Abstract
From January 1, 2018, through October 9, 2019, 82 HIV diagnoses occurred among people who inject drugs (PWID) in Cabell County, West Virginia. Increasing the use of HIV preexposure prophylaxis (PrEP) among PWID was one of the goals of a joint federal, state, and local response to this HIV outbreak. Through partnerships with the local health department, a federally qualified health center, and an academic medical system, we integrated PrEP into medication-assisted treatment, syringe services program, and primary health care settings. During the initial PrEP implementation period (April 18–May 17, 2019), 110 health care providers and administrators received PrEP training, the number of clinics offering PrEP increased from 2 to 15, and PrEP referrals were integrated with partner services, outreach, and testing activities. The number of people on PrEP increased from 15 in the 6 months before PrEP expansion to 127 in the 6 months after PrEP implementation. Lessons learned included the importance of implementing PrEP within existing health care services, integrating PrEP with other HIV prevention response activities, adapting training and material to fit the local context, and customizing care to meet the needs of PWID. The delivery of PrEP to PWID is challenging but complements other HIV prevention interventions. The expansion of PrEP in response to this HIV outbreak in Cabell County provides a framework for expanding PrEP in other outbreak and non-outbreak settings.
Keywords: people who inject drugs, HIV, preexposure prophylaxis, outbreak response, implementation
As a consequence of the opioid crisis and an increase in injection drug use (IDU), recent HIV outbreaks have occurred in the United States among people who inject drugs (PWID).1,2 Introducing HIV into IDU networks with high levels of needle and equipment sharing can result in rapid HIV transmission.3 -5 Rural or medium-sized counties with high rates of IDU may be especially vulnerable to HIV outbreaks, because they may lack the public health and health care infrastructure to quickly identify and intervene on a rapidly expanding HIV cluster.6,7
In January 2019, the West Virginia Bureau for Public Health detected an increase in the number of HIV diagnoses among PWID in Cabell County, a medium-sized metropolitan area on the western border of the state that includes the city of Huntington. In 2018, Cabell County had an adult population of 76 000 and an estimated 1857 PWID. 8 During 2013-2017, Cabell County averaged 8 cases of newly diagnosed HIV infection annually, of which an average of 2 cases per year were among PWID. From January 1, 2018, through October 9, 2019, Cabell County reported 82 new HIV diagnoses among PWID, their sex or IDU partners, and people linked to them by molecular sequencing. 9 Centers for Disease Control and Prevention (CDC) staff members supported the West Virginia Bureau for Public Health and the Cabell-Huntington Health Department (CHHD) in their response to this HIV outbreak by increasing HIV testing, expanding HIV prevention services, improving linkage to care for people with HIV, and providing surge staffing for partner services.
One key component of the response was increasing the use of HIV preexposure prophylaxis (PrEP) among PWID. PrEP use with daily tenofovir disoproxil fumarate/emtricitabine (TDF/FTC) is approved for the prevention of HIV among PWID and people at risk for sexual acquisition of HIV.5,10,11 A 2018 assessment of PWID in Cabell County and Kanawha County, West Virginia, found that knowledge of PrEP was low (30%) and that costs, potential medication nonadherence, unstable housing, and limited access to health care were perceived barriers to using PrEP; however, levels of willingness to take PrEP were high (65%). 12 Other qualitative assessments among PWID in in the United States indicated that the level of knowledge about PrEP was low.13 -17 This case study describes the implementation of PrEP in Cabell County as part of a response to an HIV outbreak among PWID.
Methods
Setting
In 2017, West Virginia ranked highest in the nation in drug overdose deaths, with an age-adjusted rate of 57.8 deaths per 100 000 population, as compared with the national rate of 21.7 deaths per 100 000 population. 18 In 2018, Cabell County recorded at least 149 overdose deaths, the highest of all counties in West Virgina. 19 In response to this challenge, CHHD and the medical community established a syringe services program (SSP) operated at CHHD, which served approximately 900 clients, increased the community distribution of naloxone, and expanded the availability of medication-assisted treatment (MAT) for people with opioid use disorder.
At the beginning of 2019, only 2 infectious disease clinics affiliated with teaching hospitals located in central Huntington offered PrEP. CHHD was working with Marshall University, an academic medical center located in Huntington, to start a PrEP clinic at the CHHD sexually transmitted infection clinic. Marshall University infectious disease faculty members had provided PrEP training to primary care providers, but broad PrEP implementation in primary care settings had not yet been achieved. Valley Health Systems was the largest network of federally qualified health centers in the area and provided primary health care and MAT. However, Valley Health providers had never received formal PrEP training.
Intervention
PrEP with daily TDF/FTC has been recommended by CDC since 2012 and for PWID since 2013. 10 However, Cabell County was estimated to have only 16 people using PrEP in 2017.20,21 West Virginia began enrolling patients in expanded Medicaid in January 2014. Medicaid covered TDF/FTC with no prior authorization requirement and minimal out-of-pocket costs. Uninsured patients could access TDF/FTC through a medication assistance program offered by the manufacturer. Both Valley Health and Marshall University were eligible to purchase TDF/FTC using the Medicaid 340B Drug Pricing Program, which allows safety-net health care systems to purchase drugs at a discounted rate, charge commercial insurance the regular price, and use the difference to provide care for their medically underserved population.
Implementation Strategy
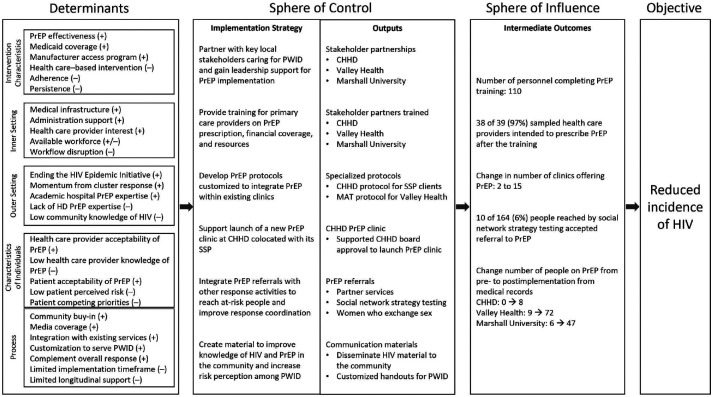
PrEP expansion activities occurred from April 18 through May 17, 2019 (Figure). CHHD introduced CDC PrEP subject matter experts to leadership team members from Valley Health and Marshall University who supported PrEP implementation. CHHD also requested CDC assistance in launching its previously planned PrEP clinic in the same location as its SSP. Valley Health requested assistance with integrating PrEP within its MAT clinic, the Provider Response Organization for Addiction Care and Treatment.
Figure.
Summary of implementation of PrEP expansion framework and outcomes, Cabell County, West Virginia, 2019. (+) indicates a favorable determinant, (–) indicates an unfavorable determinant, and (+/−) indicates a mixed determinant of PrEP expansion. The preimplementation period was November 1, 2018, through April 30, 2019. The postimplementation period was May 1 through October 31, 2019. Abbreviations: CHHD, Cabell-Huntington Health Department; HD, health department; MAT, medication-assisted treatment; PrEP, preexposure prophylaxis; PWID, people who inject drugs; SSP, syringe services program.
CDC PrEP subject matter experts conducted in-person PrEP trainings for health care providers and administrators using a module tailored for PWID in Cabell County. The training covered how to prescribe PrEP, obtain financial coverage, and locate online PrEP resources. Social services providers working at homeless shelters and drug rehabilitation programs received training on how to refer patients to PrEP clinics.
CDC PrEP subject matter experts assisted CHHD in obtaining board of health approval for starting a PrEP clinic and developing a protocol to provide PrEP for PWID enrolled in its SSP. CDC PrEP subject matters experts also assisted the Provider Response Organization for Addiction Care and Treatment with integrating PrEP in its MAT clinical workflow by shifting prerequisite PrEP laboratory testing to intake screening, offering PrEP at the first provider visit, and monitoring PrEP use at subsequent MAT visits. Throughout the implementation process, CDC worked alongside PrEP champions or clinical and local public health leaders with influence or decisional authority to integrate PrEP in their institutions.
PrEP materials specific to PWID had not been developed by CDC before this response, and CDC PrEP subject matter experts customized PrEP handouts for the affected PWID population (communication material available from the authors upon request). Public health staff members distributed these forms and informational materials to health care providers and PWID, people contacted during partner services, and sex workers during outreach events. CHHD engaged a local newspaper, a local TV station, and social media to share messages about the HIV outbreak with the public.
Finally, we integrated PrEP education and referrals with a social network testing strategy designed to recruit within IDU networks in Cabell County to reach PWID who would otherwise not be reached by conventional testing. From May 22 through August 30, 2019, staff members recruited PWID who presented for testing to engage people in their injection or sexual network for testing using a respondent-driven sampling method. Staff members offered food and toiletries, HIV and hepatitis testing, and referral to a PrEP clinic if they expressed interest in PrEP.
Outcome Measurements
All health care providers who completed PrEP training were given the opportunity to complete a posttraining questionnaire that assessed their training, whether they routinely cared for PWID, and their intention to prescribe PrEP. After training, the number of clinics in Cabell County and the surrounding region offering PrEP were counted, to compare the 6-month preimplementation (November 1, 2018, through April 30, 2019) and postimplementation (May 1 through October 31, 2019) periods. We also measured the number of people reached by social network strategy testing who were referred to PrEP during these efforts to assess willingness to initiate PrEP.
We estimated the number of people using PrEP for CHHD through a manual medical record review of patients enrolled in the CHHD SSP. Valley Health and Marshall University queried their electronic health records to identify prescriptions for TDF/FTC and then excluded PWH and those receiving postexposure prophylaxis to estimate PrEP use during the pre- and postimplementation periods. People using PrEP could be counted in one or both early (May 1 through July 31, 2019) or late (August 1 through October 31, 2019) postimplementation periods.
The National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention at CDC determined this work to be a disease control activity that did not require institutional review board review.
Outcomes
Health Care Provider Training
In total, 110 health care providers and administrators completed the PrEP training module, and 56 health care providers completed the PrEP posttraining questionnaire. Of the 56 health care providers who were trained, most were from Valley Health (n = 35, 63%) or Marshall University (n = 18, 32%) and were primary care providers (n = 48, 86%) specializing in family medicine, internal medicine, pediatrics, or obstetrics/gynecology. These health care providers reported routinely caring for PWID as a part of their practice (n = 43, 77%) and being aware of PrEP (n = 45, 80%). However, only 7 (13%) health care providers had ever prescribed PrEP and only to a total of 14 patients. Of these 14 patients, 11 received PrEP for sexual HIV risk reduction, 2 for both sexual and IDU risk, and 1 for IDU risk only. Of the 39 health care providers who completed a question on intention to prescribe PrEP after the training, 38 (97%) reported an intention to prescribe PrEP.
Clinics Offering PrEP
After implementation, health care providers at 13 additional clinics received PrEP training and accepted referrals for PrEP, including 9 primary care providers, 2 obstetricians/gynecologists, 1 MAT clinic, and 1 CHHD clinic. Several clinics also added features to improve their care of PWID, including walk-in visits, Medicaid enrollment, medication storage, and referral to other social services.
PrEP Referrals
From May 22 through August 30, 2019, 194 participants were reached by social network strategy testing and offered PrEP. Of the 171 (88%) participants with information on whether they accepted a referral to PrEP, 7 (4%) were already using PrEP and 10 (6%) who were not using PrEP accepted a PrEP referral.
People Using PrEP
In the 6 months before PrEP expansion, 9 people received PrEP through Valley Health and 6 people received PrEP through Marshall University. During the 6-month postimplementation period, only 8 of approximately 900 SSP clients started PrEP at CHHD (Table). At Valley Health, 72 patients received PrEP during the postimplementation period, including 52 patients in the early period and 40 patients in the late period. At Marshall University, 47 patients received PrEP during the postimplementation period, including 25 in the early period and 25 in the late period. Only 23 of 78 (29%) people who started PrEP in the early postimplementation period stayed on PrEP in the late postimplementation period.
Table.
Number of people prescribed PrEP after implementation of PrEP expansion, by clinical site, Cabell County, West Virginia, 2019 a
| Period | CHHD | Valley Health | Marshall University |
|---|---|---|---|
| 0-3 Months postimplementation, no. of people prescribed PrEP b | 1 | 52 | 25 |
| 3-6 Months postimplementation c | |||
| No. of people persisting on PrEP | 0 | 20 | 3 |
| No. of new PrEP starts | 7 | 20 | 22 |
| 0-6 Months postimplementation, overall no. of people prescribed PrEP d | 8 | 72 | 47 |
Abbreviations: CHHD, Cabell-Huntington Health Department; PrEP, preexposure prophylaxis.
All values are numbers.
May 1 through July 31, 2019.
August 1 through October 31, 2019.
May 1 through October 31, 2019.
Lessons Learned
PrEP expansion should be considered early in an HIV outbreak response for PWID and other populations at risk of HIV. Early PrEP expansion allows for the integration of PrEP with other response activities including HIV testing, partner services, health communication, and outreach to key populations at risk of HIV. It also engages health care providers in outbreak response and increases awareness about HIV transmission. The priority of expanding PrEP provision needs to be carefully considered for communities with limited health services. In such settings, expanding access to other interventions, such as SSP or MAT, may take precedence. Opportunities should be pursued to integrate PrEP into SSP and MAT services as they are developed.
Identifying Opportunities for PrEP Expansion
Launching a dedicated PrEP clinic de novo might not be feasible during an outbreak response. Identifying health care systems that serve the affected population and integrating PrEP within those services can facilitate timely delivery of PrEP. In the context of the HIV outbreak in Cabell County, offering PrEP at an SSP, MAT clinic, and primary care clinics with basic laboratory capacity for testing for HIV, hepatitis, and renal function brought PrEP to locations where PWID already sought care. PrEP expansion may have been more successful at primary care clinics than at the SSP because PrEP integrates easily with primary care and PWID had longitudinal relationships with health care providers.
Getting leadership buy-in was essential for identifying and engaging key health system leaders for PrEP integration and sustainability. It was also crucial to identify and partner with PrEP champions who could influence decision makers, identify ways to rapidly disseminate practice changes, and continue to support PrEP implementation after the initial response.
Adapting Material to the Local Context
Brief, in-person, and interactive trainings that fit with health care provider schedules that convey the basics of PrEP prescribing can be sufficient training for providers. PrEP training should be tailored to the local context and administered by an expert considered credible by the audience. Subsequent trainings adapted to the local context can be given by PrEP champions to continue the momentum for PrEP implementation.
Adapting communication material that is nonstigmatizing and appropriate for the group at risk of HIV is necessary for its acceptability. Local media attention on an HIV outbreak response can be used to increase HIV and PrEP knowledge among the general population and affected networks. Framing the HIV outbreak response as part of the larger Ending the HIV Epidemic initiative 22 may improve an understanding of how local activities relate to national goals and increase support for PrEP.
Understanding the Financial Landscape
The delivery of PrEP services may be financially advantageous for federally qualified health centers and other safety-net health care systems that care for medically underserved populations. Both Valley Health and Marshall University were eligible for Medicaid 340B drug pricing, whereas CHHD incurred a small cost for offering PrEP. This cost difference may contribute to the prioritization of PrEP expansion by Marshall University and Valley Health. In West Virginia, Medicaid expansion helped increase access to affordable PrEP and other health services for this PWID population. Finally, it is important to communicate that PrEP medication coverage is possible for virtually all PWID, either through commercial insurance, Medicaid, or a medication assistance program such as the federal Ready, Set, PrEP program 23 or the manufacturer medication assistance program. 24
Willingness Versus Persistence
Although some PWID in Cabell County perceived being at lower than actual risk for HIV or expressed apathy about the risk of HIV infection because it was not immediately fatal, many PWID expressed a high level of interest and willingness to use PrEP. 12 Despite this level of interest and willingness, few PWID accepted referrals, initiated PrEP, and persisted on PrEP. PWID had a disconnection between willingness and persistence, or the ability to overcome barriers that hinder a patient’s ability to continually take PrEP longitudinally. Removing the barriers of cost and health care access, facilitating colocation with existing services for PWID, and offering medication storage were insufficient in persuading many PWID to initiate PrEP. For people who started PrEP, staying on PrEP in the face of their daily challenges with homelessness, food insecurity, and violence was challenging. Further research is needed to identify which interventions increase PrEP uptake and persistence among PWID.
Longitudinal Engagement
PrEP expansion in Cabell County benefited from the initial momentum of the HIV outbreak response, resulting in a measurable increase in the number of people using PrEP. However, the time and resources available for outbreak response were limited, and follow-up of PrEP expansion after the initial field response was ad hoc. PrEP prescribing plateaued in the late postimplementation period. Offering additional health care provider training, coaching PrEP providers, refining clinical protocols, and engaging nonclinical community leaders may have increased PrEP uptake.
Conclusions
Rapidly responding to HIV clusters and outbreaks and enhancing prevention services, including the use of SSP and PrEP for people at risk for HIV, are 2 key pillars of the Ending the HIV Epidemic initiative. 22 The delivery of PrEP to PWID is challenging given the complex social determinants of health that may impair their awareness of, access to, and ability to take PrEP longitudinally to lower the risk of HIV. Nonetheless, PrEP can still play a role in interrupting HIV transmission in a PWID outbreak setting. The expansion of PrEP in response to an HIV outbreak in Cabell County demonstrates that rapid PrEP implementation can be integrated with an overall outbreak response and result in a modest increase in PrEP use. Future research is needed to describe the comparative effectiveness of PrEP in controlling HIV outbreaks to known interventions such as testing, treatment of people with HIV, and expanding SSPs.
Acknowledgments
The authors thank Elizabeth Adkins (CHHD), Kimberly Booth (Valley Health), Rachel Merino (Valley Health), Michelle Perdue (CHHD), Angie Wellman (Valley Health), and Heather Wood (CHHD) for their contributions to this work.
Footnotes
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC).
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by CDC.
ORCID iD: Nathan W. Furukawa, MD, MPH  https://orcid.org/0000-0002-4268-0556
https://orcid.org/0000-0002-4268-0556
References
- 1. Alpren C, Dawson EL, John B, et al. Opioid use fueling HIV transmission in an urban setting: an outbreak of HIV infection among people who inject drugs—Massachusetts, 2015-2018. Am J Public Health. 2020;110(1):37-44. doi: 10.2105/AJPH.2019.305366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Peters PJ, Pontones P, Hoover KW, et al. HIV infection linked to injection use of oxymorphone in Indiana, 2014-2015. N Engl J Med. 2016;375(3):229-239. doi: 10.1056/NEJMoa1515195 [DOI] [PubMed] [Google Scholar]
- 3. Conrad C, Bradley HM, Broz D, et al. Community outbreak of HIV infection linked to injection drug use of oxymorphone—Indiana, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(16):443-444. [PMC free article] [PubMed] [Google Scholar]
- 4. Cranston K, Alpren C, John B, et al. Notes from the field: HIV diagnoses among persons who inject drugs—northeastern Massachusetts, 2015-2018. MMWR Morb Mortal Wkly Rep. 2019;68(10):253-254. doi: 10.15585/mmwr.mm6810a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bradley H, Hogan V, Agnew-Brune C, et al. Increased HIV diagnoses in West Virginia counties highly vulnerable to rapid HIV dissemination through injection drug use: a cautionary tale. Ann Epidemiol. 2019;34:12-17. doi: 10.1016/j.annepidem.2019.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Van Handel MM, Rose CE, Hallisey EJ, et al. County-level vulnerability assessment for rapid dissemination of HIV or HCV infections among persons who inject drugs, United States. J Acquir Immune Defic Syndr. 2016;73(3):323-331. doi: 10.1097/QAI.0000000000001098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lerner AM, Fauci AS. Opioid injection in rural areas of the United States: a potential obstacle to ending the HIV epidemic. JAMA. 2019;322(11):1041-1042. doi: 10.1001/jama.2019.10657 [DOI] [PubMed] [Google Scholar]
- 8. Allen ST, O’Rourke A, White RH, Schneider KE, Kilkenny M, Sherman SG. Estimating the number of people who inject drugs in a rural county in Appalachia. Am J Public Health. 2019;109(3):445-450. doi: 10.2105/AJPH.2018.304873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Atkins A, McClung RP, Kilkenny M, et al. Notes from the field: outbreak of human immunodeficiency virus infection among persons who inject drugs—Cabell County, West Virginia, 2018-2019. MMWR Morb Mortal Wkly Rep. 2020;69(16):499-500. doi: 10.15585/mmwr.mm6916a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention. US Public Health Service: preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. Published March 2018. Accessed April 10, 2019. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf
- 11. Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083-2090. doi: 10.1016/S0140-6736(13)61127-7 [DOI] [PubMed] [Google Scholar]
- 12. Allen ST, O’Rourke A, White RH, et al. Barriers and facilitators to PrEP use among people who inject drugs in rural Appalachia: a qualitative study. AIDS Behav. 2020;24(6):1942-1950. doi: 10.1007/s10461-019-02767-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bazzi AR, Biancarelli DL, Childs E, et al. Limited knowledge and mixed interest in pre-exposure prophylaxis for HIV prevention among people who inject drugs. AIDS Patient Care STDS. 2018;32(12):529-537. doi: 10.1089/apc.2018.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Biello KB, Bazzi AR, Mimiaga MJ, et al. Perspectives on HIV pre-exposure prophylaxis (PrEP) utilization and related intervention needs among people who inject drugs. Harm Reduct J. 2018;15(1):55. doi: 10.1186/s12954-018-0263-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Guise A, Albers ER, Strathdee SA. “PrEP is not ready for our community, and our community is not ready for PrEP”: pre-exposure prophylaxis for HIV for people who inject drugs and limits to the HIV prevention response. Addiction. 2017;112(4):572-578. doi: 10.1111/add.13437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Peterson M, Macmadu A, Truong AQ, et al. Pre-exposure prophylaxis awareness and interest among participants in a medications for addiction treatment program in a unified jail and prison setting in Rhode Island. J Subst Abuse Treat. 2019;106:73-78. doi: 10.1016/j.jsat.2019.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Walters SM, Reilly KH, Neaigus A, Braunstein S. Awareness of pre-exposure prophylaxis (PrEP) among women who inject drugs in NYC: the importance of networks and syringe exchange programs for HIV prevention. Harm Reduct J. 2017;14(1):40. doi: 10.1186/s12954-017-0166-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hoots BE, Xu L, Kariisa M. 2018 Annual Surveillance Report of Drug-Related Risks and Outcomes—United States. Surveillance Special Report. Centers for Disease Control and Prevention; 2018. Accessed March 11, 2019. https://www.cdc.gov/drugoverdose/pdf/pubs/2018-cdc-drug-surveillance-report.pdf [Google Scholar]
- 19. West Virginia Department of Health and Human Resources. Gov. Justice—DHHR data suggests West Virginia overdose deaths appear to be declining, 2018. Accessed February 25, 2020. https://dhhr.wv.gov/News/Pages/Gov.-Justice-DHHR-Data-Suggests-West-Virginia-Overdose-Deaths-Appear-to-be-Declining.aspx
- 20. Harris NS, Johnson AS, Huang YLA, et al. Vital signs: status of human immunodeficiency virus testing, viral suppression, and HIV preexposure prophylaxis—United States, 2013-2018. MMWR Morb Mortal Wkly Rep. 2019;68(48):1117-1123. doi: 10.15585/mmwr.mm6848e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Huang YLA, Zhu W, Smith DK, Harris N, Hoover KW. HIV preexposure prophylaxis, by race and ethnicity—United States, 2014-2016. MMWR Morb Mortal Wkly Rep. 2018;67(41):1147-1150. doi: 10.15585/mmwr.mm6741a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844-845. doi: 10.1001/jama.2019.1343 [DOI] [PubMed] [Google Scholar]
- 23. US Department of Health and Human Services. Ending the HIV epidemic: ready, set, PrEP. Accessed February 25, 2020. https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/prep-program
- 24. Gilead Sciences Inc. Advancing Access Patient Assistance Program. Accessed February 25, 2020. https://www.gileadadvancingaccess.com/financial-support/uninsured