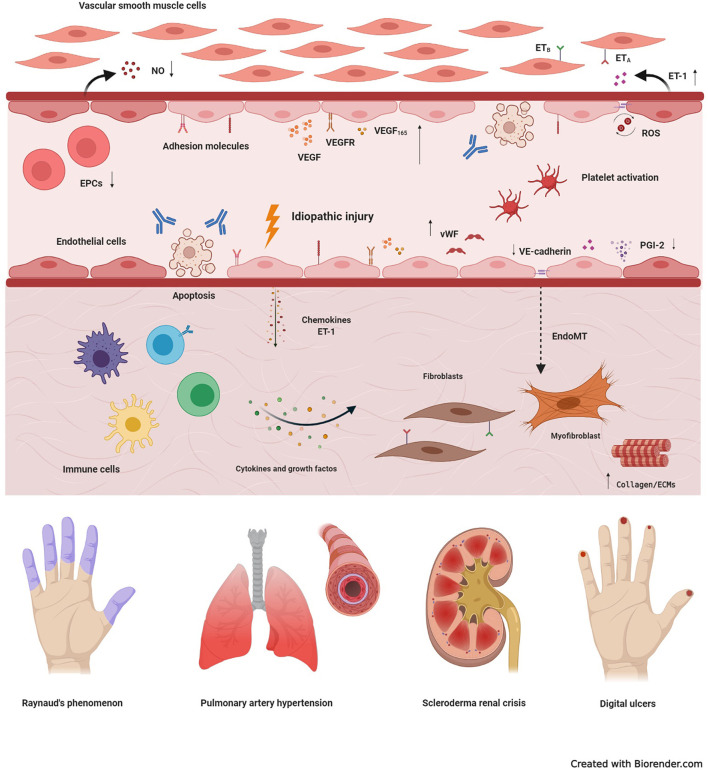
Figure 1.
Basic mechanisms of systemic sclerosis-related vasculopathy. Vascular injury is considered an initial event in the development of systemic sclerosis (SSc), and may be triggered by multiple factors, including autoantibodies, infectious agents, reactive oxygen species (ROS), or idiopathic stimuli. In the early stages of disease, vascular damage leads to activation of endothelial cells (ECs), with expression of adhesion molecules, production of chemokines, von Willebrand factor (vWF) and vasoconstrictor agents, such as endothelin-1 (ET-1). Molecules produced by the injured endothelium recruit immune cells, that generate a perivascular infiltrate. Prolonged inflammation leads to tissue fibrosis, with excessive activation of resident fibroblasts that transdifferentiate into myofibroblasts, the main cell type involved in excessive collagen production and other extracellular matrix components (ECMs). Myofibroblasts are also originated through the endothelial-to-mesenchymal transition (EndoMT). Dysfunction of endothelial progenitor cells (EPCs), antibody-induced ECs apoptosis, persistent platelet activation, decreased production of vasodilatory nitric oxide (NO) and prostaglandin I-2 (PGI-2), synthetized by ECs, also participate in the pathogenesis of SSc-vasculopathy. In addition, compensatory mechanisms of vasculogenesis and angiogenesis, including vascular endothelial growth factor (VEGF) and its receptor (VEGFR), are dysregulated and ineffective. High expression of VEGF165, an anti-angiogenic isoform, contributes to this scenario. Reactive oxygen species, further contribute to intensify damage and activation of the endothelium and, thus, increase tissue injury. Clinical manifestations of SSc-related vasculopathy include Raynaud's phenomenon, pulmonary arterial hypertension, scleroderma renal crisis, telangiectasias, digital ulcers and digital pitting scars, which severely affect quality of life and may compromise survival. ETA, type A endothelin receptor; ETB, type B endothelin receptor.