FIGURE 3.
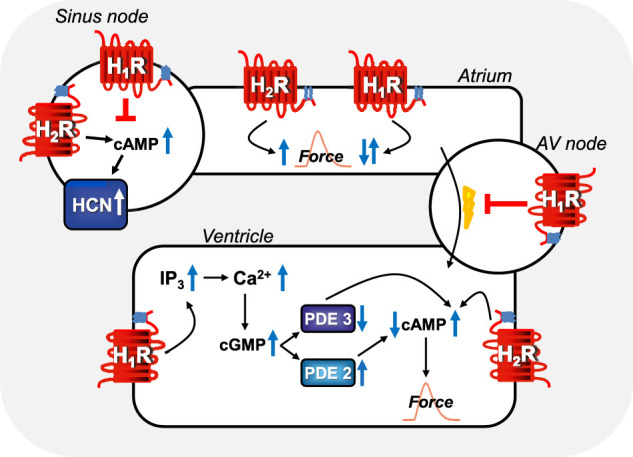
Comparison of regional H1-histamine receptor and H2-histamine receptor signaling in various regions of mammalian hearts. In sinus node cells, H2-histamine receptors can stimulate cAMP-production, this cAMP binds to HCN (=If-currents, hyperpolarization-activated ion channels) which thereafter open more often and tachycardia ensues (see Table 7 for details). Alternatively, H1-histamine receptors, in sinus node cells can reduce the beating rate via still unknown mechanisms (see Table 7 for details). In atrial muscle cells, H2-histamine receptors (via cAMP, see Figure 1A) and H1-histamine receptors (see Figure 1B via, for instance, activation of PLC and thereafter formation of IP3 and/or diacylglycerol and subsequent phosphorylation steps) can both increase atrial force of contraction in some species. In other species, H1-histamine receptors in atrial muscle cells decrease force of contraction by activation of phosphodiesterase, inhibition of protein kinases and/or activation of phosphatases. In the atrioventricular (AV) node, H1-histamine receptors in most species inhibit electrical conduction into the ventricle (see Table 7 for details). Likewise, in the ventricular muscle cells, H2-histamine receptors increase force of contraction by the mechanism depicted in Figure 1A. But also, in some species, ventricular muscle H1-histamine receptors can increase force of contraction (see Figure 1B), in other species, H1-histamine receptors lead to a reduction in force of contraction via the hypothetical mechanism depicted: a cGMP-mediated increase in phosphodiesterase II (PDE II) activity. Alternatively, in other species cGMP might inhibit PDE III and thereby increase cAMP and subsequently (See Figure 1B for details) force of contraction.
