ABSTRACT
Objective:
To evaluate the coating thickness of four brands of as-received esthetic coated rectangular archwires and their surface characteristics and coating stability after 21 days of oral exposure compared to those of conventional stainless steel (SS) and nickel titanium (NiTi) ones.
Materials and Methods:
The labial surface of the selected archwires was observed with a stereoscope and in a scanning electron microscope, and surface roughness was assessed with an atomic force microscope. The coating thickness of as-received wires and the percentage of coating lost on the labial surface of retrieved wires were measured using Image Pro Plus 4.5 software.
Results:
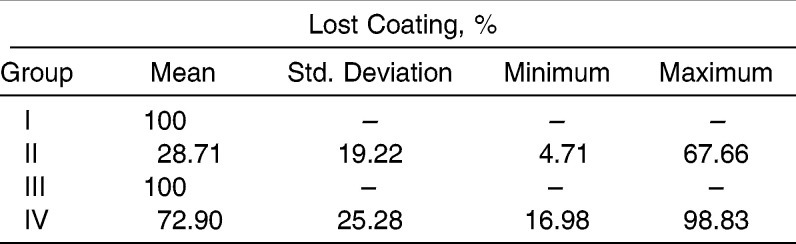
All groups showed an average coating thickness of less than 0.002 inches. After oral exposure, archwires from two groups lost all coating on the labial surface. On average, 28.71% and 72.90% of the coating was lost in each of the other two groups, and the surface roughness of the remaining coating was higher than postclinical control wires.
Conclusion:
Coated archwires had a low esthetic value as they presented a nondurable coating. The remaining coating showed a severe deterioration and a greater surface roughness than postclinical control counterparts (conventional SS and NiTi wires).
Keywords: Coating stability, Surface characteristic, Esthetic archwires
INTRODUCTION
The demand for esthetic orthodontic appliances is increasing, and the development of materials that present acceptable esthetics for the patients and an adequate clinical performance for clinicians is needed.1 This problem was partially solved by the introduction of esthetic brackets made of ceramic or composite.2 However, most archwires are still made of metals such as stainless steel (SS) and nickel titanium (NiTi), and an esthetic archwire is highly desirable to complement esthetic brackets in clinical orthodontics.
Metallic archwires coated with tooth-colored resin materials, such as synthetic fluorine-containing resin or epoxy resin composed mainly of polytetrafluoroethylyene, are currently the existing solution to this esthetic problem.3 The coating is applied in a depository process that plates the base wire, and its thickness is approximately 0.002 inches, as reported by manufacturers. Thus, a strong adhesion is achieved between the coating and the wire.4
There are different opinions in the literature concerning esthetic coated archwires. An evaluation of sliding properties and adherence of the coating to the archwires revealed that the plastic coating decreased friction between archwires and brackets.5 Some authors have experienced difficulties with these coated archwires, claiming that the color tends to change with time6 and that the coating splits during use in the mouth, exposing the underlying metal.7–9 However, despite these problems, these wires continue to be marketed and used in clinical practice, mainly when an esthetic alternative for a rectangular cross-sectional archwire is necessary.
The surface quality of archwires affects the area of surface contact and influences the esthetic result, the corrosion behavior, the plaque accumulation, and the biocompatibility.7 Among the properties in the search for the ideal archwire, the surface topography plays an important role and can critically modify the efficiency of orthodontic components.10,11 Further, increased surface roughness can increase the friction coefficient12 and is an essential factor in determining the effectiveness of archwire-guided tooth movement.11
Thus, besides coating stability, it is necessary that a coated archwire present characteristics at least comparable to the conventional, most-used archwires, like SS and NiTi alloys, when exposed to an oral environment. However, little information is available in the orthodontic literature comparing the surface changes of these archwires after oral exposure.
The purpose of this study was to evaluate the coating thickness of as-received esthetic coated rectangular archwires and their surface characteristics and coating stability after 21 days of oral exposure compared to those of conventional SS and NiTi ones.
MATERIALS AND METHODS
Four brands of coated archwire and their respective control counterparts were evaluated (Table 1). As the methods used for this study are inappropriate tools for the analysis of rounded surfaces, wires with a rectangular cross section were investigated.
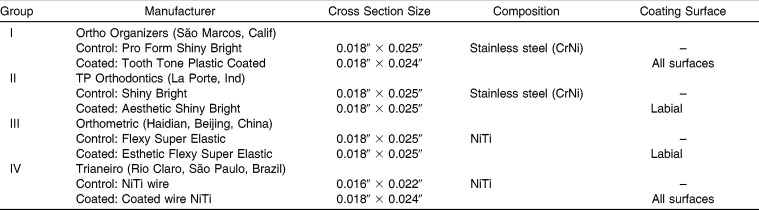
Table 1.
Characteristics of Archwires Used in the Study
A sample size calculation based on a pilot study showed that at least three as-received and six postclinical specimens per group would be necessary to detect a difference of 0.02 µm (α = 0.05, β = 0.10) in the surface roughness. The sample was composed of 164 wire segments 20 mm long. Sixty-eight wires were from as-received archwires, and 96 segments (12 specimens of each kind of wire) were retrieved after 21 days in the oral cavity.
Retrieved wires were obtained from 12 subjects. Ethical approval for this research was obtained from the Ethics in Research Committee of the Institute of Public Health Studies from the Federal University of Rio de Janeiro (process 0034.0.239.000-11). Every patient signed an informed consent form. The inclusion criteria included: good oral hygiene, no caries, and no systemic changes.
Each hemiarch of the included subjects received two metal, edgewise, standard brackets (Morelli, Sorocaba, São Paulo, Brazil), which were bonded to two posterior teeth in a way that an archwire of at least 20 mm in length could be inserted in the slot passively. The groups were allocated randomly to each hemiarch according to a split-mouth design using random number tables. Different individuals were responsible for the generation and execution of the randomization. The control wire was tied juxtaposed to the upper base of the brackets' wings, and the coated wire was tied into the slot with stainless steel 0.010-inch ligatures (Morelli). Oral hygiene products (toothbrush, toothpaste, and dental floss) and instructions were given to all patients, and they were informed not to use any other oral agents, such as mouthwashes.
All specimens were placed and removed by the same operator. The subjects were blinded as to the disposition of wires in the mouth. However, it was not possible to blind the operator to the type of coated wire used on each quadrant in the mouth because of the characteristic color of each coated wire.
Retrieved wires were collected after 21 days of oral exposure and individually immersed in detergent (Amway, Ada, Mich) in an ultrasound cleaner (Cristófoli LTDA, Campo Mourão, Paraná, Brazil) for a 20-minute cycle and afterwards in distilled water for an additional 10 minutes. As-received specimens were submitted to this same protocol.
Coating Thickness
Five as-received coated wires of each group were included, with their transverse section facing up, in 10-mm-high and 5-mm-diameter plastic tubes filled with light-curing composite resin (Monolok2; Rocky Mountain Orthodontics, Denver, Colo). Then the samples were ground in a water-cooled polishing machine (Politriz DP-9U2; Struers A/S, Copenhagen, Denmark) with 360-, 400-, 600-, and 1200-grit abrasive papers under refrigeration.
Images of transverse sections from the specimens were made with a stereoscope at 45× magnification (Olympus SZ61; Olympus, Tokyo, Japan). The coating thickness of all coated surfaces of each wire was measured using Image Pro Plus 4.5 software (Media Cybernetics, Silver Spring, Md). For each coated surface, three coating thickness readings were measured randomly (Figure 1). The operator was previously calibrated (intraclass correlation coefficient = .99) by measuring 10 samples twice.
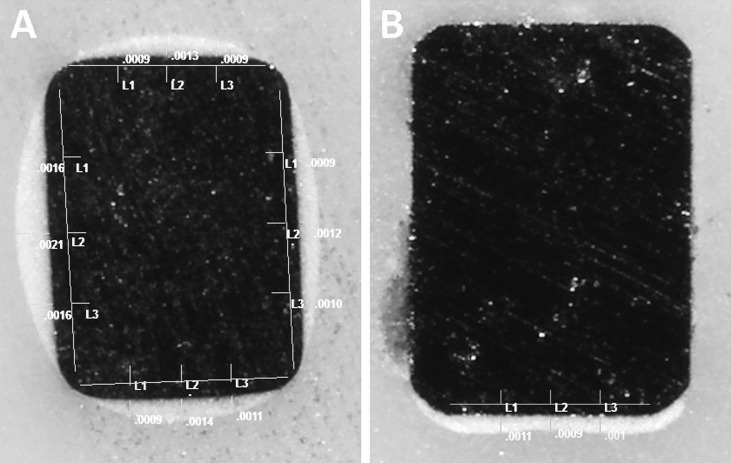
Figure 1.
Stereoscope images of coating thickness measurement method: (A) group IV with all surfaces coated and (B) group II with coating only on the labial surface. Original magnification 45×.
Lost Coating Measurement
An Olympus SZ61 stereoscope was used to study the labial surface topography of the wires at 35× magnification, and digital images were recorded. The lost coating on the labial surface of all retrieved coated wires was measured using Image Pro Plus 4.5 software. Graph paper with a width of 10 mm was fixed on a glass slide and served as a template. Each wire was positioned with the midpoint on the center of the graph paper, and the ends were fixed with wax. Two 5-mm-long images were obtained of the same sample, one on its right side and one on its left side. Thus, the 10-mm segment of each coated wire located in the interbracket space was fully evaluated (Figure 2).
Figure 2.
Representative stereoscope images of labial surfaces of postclinical coated wires, where lost coating was measured using Image Pro Plus 4.5 software: (A) group II and (B) group IV. Original magnification 35×.
The overall area of the wire and the area of the lost coating on the labial surface were calculated, and the percentage of the lost coating was obtained.
Surface Characterization
A scanning electron microscope (SEM; JEOL JSM 6460 LV; JEOL Ltd, Tokyo, Japan) was used to assess the micromorphological characteristics of the labial surfaces of three as-received and six postclinical samples from each kind of wire. The images were recorded at 90×, 200×, and 500× magnification.
Surface Roughness
Three as-received and six retrieved samples from each kind of wire—coated and control—were analyzed. Each wire segment was fixed on a glass slide with its labial surface facing up. Surface roughness measurements were made with an atomic force microscope (AFM; JPK Nanowizard, Nr: H-01-0086, and JPK Image Processing software, version 3.0; JPK Instruments AG, Berlin, Germany) with a noncontact tip coated with silicon (NCLR-20; NanoWorld, Neuchâtel, Switzerland), with a constant force of 48 N/mm and resonance frequency of 190 kHz. For each specimen, three surface scans were taken with a scanning area of 20 µm × 20 µm, one in the center of the wire, one 2 mm left, and one 2 mm right. Proprietary software was used to calculate the arithmetic average roughness, Ra (the arithmetic mean of the absolute departures of the roughness profile from the mean line).
Statistical Analyses
A standard statistical software package (SPSS version 16.0; SPSS Inc, Chicago, Ill) was used for data analysis. The Kolmogorov-Smirnov test was applied to verify the normality in the results, and descriptive data were calculated for coating thickness, lost coating percentage, and surface roughness. The surface roughness results of each group were submitted to a two-way analysis of variance test to verify the influence of coating and of clinical exposure and the interaction of both factors on the results. A one-way analysis of variance with a Tukey post-hoc test was used afterwards to identify intragroup differences in surface roughness.
RESULTS
Coating thickness for as-received wires is shown in Table 2. All groups showed an average coating thickness of less than 0.002 inches, which is the thickness informed by the manufacturers. Group IV had the highest average coating thickness, but it was the most irregular one, assuming a round cross-sectional aspect (Table 2 and Figure 1A). The most uniform coating was present in group II (Figure 1B). A lower coating thickness was observed on the corners in all groups.
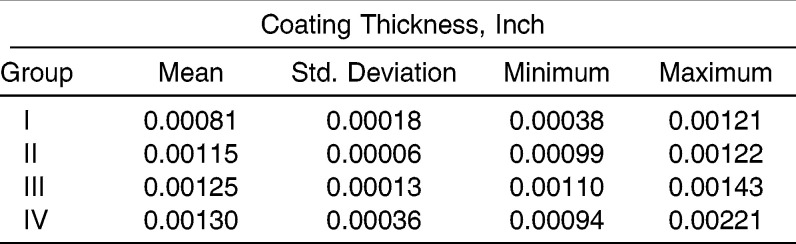
Table 2.
Coating Thickness (Inch) Mean, Standard deviation, and Minimum and Maximum Values of As-Received Coated Wires in Each Group
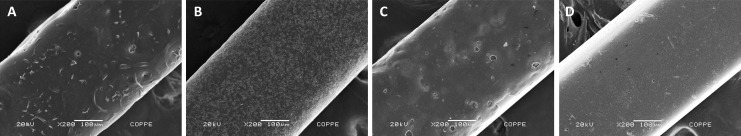
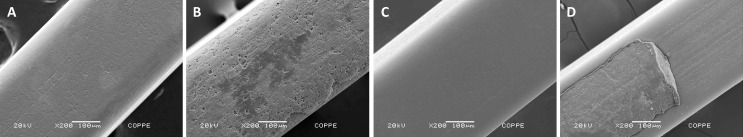
Figure 3 shows the evaluation of the labial surface topography of the as-received coated wires with SEM photomicrographs. Many of the specimens were characterized by small delamination and irregularities of the coating over some points. Group IV presented the smoothest surface aspect and group II the roughest.
Figure 3.
Photomicrographs of as-received coated wires: (A) group I, (B) group II, (C) group III, and (D) group IV. Original magnification 200×.
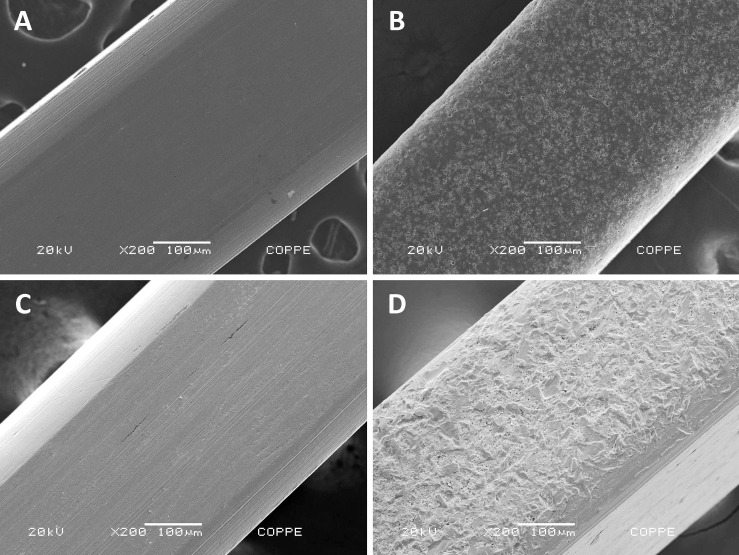
Illustrative SEM photomicrographs of retrieved coated wires are shown in Figure 4. The entire coating layer on the labial surface was lost in groups I and III, exposing the metallic surface underneath. Group IV showed some areas of coating delamination, but the metallic surface underneath presented an appearance similar to the retrieved control wires, as in groups I and III. Coating delamination areas on retrieved wires of group II showed a rougher metallic surface aspect than retrieved control wires (Figure 5).
Figure 4.
Photomicrographs of postclinical coated wires: (A) group I with the entire coating layer lost, (B) group II with remaining coating, (C) group III with the entire coating layer lost, and (D) group IV with remaining coating. Original magnification 200×.
Figure 5.
Photomicrographs of group II wires: (A) as-received control wire, (B) as-received coated wire, (C) postclinical control wire, and (D) rough surface of postclinical coated wire that lost the coating layer. Original magnification 200×.
Percentages of lost coating on the labial surface after oral exposure are shown in Table 3. In groups I and III, all coating was lost after oral exposure, exposing the metallic surface below completely. On average, 28.71% and 72.90% of coating was lost in groups II and IV, respectively (Figure 2).
Table 3.
Lost Coating Percentage Mean, Standard Deviation, and Minimum and Maximum Values (Labial Surface of Postclinical Coated Wires)
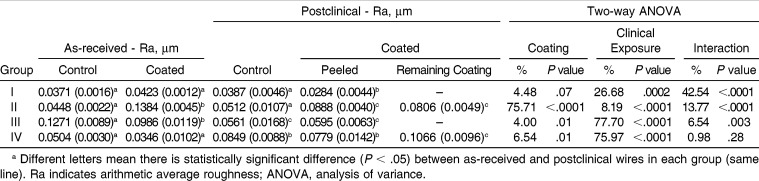
The comparison of surface roughness between as-received control and coated wires in each group is shown in Table 4. No statistically significant difference was seen in the surface roughness of as-received control and coated wires in groups I and IV. In group II, the surface roughness of as-received coated wires was approximately three times higher than that of SS control wires. Nevertheless, in group III, the surface roughness of as-received coated wires was lower than that of NiTi control wires. The roughest coating was found in group II, and the smoothest coating was in group IV.
Table 4.
Surface Roughness (Ra, µm) Mean and Standard Deviation, Two-Way Analysis of Variance Results, and Tukey Post Hoc Comparison Between As-Received and Postclinical Control and Coated Wires in Each Groupa
The comparison of surface roughness between as-received and postclinical wires in each group is shown in Table 4. The two-way analysis of variance test results showed that the coating factor was the one most responsible (75.71%) for the variation in the surface roughness in group II. In groups III and IV, the factor most responsible was the clinical exposure (77.70% and 75.97%, respectively). And in group I, the interaction of both factors was the greatest factor responsible (42.54%) for the variation. In group IV, the roughness of the remaining coating of the postclinical coated wires was higher than that of as-received coated wires, but in group II it was lower. The roughness of peeled areas of postclinical coated wires was lower or similar to that of postclinical control wires in groups I, III, and IV, and rougher than control wires' surface in group II. For groups I and II with SS control wires, no statistical difference was observed in surface roughness of as-received and postclinical samples. For NiTi control wires, the roughness surface decreased after oral exposure in group III and increased in group IV. Surface roughness of the remaining coating in groups II and IV, which maintained the coating partially, was higher than postclinical control wires' surface.
DISCUSSION
Retrieval analyses conducted on dental materials have recently received increasing interest because of the critical information derived from investigating the performance of the material in the environment in which it was intended to function.13 The evidence available implies that the mechanism of surface modification is not completely elucidated.14
The surface topography of an orthodontic wire is an essential property known to influence its mechanical characteristics, esthetic appearance, corrosion behavior, and/or its biocompatibility.15 Clinically, a rough surface encourages greater plaque accumulation, influences its friction properties, and increases corrosion and color instability.11,12,16,17
Among the available techniques for determining surface roughness, AFM seems to be the most suitable for the investigation of surface topography. This noninvasive technique produces a more detailed surface profile delivering a three-dimensional, realistic impression and giving quantitative and qualitative height measurements.11
The labial surface topography of as-received coated wires with SEM showed coating delamination and irregularities (Figure 3). A great variation in the type and number of surface defects on the labial side of each sample, and also between different samples of as-received wires, could be noted. This variation probably depends on different factors during the manufacturing process. Specific information about the processing of the wires is a property of each manufacturer and is not available. Nevertheless, this investigation revealed a large number of irregularities present on as-received archwires.
Additionally, as-received coated wires did not show a uniform coating-thickness pattern (Table 2). The coating layer clearly tended to be thicker in the center and thinner on the edges of labial surface (or all surfaces; Figure 1). This characteristic could make the coating layer more susceptible to damage. Besides, this irregularity in coating thickness might impair the wire-bracket slot engagement, influencing tooth movement.
The coating layer peeled off in many areas during oral exposure, leaving surface defects. This peeling characteristically started by the upper and lower labial edges—because these are tensile accumulation zones with lower coating thickness—and toward the center of the surface (Figure 2). This clearly affects the esthetic value of these coated wires. These results agree with a study by Elayyan et al.7 in which the coating was partially lost, with increased roughness after clinical use. However, this study just evaluated one type of esthetic archwire and did not compare its surface characteristics with those of postclinical SS and NiTi archwires.
The smaller loss of the coating layer in group II may be due to a surface treatment on stainless steel, which makes the labial surface where the coating is applied rougher, improving the mechanical adhesion between the coating and substrate (Figure 5). Peeled areas on these wires that exposed the metallic surface underneath presented a higher surface roughness than that of postclinical control wires (Table 4). Moreover, the surface roughness of the remaining coating was also higher than that of postclinical control wires. The irregular surfaces observed microscopically, some areas of the remaining coating layer and some areas of metallic exposure, may lead to plaque accumulation in surface defects, and tooth movement may be affected due to entrapment of bracket edges inside these defects, according to some authors.8,9,18
The surface quality of the products investigated differs significantly. A dominant factor in the determination of the surface structure of an orthodontic archwire is the production technique. As the production techniques are generally similar for all types of wires from one manufacturer, the differences in the surface roughness of peeled areas of coated wires is probably due to the method of applying the coating, which could require some surface treatment and/or heat treatment, or due to the properties and composition of the coating material. No group had its entire coating layer maintained and at the same time presented a surface roughness similar to the ones from the control wires after oral exposure. The surface roughness of the remaining coating in groups II and IV, which maintained the coating layer partially, was higher than postclinical control wires and showed a highly deteriorated surface (Table 4 and Figure 4).
The oral exposure of 21 days had an important role in the coating loss and in the surface quality of coated wires. Considering the orthodontic treatment duration, none of the esthetic archwires studied presented ideal characteristics for clinical use. Limitations of this paper include a short duration of oral exposure and few studies in the literature to compare our results with, making our conclusions based mainly on our findings. Therefore, the necessity of knowledge of the surface characteristics of the commercially available and currently used coated archwires is evident. The permanent development of these materials is urgent, and ideal esthetic archwires should have great esthetic aspects, with surface characteristics at least similar to those of conventional SS and NiTi archwires, and the ability to maintain integrity in the oral environment.
CONCLUSIONS
The esthetic coated archwires did not show a uniform coating-thickness pattern.
These wires had low esthetic value as they presented a nondurable coating after oral exposure.
The remaining coating showed a severe deterioration and a greater surface roughness compared to postclinical control counterparts (conventional SS and NiTi wires).
REFERENCES
- 1.Elayyan F, Silikas N, Bearn D. Mechanical properties of coated superelastic archwires in conventional and self-ligating orthodontic brackets. Am J Orthod Dentofacial Orthop. 2010;137:213–217. doi: 10.1016/j.ajodo.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 2.Russell JS. Aesthetic orthodontic brackets. J Orthod. 2005;32:146–163. doi: 10.1179/146531205225021024. [DOI] [PubMed] [Google Scholar]
- 3.Ramadan AA. Removing hepatitis C virus from polytetrafluoroethylene-coated orthodontic archwires and other dental instruments. East Mediterr Health J. 2003;9:274–278. [PubMed] [Google Scholar]
- 4.Clocheret K, Willems G, Carels C, Celis JP. Dynamic frictional behaviour of orthodontic archwires and brackets. Eur J Orthod. 2004;26:163–170. doi: 10.1093/ejo/26.2.163. [DOI] [PubMed] [Google Scholar]
- 5.Husmann P, Bourauel C, Wessinger M, Jager A. The frictional behavior of coated guiding archwires. J Orofac Orthop. 2002;63:199–211. doi: 10.1007/s00056-002-0009-5. [DOI] [PubMed] [Google Scholar]
- 6.Silva DL, Mattos CT, Araújo MV, Ruellas ACO. Color stability and fluorescence of different orthodontic esthetic archwires. Angle Orthod. 2013;83:127–132. doi: 10.2319/121311-764.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elayyan F, Silikas N, Bearn D. Ex vivo surface and mechanical properties of coated orthodontic archwires. Eur J Orthod. 2008;30:661–667. doi: 10.1093/ejo/cjn057. [DOI] [PubMed] [Google Scholar]
- 8.Postlethwaite KM. Advances in fixed appliance design and use: 1. Brackets and archwires. Dent Update. 1992;19:276–278, 280. [PubMed] [Google Scholar]
- 9.Kusy RP. A review of contemporary archwires: their properties and characteristics. Angle Orthod. 1997;67:197–207. doi: 10.1043/0003-3219(1997)067<0197:AROCAT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.D'Anto V, Rongo R, Ametrano G, et al. Evaluation of surface roughness of orthodontic wires by means of atomic force microscopy. Angle Orthod. 2012;82:922–928. doi: 10.2319/100211-620.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bourauel C, Fries T, Drescher D, Plietsch R. Surface roughness of orthodontic wires via atomic force microscopy, laser specular reflectance, and profilometry. Eur J Orthod. 1998;20:79–92. doi: 10.1093/ejo/20.1.79. [DOI] [PubMed] [Google Scholar]
- 12.Doshi UH, Bhad-Patil WA. Static frictional force and surface roughness of various bracket and wire combinations. Am J Orthod Dentofacial Orthop. 2011;139:74–79. doi: 10.1016/j.ajodo.2009.02.031. [DOI] [PubMed] [Google Scholar]
- 13.Eliades T, Eliades G, Athanasiou AE, Bradley TG. Surface characterization of retrieved NiTi orthodontic archwires. Eur J Orthod. 2000;22:317–326. doi: 10.1093/ejo/22.3.317. [DOI] [PubMed] [Google Scholar]
- 14.Eliades T, Bourauel C. Intraoral aging of orthodontic materials: the picture we miss and its clinical relevance. Am J Orthod Dentofacial Orthop. 2005;127:403–412. doi: 10.1016/j.ajodo.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 15.Daems J, Celis JP, Willems G. Morphological characterization of as-received and in vivo orthodontic stainless steel archwires. Eur J Orthod. 2009;31:260–265. doi: 10.1093/ejo/cjn104. [DOI] [PubMed] [Google Scholar]
- 16.Saunders CR, Kusy RP. Surface topography and frictional characteristics of ceramic brackets. Am J Orthod Dentofacial Orthop. 1994;106:76–87. doi: 10.1016/S0889-5406(94)70024-9. [DOI] [PubMed] [Google Scholar]
- 17.Eliades T, Athanasiou AE. In vivo aging of orthodontic alloys: implications for corrosion potential, nickel release, and biocompatibility. Angle Orthod. 2002;72:222–237. doi: 10.1043/0003-3219(2002)072<0222:IVAOOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Proffit WR. Contemporary Orthodontics. St Louis, Mo: Mosby; 2000. [Google Scholar]