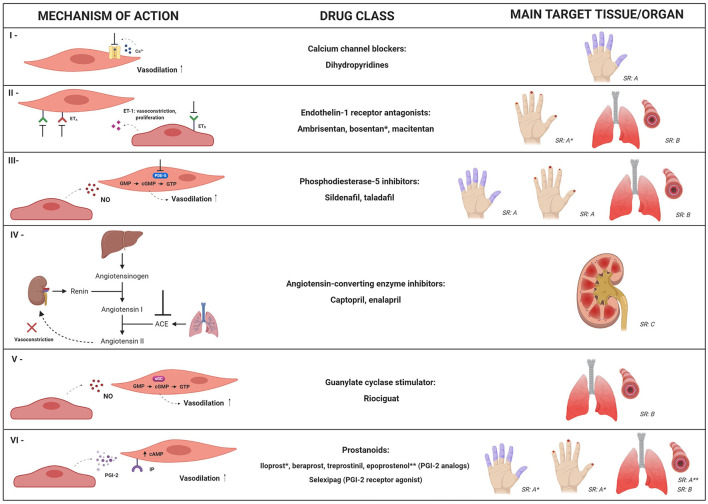
Figure 2.
Mechanistic targets of the main pharmacological approaches for systemic sclerosis-related vasculopathy. Multiple drug options, with different mechanistic approaches, can be used for management of vascular manifestations in SSc patients. This figure summarizes mechanisms and clinical indications for: calcium channel blockers (I); endothelin-1 receptor antagonists (II); phosphodiesterase-5 (PDE-5) inhibitors (III); angiotensin-converting enzyme (ACE) inhibitors (IV); guanylate cyclase stimulator – riociguat (V) and prostanoids (VI). SR: strength of recommendation; SR: A, SR: B or SR: C according to the European League against Rheumatism, in 2017 (87). Dihydropyridines, PDE-5 inhibitors and iloprost are recommended for SSc-associated Raynaud's phenomenon (SR: A); bosentan is recommended to reduce the number of new digital ulcers (SR: A); PDE-5 inhibitors and iloprost are recommended for active digital ulcers (SR: A); PDE-5 inhibitors, endothelin-1 receptor antagonists (bosentan, ambrisentan, and macitentan) and riociguat are recommended for treatment of SSc-related pulmonary artery hypertension (SR: B); epoprostenol (SR: A) and other prostacyclin analogs (SR: B) are recommended for severe SSc-related pulmonary artery hypertension; ACE inhibitors are recommended as treatment for scleroderma renal crisis (SR: C). * and ** indicate clinical conditions in which specific drugs from the class are recommended. NO, nitric oxide; ET-1, endothelin-1; ETA, type A endothelin receptor; ETB, type B endothelin receptor; cGMP, cyclic guanosine-5-monophosphate; sGC, soluble guanylate cyclase; cAMP, cyclic adenosine monophosphate; GTP, guanosine-5′-triphosphate; IP, prostacyclin receptor; PGI-2, prostaglandin I-2.