence of Anxiety in People without Covid-19 based on gender.
3.3.2. Subgroup analysis for age
A unit of increase in the population age increased the prevalence of anxiety by 0.03 (95% CI, 0.02-0.05) depicting that older adults were excessively affected by anxiety disorders (P-value<0.05). (Fig. 4)
3.3.3. Subgroup analysis for continents and WHO regions
The prevalence of anxiety among the general population during the COVID-19 pandemic in different continents showed that the highest prevalence of anxiety in Africa 61.8% (95% CI, 57%-66.4%) followed by America 34.9% (95% CI, 27.7%-42.9%), Europe 30.7% (95% CI, 22.8%-40%) and Asia 24.5% (95% CI, 20.7%-28.9%). Comparing different regions of WHO revealed that the highest prevalence of anxiety belonged to AFRO 61.8% (95% CI,57%-66.4%) followed in descending order by EMRO 42.3% (95% CI, 31.2%-54.3%), SEARO 37.3% (95% CI, 31.1%-43.9%), EURO 35.9% (95% CI, 26.1%-47%) and PAHO 34.9% (95% CI, 27.7%-42.9%). (Table 1)
3.3.4. Meta-analysis for different occupation
The subgroup analysis of the study population depicted that 55.9% of non-medical workers (95% CI, 29.6%-79.4%) had a higher prevalence of anxiety followed by pregnant women corresponding to 34.1% (95% CI, 21.1%-50.1%), ordinary people with 30.8% (95% CI, 25.7%-36.6%) and students 30.7% (95% CI, 22.2%-40.9%) (Table 2 ).
Table 2.
Prevalence of Anxiety in People without Covid-19 based on Occupation.
| Occupations | Effect size and 95% interval | Test of null (2-Tail) | Heterogeneity | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number Studies | Point estimate | Lower limit | Upper limit | Z-value | P-value | Q-value | df (Q) | P-value | I-squared | |
| Non-Medical Workers | 7 | 0.559 | 0.296 | 0.794 | 0.423 | 0.672 | 3781.885 | 6 | 0.00 | 99.84 |
| Ordinary people | 49 | 0.308 | 0.257 | 0.366 | -6.177 | 0.000 | 8549.950 | 48 | 0.00 | 99.44 |
| Patients(Other than Covid-19) | 5 | 0.386 | 0.249 | 0.543 | -1.428 | 0.153 | 96.879 | 4 | 0.00 | 95.87 |
| Pregnant | 11 | 0.341 | 0.211 | 0.501 | -1.949 | 0.051 | 1470.393 | 10 | 0.00 | 99.32 |
| Student | 23 | 0.307 | 0.222 | 0.409 | -3.583 | 0.000 | 3846.449 | 22 | 0.00 | 99.43 |
| Other | 4 | 0.482 | 0.235 | 0.518 | 0.923 | 0.356 | 45.220 | 3 | 0.00 | 93.37 |
4. Discussion
We have reviewed and analyzed 103 studies on prevalence of anxiety among population worldwide. To our knowledge, this is the first systematic review and meta-analysis providing a comprehensive and to date on the anxiety burden of COVID-19 on both infected and non-infected population. As we conducted meta-analysis of socio-demographic factors for the prevalence of anxiety in different continents and WHO regions, the findings are expected to provide reliable information for health policy makers in designing targeted mental health services for different population sub-groups. In this review, the prevalence of anxiety in COVID-19 patients and the entire non-infected population was reported to be 39.6% and 27.3% respectively; highlighting a moderately high rate of prevalence. According to a study conducted by Salari et al. the prevalence of anxiety due to the COVID-19 pandemic in the general population was 31.9% (Cai et al., 2020). Latest studies also affirmed the negative consequences of the pandemic on the mental health of population (Louie et al., 2020, Huremović, 2019, Chew et al., 2020). Correspondingly, they reported a higher prevalence of anxiety (39.4%) than the rate announced before the coronavirus epidemic (Cheng et al., 2020, Walton et al., 2020). Social isolation, quarantine and other restrictions enforced by governments to prevent the spread of the virus adversely affected the economic and financial status of countries and led to fear and anxiety in almost the whole world (Stang, 2010, Cheung et al., 2012).
COVID-19 has changed daily routine lives and influenced every aspects of life dramatically. Universities, schools and other educational institutions were closed in most of the countries influencing billions of learners globally. A considerable change in the learning method caused a great deal of stress among parents who have been forced to carry on some extent of homeschooling (Moher et al., 2009, Santabárbara et al., 2021). Furthermore, limited financial resources, unemployment, being overwhelmed with loss of control combined with remote work and a sense of unpredictability increased the feeling of anxiety, stress, or depression among older adults (Skoda et al., 2020). In our review, pregnant women were reported to be more vulnerable toward mental health problems needing social support services, and special education in the field of stress management. Similarly some of the literatures affirmed that the COVID-19 pandemic has reduced sense of control and increased anxiety in women limited access to accurate information on the impacts of COVID-19 during pregnancy (Santabárbara et al., 2021, Alshekaili et al., 2020). Reducing the negative impacts of misinformation on the population's emotion through the provision of accurate information about the pandemic in a proper way by health authorities can lead to psychological advantages and a sense of security in the general population. Ensuring adequate access to personal protective equipment (PPE) and promoting optimistic attitude toward the COVID-19 were among other influential strategies suggested in the literature to combat depression and anxiety (Cabarkapa et al., 2020).
In line with our findings recent studies revealed that females are more likely to be affected by psychological disorders compared to men (Nishimura et al., 2021, Nakhostin-Ansari et al., 2020). In fact in most of the literatures the prevalence of anxiety was higher in women during the COVID-19 crisis (Chew et al., 2020, Cabarkapa et al., 2020, Spoorthy et al., 2020, Jafri et al., 2020). The gender dissimilarities might be due to the higher genetic sensitivity of women toward disturbing situations, their hormonal imbalances or even a higher prevalence of pre-existing psychological disorders among them (Organization WH 2014, Andrews et al., 2001, Cotton et al., 2006).
Aging was another risk factor for increasing the level of anxiety in the population. Our results confirmed that the prevalence of anxiety was significantly higher in older adults. As older people are at higher risk of developing severe disease due to age-related physical and psychological vulnerability and underlying health problems they seem to have a higher level of psychological distress. Furthermore owing to uncertainty about the future and concerns over economic issues followed by the COVID-19 outbreak, they are adversely affected by revenue losses and financial pressures (Louie et al., 2020, Vindegaard and Benros, 2020, Jafri et al., 2020). To resolve the issue, psychologists, social workers and primary care physicians are suggested to provide mental health services to the public and promote their psychological well-being through advising them to avoid social isolation, and improve communication skills (Lai et al., 2020).
Finally our review revealed a considerable variation regarding the anxiety prevalence between continents. In Asian countries anxiety has been reported to be lower than others. The reason might be due to their family members who are mostly living together or next to each other representing a preference for a tightly-knit framework in the society. Thus during the pandemic such strong network of supportive families acted as an important preventive factor for social isolation resulting in decreased risk of mental health disorders (Organization WH 2014). On the other hand, Africa reported high burden of mental problems caused by a significant morbidity and mortality rate of COVID-19 which resulted in tighter coronavirus restrictions enforced by the government to implement quarantine, social distancing, and community containment. These limitations led to economic collapse which brought about financial concerns, and other destructive psychosocial impacts (Cheung et al., 2012, Elbay et al., 2020).
In response to heavy burden of mental disorders, health authorities should make more efforts in increasing public awareness of the COVID-19 pandemic to ensure a sense of security and emotional relief. In fact, promoting an optimistic attitude toward the COVID-19 has been recommended to avoid major psychological distress. Furthermore a proper system to generate and distribute required number of personal protective equipment during the pandemic was reported to be associated with a lower level of concern in the population (Chew et al., 2020, Cabarkapa et al., 2020).
5. Limitation
There are some limitations regarding the current review. First of all, lack of quantitative data about the prevalence of anxiety in some of the geographical regions concentrated our findings on some special countries including China which negatively affected the generalization of the results. Second, only studies published in English were included in the review which might result in language bias. Finally, non-uniform methods applied to evaluate the prevalence of anxiety might be another reason for methodological heterogeneity.
6. Conclusion
Anxiety symptoms can result in functional impairment and social deficiencies which are mainly associated with a considerable reduction in individuals’ quality of life. Rise in coronavirus hospitalizations and deaths can also deteriorate the mental well-being of population worldwide bringing them psychological distress and mental pressure. Thus, during the current crisis, it is essential to identify those who are more likely to be suffered from mental disorders at different layers of populations, in order to apply appropriate supportive interventions with a view to provide targeted mental health services during the outbreak.
Authorship contributions
Contributorship statement
1. Category
Conception and design of study: Samira Raoofi, Ahmad Ghashghaee, Fatemeh Pashazadeh Kan
Acquisition of data: Zahra Hoseinipalangi, Fatemeh Pashazadeh Kan, Samira Raoofi, Saghar Khani, Fatemeh Tajik, Neda Raoofi, Saba Ahmadi, Sepideh Aghalou
Analysis and/or interpretation of data: Hossein Hosseinifard, Sepide Rezaei, Fatemeh Torabi
2. Category
Drafting the manuscript: Sepide Rezaei, Ahmad Ghashghaee, Afsaneh Dehnad,
Revising the manuscript critically for important intellectual content: Sepide Rezaei, Afsaneh Dehnad, Ahmad Ghashghaee, Fatemeh Pashazadeh Kan
Approval of the version of the manuscript to be published: Samira Raoofi, Ahmad Ghashghaee, Sima Rafiei, Hossein Hosseinifard
Funding
Not applicable.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Declaration of Competing Interests
The authors declare that they have no competing interests.
Acknowledgements
Not applicable.
References
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- Cheung MWL, Ho RC, Lim Y, Mak A. Conducting a meta-analysis: basics and good practices. Int. J. Rheumatic Dis. 2012;15(2):129–135. doi: 10.1111/j.1756-185X.2012.01712.x. [DOI] [PubMed] [Google Scholar]
- Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beutel ME, Klein EM, Brähler E, Reiner I, Jünger C, Michal M, et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17(1):97. doi: 10.1186/s12888-017-1262-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vardanjani AE, Ronco C, Rafiei H, Golitaleb M, Pishvaei MH, Mohammadi M. Early hemoperfusion for cytokine removal may contribute to prevention of intubation in patients infected with COVID-19. Blood. Purif. 2021;50(2):257–260. doi: 10.1159/000509107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobaldini E, Costantino G, Solbiati M, Cogliati C, Kara T, Nobili L, et al. Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases. Neurosci. Biobehav. Rev. 2017;74:321–329. doi: 10.1016/j.neubiorev.2016.07.004. [DOI] [PubMed] [Google Scholar]
- Mallet J, Dubertret C, Le Strat Y. Addictions in the COVID-19 era: current evidence, future perspectives a comprehensive review. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2020 doi: 10.1016/j.pnpbp.2020.110070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng P, Xia G, Pang P, Wu B, Jiang W, Li Y-T, et al. COVID-19 epidemic peer support and crisis intervention via social media. Community Ment. Health J. 2020;56:786–792. doi: 10.1007/s10597-020-00624-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang SX, Sun S, Jahanshahi AA, Alvarez-Risco A, Ibarra VG, Li J, et al. Developing and testing a measure of COVID-19 organizational support of healthcare workers–results from Peru, Ecuador, and Bolivia. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louie PK, Harada GK, McCarthy MH, Germscheid N, Cheung JP, Neva MH, et al. The impact of COVID-19 pandemic on spine surgeons worldwide. Global Spine J. 2020;10(5):534–552. doi: 10.1177/2192568220925783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huremović D. Springer; 2019. Psychiatry of Pandemics: A Mental Health Response to Infection Outbreak. [Google Scholar]
- Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai W, Lian B, Song X, Hou T, Deng G, Li H. A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva FCT, Neto MLR. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2020 doi: 10.1016/j.pnpbp.2020.110062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buselli R, Corsi M, Baldanzi S, Chiumiento M, Del Lupo E, Dell'Oste V, et al. Professional quality of life and mental health outcomes among health care workers exposed to Sars-Cov-2 (Covid-19) Int. J. Environ. Res. Public Health. 2020;17(17):6180. doi: 10.3390/ijerph17176180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan BY, Chew NW, Lee GK, Jing M, Goh Y, Yeo LL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann. Intern. Med. 2020;173(4):317–320. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew NW, Ngiam JN, Tan BY-Q, Tham S-M, Tan CY-S, Jing M, et al. Asian-Pacific perspective on the psychological well-being of healthcare workers during the evolution of the COVID-19 pandemic. BJPsych Open. 2020;6(6) doi: 10.1192/bjo.2020.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. 2020;9(3):241–247. doi: 10.1177/2048872620922795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara J, Bueno-Notivol J, Lipnicki DM, Olaya B, Pérez-Moreno M, Gracia-García P, et al. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: a rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021 doi: 10.1016/j.pnpbp.2021.110244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skoda E-M, Bäuerle A, Schweda A, Dörrie N, Musche V, Hetkamp M, et al. Severely increased generalized anxiety, but not COVID-19-related fear in individuals with mental illnesses: a population based cross-sectional study in Germany. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020960773. 0020764020960773. [DOI] [PubMed] [Google Scholar]
- Alshekaili M, Hassan W, Al Said N, Al Sulaimani F, Jayapal SK, Al-Mawali A, et al. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ open. 2020;10(10) doi: 10.1136/bmjopen-2020-042030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabarkapa S, Nadjidai SE, Murgier J, Ng CH. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain, Behav. Immunity-Health. 2020 doi: 10.1016/j.bbih.2020.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishimura Y, Ochi K, Tokumasu K, Obika M, Hagiya H, Kataoka H, et al. Impact of the COVID-19 pandemic on the psychological distress of medical students in japan: cross-sectional survey study. J. Med. Internet Res. 2021;23(2):e25232. doi: 10.2196/25232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakhostin-Ansari A, Sherafati A, Aghajani F, Khonji MS, Aghajani R, Shahmansouri N. Depression and anxiety among Iranian Medical Students during COVID-19 pandemic. Iranian J. Psychiatry. 2020;15(3):228. doi: 10.18502/ijps.v15i3.3815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–a review. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jafri L, Ahmed S, Siddiqui I. Impact of COVID-19 on laboratory professionals-A descriptive cross sectional survey at a clinical chemistry laboratory in a developing country. Ann. Med. Surgery. 2020;57:70–75. doi: 10.1016/j.amsu.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization WH. World Health Organization, Geneva, Switzerland. 2014.
- Andrews G, Issakidis C, Carter G. Shortfall in mental health service utilisation. Br. J. Psychiatry. 2001;179(5):417–425. doi: 10.1192/bjp.179.5.417. [DOI] [PubMed] [Google Scholar]
- Cotton SM, Wright A, Harris MG, Jorm AF, McGorry PD. Influence of gender on mental health literacy in young Australians. Austr. New Zealand J. Psychiatry. 2006;40(9):790–796. doi: 10.1080/j.1440-1614.2006.01885.x. [DOI] [PubMed] [Google Scholar]
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. -e. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.