Abstract
Purpose:
To study the current management trends for extraperitoneal bladder injuries (EBI) and evaluate the use of operative repair (OR) versus catheter drainage (CD), and the associated complications with each approach.
Methods:
We prospectively collected data on bladder trauma from 20 Level-1 trauma centers across the United States from 2013–2018. We excluded patients with intraperitoneal bladder injury and those who died within 24 hours of hospital arrival. We separated EBI patients into two groups (CD vs. OR) based on their initial management within the first four days and compared the rates of bladder injury-related complications among them. Regression analyses were used to identify potential predictors of complications.
Results:
From 323 bladder injuries, we included 157 patients with EBI. Concomitant injuries occurred in 139 (88%) patients with pelvic fracture seen in 79%. Sixty-seven patients (43%) initially underwent OR for their EBI. The three most common reasons for OR were: severity of injury or bladder neck injury (40%), injury found during laparotomy (39%), and concern for pelvic hardware contamination (28%). Significant complications were identified in 23% and 19% of the CD and OR groups, respectively (p=0.55). The only statistically significant predictor for complications was bladder neck or urethral injury (RR 2.69; 95% 1.21–5.97; p=0.01).
Conclusions:
In this large multi-institutional cohort, 43% of patients underwent surgical repair for initial management of EBI. We found no significant difference in complications between the initial management strategies of CD and OR. The most significant predictor for complications was concomitant urethral or bladder neck injury.
Keywords: Epidemiology, urinary bladder, wounds and injuries, trauma centers, multicenter study
Introduction:
Bladder trauma is the second most common genitourinary injury and occurs in about 4% of patients with traumatic pelvic fractures.1–3 The majority of bladder injuries are extraperitoneal and are accompanied by other abdominal organ injuries.4, 5 Intraperitoneal bladder injuries are usually surgically repaired, however, the role of surgical repair for extraperitoneal bladder injuries (EBI) is not well-defined.
Current guidelines from the American Urological Association (AUA) recommend catheter drainage (CD) for the initial management of uncomplicated, blunt EBI.6 The relative indications for operative repair (OR) of EBI include concomitant injuries to the bladder neck, rectum, or vagina, bony spicules within the bladder, and persistent gross hematuria with clots.6, 7 However, data are conflicting regarding the utility of OR for EBI and the associated complications of either CD or OR. For instance, the University of Texas at Houston reported their 7-year data in which 23% of their 39 EBI patients underwent OR.8 Additionally, in a more recent series of 80 EBI patients from the Vanderbilt University, 30% underwent OR as a secondary procedure during non-urologic interventions.9
Research on EBI is mostly limited to retrospective, single-institutional studies, or studies utilizing administrative data such as the National Trauma DataBank (NTDB). We sought to understand the current management trends and outcomes of CD versus OR for EBI in a large contemporary multi-institutional cohort.
Methods:
This study is part of the Multi-institutional Genito-Urinary Trauma Study (MiGUTS), which is a partnership between the American Association for the Surgery of Trauma (AAST) Multi-institutional Trials Committee, and the Trauma and Urologic Reconstruction Network of Surgeons (TURNS). For the current study, bladder trauma data were included from 20 level-1 trauma centers participating in phase-1 (2014–2017) or phase-2 (2013–2018) of the MiGUTS project (a full list of participating centers and collaborators can be found at http://www.turnsresearch.org/page/genito-urinary-trauma-study-miguts-bladder).
We excluded patients with an intraperitoneal bladder injury component and those who died within 24 hours of admission. The following clinical variables were considered: age, sex, trauma mechanism (blunt vs. penetrating), presence of concomitant injuries (solid organ, gastrointestinal, spinal cord, major vascular, and pelvic fracture), injury severity score (ISS; an anatomical scoring system ranging from 0–75 reflecting overall injury severity in polytrauma patients and calculated based upon abbreviated injury scores from six body regions)10, exploratory laparotomy for non-urologic reasons, pelvic orthopedic interventions (open reduction and internal fixation [ORIF], closed reduction and internal fixation [CRIF], and external fixation of pelvis), hospital length of stay, and complications. Significant complications were defined as the presence of the following urologic or orthopedic conditions: pelvic infection/urinoma, persistent urinary extravasation, urinary tract fistula, non-union fractures, hardware infection or removal, and pelvic osteomyelitis. Operative variables included type of physician performing the bladder repair (urologist vs. trauma/acute care surgeon), and the main reasons for repair, which included the ability to choose one or more of the following options: discovered during laparotomy and repaired at the time of exploration; repaired at the time of pelvic fixation due to concern over urinary leakage and contamination of pelvic hardware; hematuria and blood clots hindering urine drainage; severity of extraperitoneal injury (large injury, bladder neck injury, other); and concomitant rectal, bowel, or vaginal injury. When available, follow-up imaging data were collected to assess healing of bladder injury. Persistent urinary extravasation was defined as any indication of urine leak from the bladder injury in the follow-up images regardless of timing of the study. Time to catheter removal was recorded if documented. Patients were grouped as either CD or OR based upon their initial management within the first four days after hospital admission. We compared clinical variables, and urologic and orthopedic complications between these two groups.
Data are presented as mean (SD) or median (25th–75th interquartile range [IQR]) when appropriate. Independent samples t-test (or Wilcoxon rank-sum test when appropriate) and chi-squared test (or Fisher’s exact test when appropriate) were used to compare continuous and categorical variables between the management groups, respectively. Mixed-effect univariable Poisson regression models, with clustering by facility and robust estimator for error, were developed to assess the associations between different predictors and complications after EBI. Results from regression models are reported as risk ratios (RR) with 95% confidence intervals (CIs). The multivariable model included bladder management as well as variables with a P-value<0.1 from the univariable analyses. As the number of outcomes were small, we relaxed the rule of ten events per predictor to include 5–6 variables in the multivariable model.11 All statistical analyses were conducted using STATA 15 (Stata Corp, College Station, TX, USA) and a P-value<0.05 was considered statistically significant.
Results:
We identified 323 bladder injuries of which 164 (51%) involved only EBI. After excluding those who died within 24 hours of hospital arrival, 157 patients with EBI were included. The mean age was 40.6 (SD: 17.5) years, 106 (68%) were male, and 121 (77%) had a blunt mechanism of injury. Mean ISS was 26.1 (SD: 12.5) and concomitant injuries occurred in 139 (88%) with pelvic fracture seen in 124 (79%). Pelvic fracture related orthopedic procedures were performed in 85 (54%) patients and included: ORIF (n=57, 47%), CRIF (n=35, 29%), and external fixation (n=29, 24%) [some patients underwent more than one procedure]. There were three additional mortalities in our cohort of EBI patients after the initial exclusion step; none were related to the genitourinary injuries. Patients who underwent surgical repair were younger, more were male, had a higher rate of penetrating and bladder neck injury, had lower ISS, and had lower rates of pelvic fracture compared to the non-operative group. Patient and injury characteristics are summarized in Table-1.
Table-1.
Demographics and management of extraperitoneal traumatic bladder injury
| Total (n=157) |
Non-operative (n=90) |
Operative Repair (n=67) |
p value * | |
|---|---|---|---|---|
| Age, mean (SD), y | 40.6 (17.5) | 44.7 (18.6) | 35.0 (14.2) | <0.001 |
| Male sex, n (%) | 106 (68) | 54 (60) | 52 (78) | 0.02 |
| Type of injury | 0.001 | |||
| Blunt | 121 (77) | 83 (92) | 38 (57) | |
| Penetrating | 36 (23) | 7 (8) | 29 (43) | |
| ISS, mean (SD) | 26.1 (12.5) | 28.4 (13.1) | 23.0 (11.2) | 0.01 |
| Concomitant injuries, n (%) | 139 (88) | 82 (91) | 57 (85) | 0.24 |
| Pelvic fracture | 124 (79) | 79 (89) | 45 (67) | 0.001 |
| Bladder neck injury | 19 (12) | 5 (6) | 14 (21) | 0.004 |
| Urethral injury | 15 (10) | 7 (8) | 8 (12) | 0.38 |
| Colon injury | 16 (10) | 6 (7) | 10 (15) | 0.09 |
| Rectal injury | 18 (11) | 4 (4) | 14 (21) | 0.001 |
| Non-urologic operation | ||||
| Exploratory laparotomy | 65 (41) | 15 (17) | 50 (75) | <0.001 |
| Pelvic orthopedic procedure | 85 (54) | 52 (58) | 33 (49) | 0.29 |
| Length of stay, median (IQR), d | 12 (6–21) | 12 (6–20) | 12 (6–21) | 0.81 |
| ICU Length of stay, median (IQR), d | 6 (3–13) | 5 (3–13) | 6 (2–15) | 0.97 |
| Time to catheter removal, median (IQR), d | 17 (13–24) | 18 (14–27) | 16 (12–22) | 0.16 |
| Urologic complications, n (%) | 27 (17) | 16 (18) | 11 (16) | 0.82 |
| Orthopedic complications, n (%) | 10 (6) | 5 (6) | 5 (7) | 0.74 |
comparisons made between non-operative and surgical repair management groups
Sixty-seven (43%) patients underwent surgical repair of their EBI. The median time to repair was 5.4 hours (IQR: 1.7–22.7). Urologists repaired the bladder in 48 (72%) cases, and the remainder were repaired by trauma/acute care surgeons. Time to catheter removal was not significantly different between the CD and OR groups (18 vs. 16 days, p=0.16, data available for 98 [62%] patients). Fifty-one patients (76%) had information available on follow-up imaging: fluoroscopic cystogram was performed in 33 (65%), compared to CT cystogram in 18 (35%). The three leading reasons for EBI repair were: severity of the injury or bladder neck injury (40%), injury found during laparotomy (39%), and concerns about pelvic hardware contamination (28%). The top three reasons were similar with different orders among urologic vs. non-urologic surgeons who performed the repairs (the top reason being severity of injury for urologists and injuries found during laparotomy for non-urologists). Table-2 describes the surgically repaired cohort.
Table-2.
Characteristics of the surgical repair cohort
| N=67 | |
|---|---|
| Time to initial repair, median (IQR), hours | 5.4 (1.7–22.7) |
| Reason for initial repair, n (%) | |
| Severity of injury/bladder neck injury | 27 (40) |
| Injury found during laparotomy | 26 (39) |
| Concern for pelvic hardware contamination | 19 (28) |
| Concomitant gastrointestinal or vaginal injury | 11 (16) |
| Hematuria or blood clots obstructing urine drainage | 8 (12) |
| Type of physician performing the initial repair, n (%) | |
| Urologist | 48 (72) |
| Acute care surgeon/general surgeon | 16 (24) |
| Not recorded | 3 (4) |
| Follow-up imaging modality, n (%) | |
| Fluoroscopic cystogram | 33 (65) |
| CT cystogram | 18 (35) |
| Persistent urinary extravasation, n (%) | 9 (13) |
| Management of persistent extravasation, n (%) | |
| Additional bladder repair(s) | 2 (22) |
| Continued Foley drainage | 3 (33) |
| Suprapubic tube/percutaneous nephrostomy | 4 (45) |
| Patients with urologic complications, n (%) | 11 (16) |
| Clavien-Dindo I | 2 |
| Clavien-Dindo IIIa | 4 |
| Clavien-Dindo IIIb | 5 |
| Patients with orthopedic complications, n (%) | 5 (7) |
| Clavien-Dindo IIIb | 5 |
We found no significant difference in the total bladder-related urologic or orthopedic complications between the CD and OR groups (23% vs. 19%; p=0.55). Table 3 compares the urologic and orthopedic complications between the groups. The significant univariable predictors for complications included: age and associated bladder neck/urethral injury. Other factors including non-operative management, ISS, pelvic fracture, and pelvic orthopedic procedures were not significant predictors of bladder-related complications (Table-4). In the multivariable analysis, only presence of bladder neck/urethral injury was a significant predictor for complications after EBI (RR 2.69; 95% 1.21–5.97; p=0.01) [Table-4]. Overall, 19 patients had bladder neck injury. Of the 5 EBI with bladder neck injury in the CD group, three were eventually repaired due to persistent leak or more complex injuries (including one with bone fragments in bladder). Of the 14 patients with bladder neck injury in the OR group, 3 had persistent leak that was healed with temporary urinary diversion and/or continued catheter drainage, three had more complex courses with fistulas, urinary incontinence, and multiple or failed repairs, and the other eight had no complications.
Table-3.
Bladder-injury related significant urologic and orthopedic complications in patients with extra-peritoneal bladder injury separated by management
| Non-operative (n=90) |
Surgical Repair (n=67) |
p value | |
|---|---|---|---|
| Total patients with complications, n (%) | 21 (23) | 13 (19) | 0.55 |
| No. of urologic complications, n (%) | |||
| Pelvic infection/Urinoma | 1 (1) | 4 (6) | 0.16 |
| Persistent urinary extravasation | 16 (18) | 9 (13) | 0.46 |
| Urinary tract to skin fistula | 1 (1) | 3 (4) | 0.31 |
| No. of orthopedic complications, n (%) | |||
| Non-union | 1 (1) | 1 (1) | 0.99 |
| Hardware infection/removal | 4 (4) | 5 (7) | 0.50 |
| Pelvic osteomyelitis | 0 (0) | 2 (3) | 0.18 |
Table-4.
Regression analyses of factors predicting complications after extra-peritoneal bladder injury
| Univariable | Multivariable | |||
|---|---|---|---|---|
|
| ||||
| RR (95% CIs) | p value | RR (95% CIs) | p value | |
| Age (per year) | 1.02 (1.00–1.04) | 0.05 | 1.02 (0.99–1.04) | 0.16 |
| Male sex | 1.01 (0.50–2.01) | 0.99 | --- | --- |
| ISS (per unit) | 1.02 (1.00–1.05) | 0.07 | 1.01 (0.98–1.04) | 0.41 |
| Penetrating Trauma | 0.32 (0.10–1.05) | 0.06 | 0.68 (0.15–2.94) | 0.61 |
| Pelvic fracture | 2.67 (0.81–8.72) | 0.11 | --- | --- |
| Bladder neck/urethral injury | 3.02 (1.49–6.11) | 0.002 | 2.69 (1.21–5.97) | 0.01 |
| Colon/rectal injury | 1.25 (0.54–2.87) | 0.60 | --- | --- |
| Pelvic orthopedic procedure | 2.03 (0.97–4.25) | 0.06 | 1.31 (0.55–3.12) | 0.53 |
| Non-operative management | 1.20 (0.60–2.40) | 0.60 | 1.20 (0.53–2.72) | 0.66 |
Persistent urinary extravasation was identified in 25 (20%) of 122 patients with EBI who had follow-up imaging, with 16 (23%) in the CD cohort and 9 (18%) in the OR group. Of the 9 patients from the operative cohort with persistent leak, two required additional repairs, three were managed with continued catheter drainage, and four needed additional drainage tubes placed (supra-pubic or nephrostomy tubes). Of the 16 patients who had persistent leak in the CD group, 10 were managed with continued catheter drainage and the median time to resolution of leak was 28 days after injury. A total of six patients had delayed repair after initial management of CD. Of these, two had bone fragments identified at follow-up imaging and one patient had cutaneous fistula formation to the labia; the other three did not have further details regarding the circumstances surrounding the repair. Figure-1 depicts a flow chart for management of persistent urinary extravasation in our cohort.
Figure-1.
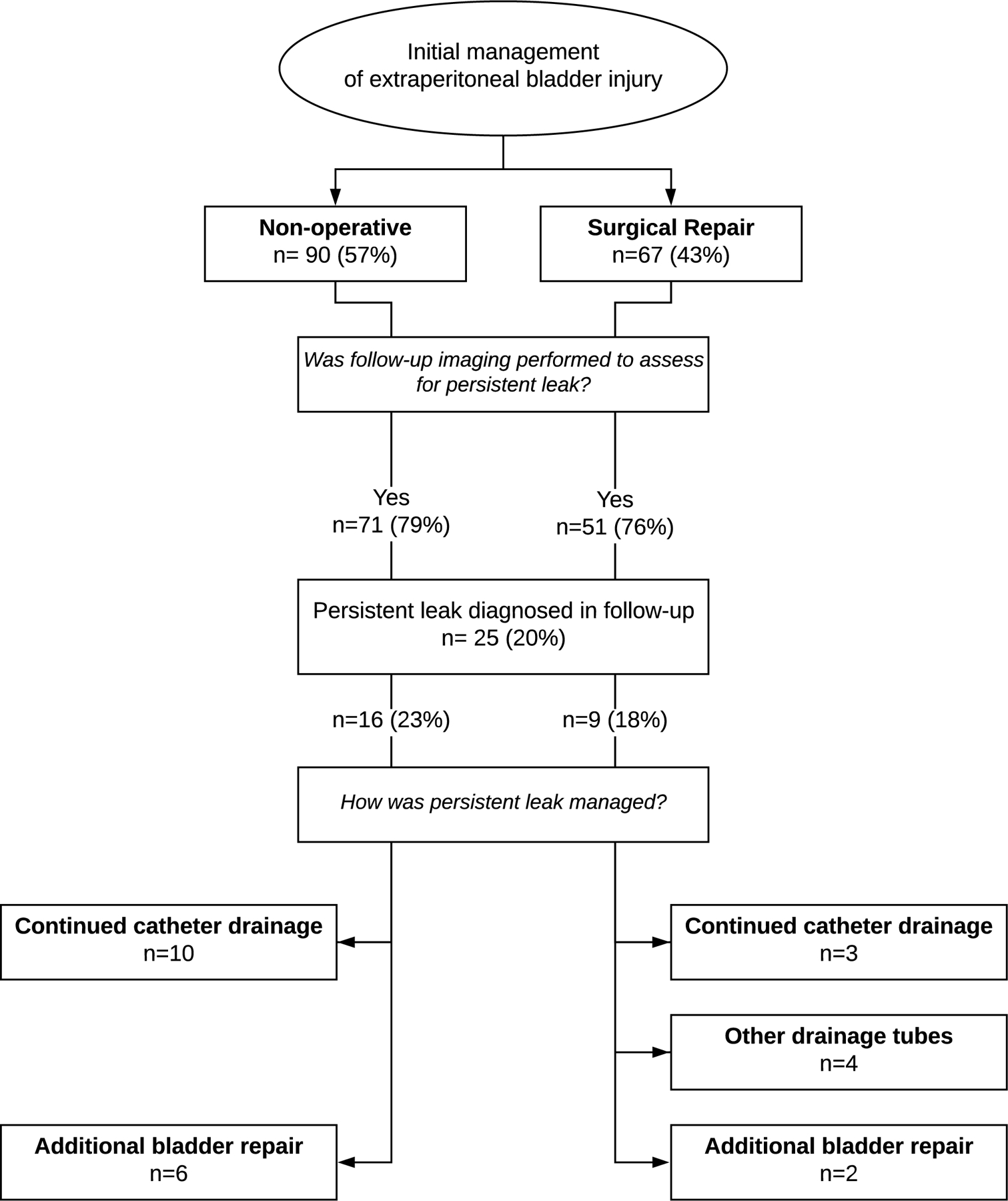
Flow diagram – Management of extraperitoneal bladder injury with persistent urinary extravasation on follow up imaging
Discussion:
In this contemporary multi-institutional cohort of bladder trauma, 51% of injuries were extraperitoneal, of which 43% underwent surgical repair as their initial management. We found that bladder neck/urethral injury was associated with a higher bladder-related complication rate after EBI. The complication rate was not different in respect to the initial management strategy of CD or OR, although this may reflect selection bias with the complexity of injuries being more severe in the OR group.
Studies from the NTDB demonstrated a 50% rate of bladder repair in adults with EBI with an association between bladder repair and better survival.4, 12 In the NTDB, the mortality rate for EBI was 10.8% compared to our rate of 6.1%. However, all 10 mortalities in our cohort occurred due to the severity of concomitant injuries with seven within the first 24 hours. Possible explanations for the associations observed in the NTDB is inclusion of intraperitoneal injuries and that severely injured patients may not have undergone bladder repair due to the higher-priority injuries or poor prognosis, and then died at a higher rate without bladder repair.
Neither CD nor OR was free from complications, however, we found no difference in the overall urologic or orthopedic complication rates between the two groups. Despite a large number of EBI patients included in our series, our study might be underpowered to address this question given the small number of complications in each group. However, our 23% complication rate in the CD group is consistent with a previous report on 29 EBI patients treated with CD alone that showed a 26% complication.13 A more contemporary series suggested a reduced rate of major complications in EBI patients who underwent bladder repair at the time of ORIF or exploratory laparotomy compared to those who underwent these procedures without repair (4% vs 30% complication rate, respectively).9 However, similar to our study, the conclusions could have easily been affected by just 1 or 2 cases due to the low numbers of complications and rarity of EBI.
Complex EBI injuries include concomitant injuries to the bladder neck, rectum, or vagina, bony spicules within the bladder, or persistent gross hematuria with clots.6, 7 The diagnosis of complex EBI is nuanced and depends on multiple factors, including imaging modality (CT vs. plain X-ray), and the quality and timing of the imaging study. In our study, six patients who were first managed with CD, ultimately underwent OR due to persistent urinary extravasation. Two patients had bone spicules in the bladder and likely would have benefited from early repair if this had been diagnosed on original imaging. We found a significant association between bladder-related complications and the presence of bladder neck/urethral injuries. These concomitant lower tract injuries may lead to increased urinary extravasation, prolonged exposure of the pelvis to urine, or could increase the complexity of both the urologic or orthopedic surgeries. Both the AAST and the AUA guidelines recommend bladder repair for patients with concomitant bladder neck injury.6, 14 However, in our cohort, five of the 19 patients with bladder neck injury identified were initially managed with CD. Although we did not have details on the reasons for this approach, three of these five patients eventually underwent a bladder repair for persistent urinary extravasation. Additionally, about half of patients with bladder neck injury who initially underwent OR, had delayed healing or a complicated recovery course. These observations stress the importance of diagnosing bladder neck injury so initial management with CD is truly reserved for uncomplicated injuries. CT cystogram with initial non-contrast view and retrograde filling of the bladder with more than 300cc is the gold standard to assess for bladder injury and provides the most anatomic detail.15
Previous orthopedic and urologic literature, including the AUA trauma guidelines, has stressed EBI undergo bladder repair if orthopedic hardware is implanted, especially if ORIF is performed due to the potential hardware contamination with urine.6, 16, 17 Of note, in our series, 42% of patients who underwent ORIF did not undergo bladder repair (either immediate or delayed). Rates of orthopedic complications were not different in ORIF patients who underwent CD vs. OR. Although some of these ORIF procedures might have only involved screw placement and some might have been performed after partial healing of bladder injuries, this finding raises the question of whether immediate bladder repair is needed for all patients undergoing pelvic ORIF. However, concern for pelvic hardware contamination was still the third most common reason reported for initial repair of EBI in our cohort. This approach might find root in the literature recommending EBI repair at the time of ORIF, although the evidence behind these recommendations is weak.13, 16–18
This study has similar limitations to any non-randomized, cohort study, and there is a possibility of selection bias for treatment groups. We suspect more complex injuries undergo repair at a higher rate and thus a comparable rate of complications between patients managed with CD and OR may not be valid. Currently, a robust method of classifying complex EBI injuries is lacking, and until a strategy is developed to better stratify severity of EBI, this limitation will remain a confounder of studies of this injury pattern. Furthermore, the initial management and follow-up protocols were not standardized across all centers. Thus, surgical technique, catheter type and duration, and the use of post-operative imaging might vary across the centers. These differences could be based on local trauma protocols, the type of surgeon managing the injury (trauma/acute care surgeon vs. urologist) and individual surgeons experience and preferences. Despite these limitations, our study does reflect contemporary real-world management of EBI from 20 Level-1 trauma centers from across the United States and is the largest contemporary study on management of EBI. The multi-institutional nature of the data and not relying upon historic data spanning time periods where genitourinary trauma management has changed substantially, is another strength of this study.
Conclusion:
In this large multi-institutional cohort, we found that 43% of patients underwent operative repair for initial management of EBI. We did not find any significant difference in pelvic orthopedic or urologic complications between the initial management strategies of catheter drainage and operative repair, but given the possible selection bias in management decisions, these results should be interpreted with caution. The most significant predictor for complications was concomitant urethral or bladder neck injury. We recommend adhering to the current guidelines about operative repair of EBI in presence of bladder neck injuries. More data is needed on the timing and type of follow-up imaging and also the necessity of bladder repair in patients with orthopedic hardware.
Acknowledgments
Disclosure: This study was not directly supported by any industrial or federal funds. The investigation was in part supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067-05 (formerly 8UL1TR000105 and UL1RR025764).
Footnotes
Conflicts of Interest: None
References:
- 1.McGeady JB, Breyer BN: Current epidemiology of genitourinary trauma. Urol Clin North Am, 40: 323, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bjurlin MA, Fantus RJ, Mellett MM et al. : Genitourinary injuries in pelvic fracture morbidity and mortality using the National Trauma Data Bank. J Trauma, 67: 1033, 2009 [DOI] [PubMed] [Google Scholar]
- 3.Johnsen NV, Dmochowski RR, Young JB et al. : Epidemiology of Blunt Lower Urinary Tract Trauma With and Without Pelvic Fracture. Urology, 102: 234, 2017 [DOI] [PubMed] [Google Scholar]
- 4.Deibert CM, Spencer BA: The association between operative repair of bladder injury and improved survival: results from the National Trauma Data Bank. J Urol, 186: 151, 2011 [DOI] [PubMed] [Google Scholar]
- 5.Phillips B, Holzmer S, Turco L et al. : Trauma to the bladder and ureter: a review of diagnosis, management, and prognosis. Eur J Trauma Emerg Surg, 43: 763, 2017 [DOI] [PubMed] [Google Scholar]
- 6.Morey AF, Brandes S, Dugi DD 3rd et al. : Urotrauma: AUA guideline. J Urol, 192: 327, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lucas JW, Chen A, Simhan J: The Role of Surgery in the Management of Complex Extraperitoneal Bladder Injury. Current Trauma Reports, 3: 265, 2017 [Google Scholar]
- 8.Corriere JN Jr., Sandler CM: Management of the ruptured bladder: seven years of experience with 111 cases. J Trauma, 26: 830, 1986 [DOI] [PubMed] [Google Scholar]
- 9.Johnsen NV, Young JB, Reynolds WS et al. : Evaluating the Role of Operative Repair of Extraperitoneal Bladder Rupture Following Blunt Pelvic Trauma. J Urol, 195: 661, 2016 [DOI] [PubMed] [Google Scholar]
- 10.Baker SP, O’Neill B, Haddon W Jr. et al. : The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma, 14: 187, 1974 [PubMed] [Google Scholar]
- 11.Vittinghoff E, McCulloch CE: Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol, 165: 710, 2007 [DOI] [PubMed] [Google Scholar]
- 12.Deibert CM, Glassberg KI, Spencer BA: Repair of pediatric bladder rupture improves survival: results from the National Trauma Data Bank. J Pediatr Surg, 47: 1677, 2012 [DOI] [PubMed] [Google Scholar]
- 13.Kotkin L, Koch MO: Morbidity associated with nonoperative management of extraperitoneal bladder injuries. J Trauma, 38: 895, 1995 [DOI] [PubMed] [Google Scholar]
- 14.Yeung LL, McDonald AA, Como JJ et al. : Management of blunt force bladder injuries: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg, 86: 326, 2019 [DOI] [PubMed] [Google Scholar]
- 15.Myers JB, Taylor MB, Brant WO et al. : Process improvement in trauma: traumatic bladder injuries and compliance with recommended imaging evaluation. J Trauma Acute Care Surg, 74: 264, 2013 [DOI] [PubMed] [Google Scholar]
- 16.Morey AF, Zhao L: Bladder Injuries. In: Campbell-Walsh Urology Edited by Wein AJ: Elsevier Inc., vol. 11, pp. 2387–2388, 2016 [Google Scholar]
- 17.Agarwal A: Pelvic Ring Fractures. In: Rockwood and Green’s fractures in adults Edited by Court-Brown C, Heckman J, McQueen M et al. : Wolters Kluwer Health, vol. 8, pp. 1816–1817, 2015 [Google Scholar]
- 18.Figler BD, Hoffler CE, Reisman W et al. : Multi-disciplinary update on pelvic fracture associated bladder and urethral injuries. Injury, 43: 1242, 2012 [DOI] [PubMed] [Google Scholar]


