Abstract
Aim:
Present systematic review and meta-analysis examined the burden of psychological reactions predominantly anxiety, depression, stress, and insomnia during the novel COVID-19 pandemic phase among the frontline healthcare, nonfrontline healthcare, and general population.
Material and Methods:
PubMed, EMBASE, and SCOPUS were searched for studies between January 1, 2020, and May 25, 2020. Brief protocol of the systematic review was registered with the PROSPERO database, (CRD42020186229). Any study that reported the burden of at least one of psychological reactions including anxiety or depression or stress or insomnia was eligible. Heterogeneity was assessed using I2 statistic and results were synthesized using random-effect meta-analysis.
Results:
Out of 49 eligible studies, 41 databases from 37 studies reported anxiety, 39 databases (35 studies) reported depression, 20 studies reported stress and 12 databases from 11 studies reported insomnia. The overall prevalence for anxiety, depression, stress, and insomnia was 26.3%, 25.9%, 26.2%, and 31.3%, respectively. Prevalence of anxiety, depression, stress, and insomnia were found highest among the frontline healthcare as compared to general healthcare workers and the general population.
Conclusion:
Anxiety, depression, stress, and insomnia were more prevalent among frontline health-care workers compared to general. Such increased prevalence is prompting toward the global mental health emergency. Therefore, a call of urgent attention and pan-region effective mental-health intervention are required to mitigate these psychological reactions.
Keywords: Anxiety, COVID-19, depression, frontline healthcare workers, insomnia, stress
INTRODUCTION
Novel pneumonia caused by the coronavirus disease (COVID-19) has emerged in the Chinese city of Wuhan (Hubei province) in late December 2019 and spread rapidly nationwide and all over the world.[1] The World Health Organization declared an international public health emergency on January 30, 2020. The virus spread in nearly 213 countries and territories with 66.2 million confirm cases, 1.5 million confirmed deaths, and 45.8 million recovered according to the global data reported by the Worldometer on December 4, 2020.
During this global pandemic fear of rapid infection spread, falling sick and dying social isolation, and extended quarantine are expected to influence mental health. Fear related to shortages of vaccine, critical care support fear of financial crisis, joblessness, and frozen economy, during the lockdown, may play the lead role to increase the burden of mental health illness. Such psychological burden had been reported among the COVID-19 patients, healthcare personnel, medical students, and older as well as the general population.[1,2,3]
During the Ebola outbreak in West Africa, the greater number of healthy people was mentally traumatized compare to the number of infected people and remained longer. Such historical devastation prompts toward another global mental health challenge during the COVID-19 pandemic. Therefore, it is important to understand the increased burdens of mental health outcomes as a consequence of the COVID-19 pandemic.
Estimates of psychological burdens vary across the studies. Such variations might occur because these studies carried on different population, with varying sample sizes and dealt with different scales of mental-illness assessment.
In this study, a systematic review and meta-analysis was conducted to assess the burden of mental health outcomes predominantly on the prevalence of anxiety, depression, stress, and insomnia during COVID-19 global emergency among three group of the population, i.e. frontline health-care workers (FHW), nonFHWs (NFHW) and the general population who are not healthcare workers.
MATERIAL AND METHODS
Protocol of the present systematic review was registered with the PROSPERO database (Registration Number: CRD42020186229). The present systematic review manuscript is designed as per the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analysis.
A systematic literature search in electronic databases including Embase, PubMed, and Scopus between January 1, 2020, and May 25, 2020, was used to find the eligible studies. The used search term was “(COVID-19 OR SARS-CoV-2 OR 2019-nCoV OR coronavirus) AND (Depression OR Anxiety OR stress OR insomnia OR “psychological distress”OR “Psychiatric illness” OR “Mental Health”).” In addition, a supplementary search was conducted using Google Scholar. All the published or unpublished studies assessing mental illness using scientific rating scale and reporting overall prevalence/graded prevalence (mild, moderate, and severe) of psychological anxiety or depression or stress or insomnia as an impact of COVID-19 using original data were considered eligible.
All the retrieved articles first were screened based on title and abstract and then reviewed for the full text of potentially eligible articles independently and in duplicate by both authors (B. T. and M. P.). Data regarding study identification, population, sample size, the prevalence of anxiety, depression, stress, and insomnia (or categorized on the graded scale like normal, mild, moderate, and severe), scale for outcome measurement and quality-related variables were extracted by both authors independently on the preprepared form. All the discrepancies were resolved by discussion.
The modified Newcastle-Ottawa Quality Assessment Scale was used to assess the methodological quality for cross-sectional studies.[4] Since the present meta-analysis focused only prevalence of mental health outcomes, the quality of the studies was judged based on four criteria only including representative sample, adequate sample size, low nonresponse rate, and objective outcome measurement. Hence, the range of quality score was 0–5. Quality scores were categorized as 4/5 = Good, 3 = Average, and 2/0 = Poor. Both the reviewer (BT and MP) independently assessed the quality of eligible studies.
Proportion of psychological stress, anxiety, depression, and insomnia as overall, as well as on the graded scale of mild, moderate, and severe were pooled using fixed-effect inverse variance method or DerSimonianand Liard random effect method[5] depending on heterogeneity measured using I2 statistic.[6] Subgroup analysis was performed based on type of population, i. e., FHW, NFHW, and other general.
we used egger's test[7] to assess publication bias. The quality of our evidence was graded using Grading of Recommendations, Assessment, Development, and Evaluations approach.[8]
RESULTS
A total of 2337 unique studies were identified by searching the databases. Out of these, 111 studies qualified for full-text review [Figure 1]. Of these 111 studies, 63 were excluded because of various reasons mentioned in Figure 1.
Figure 1.
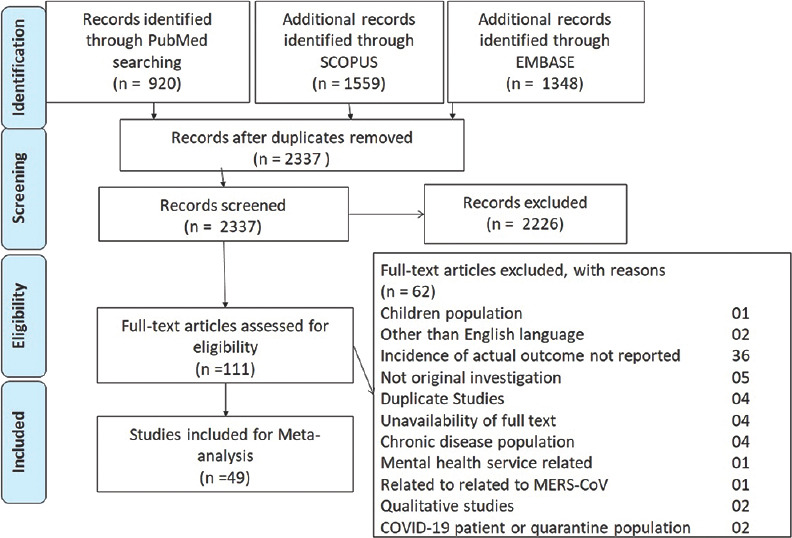
Preferred reporting items for systematic reviews and meta-analysis flow chart for eligible studies
A total of 49 studies comprised 55 datasets of the diverse population for 147142 individuals were included. Of these 55 datasets, 32 datasets involving 123650 individuals reported mental health burden for the general population.[3,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]; 15 datasets reported mental health of 8335 frontline healthcare workers[22,39,40,41,42,43,44,45,46,47,48,49,50,51,52] and eight datasets reported for 12,462 nonfrontline health-care workers.[2,15,26,53,54,55,56] Study level characteristics are presented in Supplementary Table S1.
Table S1.
Study level characteristics
| Study | Country | Population | Sample size | Anxiety prevalence (%) | Depression prevalence (%) | Stress prevalence (%) | Insomnia prevalence (%) |
|---|---|---|---|---|---|---|---|
| Cao W | China | Medical students | 7143 | 24.86 | NR | NR | NR |
| Wang C | China | General population | 1210 | 36.36 | 30.33 | 32.15 | NR |
| Lai J | China | Healthcare workers in fever clinic and COVID-19 wards | 1257 | 44.55 | 50.44 | 71.52 | 33.97 |
| Wang Y | China | General population | 600 | 6.33 | 17.17 | NR | NR |
| Huang JZ | China | Medical-staff involved in COVID-19 | 230 | 23.04 | NR | NR | NR |
| Qui J | China, Hongcong, Macau, Taiwan | General population | 52730 | NR | NR | 34.43 | NR |
| Lu W | China | Medical workforce fighting COVID-19 and administrative staff | 2299 | 25.51a, 18.68c | 12.1a, 8.17c | NR | NR |
| Nguyen HC | Viatnam | People visiting OPD of a hospital | 3947 | NR | 7.45 | NR | NR |
| Zhang WR | China | Medical as well as nonmedical health worker | 2182 | 10.45 | 10.63 | NR | 33.87 |
| Zhang Y | China | Local people | 263 | NR | NR | 7.6 | NR |
| Ahmed MZ | China | Wechat users | 1074 | 28.96 | 37.15 | NR | NR |
| Chen Y | China | Peadiatric medical staff working at high risk place | 105 | 18.1 | 29.52 | NR | NR |
| Chew NWS | Singapore-India | Health care workers | 906 | 15.67 | 10.6 | 5.19 | NR |
| Lei L | China | General population | 1593 | 8.35 | 14.69 | NR | NR |
| Moghanibasi AM | Iran | General population | 10754 | 50.88 | NR | NR | NR |
| Sacham M | Israel | Dentist and dental hygienist | 338 | NR | NR | 11.54 | NR |
| Tan W | Singapore | Working population | 673 | 6.09 | 5.94 | 3.27 | 14.56 |
| Yuvan S | China | General population | 939 | NR | NR | NR | 56.12 |
| Zhu S | China | Health care workers frontline as well as nonfrontline | 2279 | 19.69a, 22c | 21.25a, 21.69c | NR | NR |
| Li J | China | General population (no psychiatric history) included few COVID-cases | 5033 | 20.45 | 20.45 | NR | NR |
| Zhou SJ | China | Adolecent | 8079 | 37.38 | 43.73 | NR | NR |
| Liang L | China | Young general people | 584 | NR | NR | 14.38 | NR |
| Zhang J | China | COVID-19 infected, quarantined patients and general population | 57 | 43.88c, 26.31d, 10e | 62.24c, 36.84d, 12e | NR | NR |
| Hao F | China | Healthy subjects | 109 | 6.42 | 1.83 | 0.92 | 25.69 |
| Jahanshahi AA | Iran | Iranian adults | 1058 | NR | NR | 61.06 | NR |
| Ren Y | China | General population | 1172 | 13.31 | 18.77 | 7.00 | 7.25 |
| Xingxing Li | China | Frontline healthcare | 948 | NR | NR | NR | 32.81 |
| González-Sanguino C | Spain | General population | 3484 | 21.58 | 18.69 | 15.79 | NR |
| Du J | China | Frontline healthcare workers | 310 | 9.03 | 5.48 | NR | NR |
| Voitsidis P | Greece | Elderly population | 2363 | NR | NR | NR | 37.62 |
| Odriozola-González P | Spain | Students and workers of a Spanish university | 3,707 | 35.18 | 48.10 | 40.33 | NR |
| Abdessater M | France | Frontline g French urologists in training | 275 | NR | NR | 91.64 | NR |
| Sherman A. Lee | USA | MTurk workers | 1237 | 35.97 | 40.02 | NR | NR |
| Chen-Yun Liu | China | Frontline healthcare workers | 512 | 12.50 | NR | NR | NR |
| Ferit Durankus | Turkey | Pregnant women | 260 | NR | 35.38 | NR | NR |
| Tawfiq Choudhury | England | Frontline healthcare workers | 65 | 60.98 | 53.85 | NR | NR |
| Nicola Cellini | Italy | General population | 1310 | 32.60 | 24.20 | 50.15 | NR |
| Selçuk Özdin | Turkey | General Population | 343 | 45.19 | 23.62 | NR | NR |
| Junling Gao | China | General population | 4872 | 22.60 | 48.30 | NR | NR |
| Naiara Ozamiz-Etxebarria | Spain | General population | 976 | 26.02 | 18.85 | 23.67 | NR |
| Michael Y Ni | China | General population and health professonals | 1791 | 21.96b, 23.84c | 19.59 | NR | NR |
| Andrea Amerio | Italy | Frontline general practitioners | 131 | NR | 22.90 | NR | NR |
| Chenxi Zhang | China | Frontline medical staffs | 1563 | 44.72 | 50.67 | NR | 36.08 |
| Juhong Zhu | China | Frontline healthcare workers | 165 | 20.00 | 44.24 | NR | NR |
| Cristina Mazza | Italy | General population | 2766 | 18.69 | 32.75 | 27.19 | NR |
| Ugo Consolo | Italy | Dental practitioners | 356 | 57.30 | NR | NR | NR |
| Yun Li | China | General population | 3637 | 27.50 | 31.21 | 17.60 | 33.71 |
| Huang Y | China | General population and health care workers | 7236 | 35.64b, 34.85c | 19.82b, 20.21c | NR | 19.82b, 15.76c |
a Frontline Health Care Worker, bNonfrontline Healthcare Worker, cGeneral Population, dCOVID-19 patients, eQuarantined. NR: Not reported, COVID-19: Coronavirus disease-2019, OPD: Outpatient department
Group-wise data were extracted for the studies which reported mental health for more than group to facilitate subgroup comparison.[15,22,26,39,43]
The majority of the studies (32 out of 49) were conducted in China. Among rest of the 17 studies, four studies were conducted in Italy,[10,23,41,54] three in Spain,[13,27,28] two [16,24] from Iran, two from Turkey[11,29] and one-one study was conducted in Israel,[55] Singapore,[53] Greece,[33] France,[40] USA,[17] and England.[43] Further, the study conducted in Singapore[53] included data for India as well as Singapore. Hence, country-level data were extracted for this study.
The severity of psychological health parameters were reported by 18 studies (2,3,9,14,18,24,28,32,34,38,42,43,45,46,48,49,51,54); 17 for anxiety (2,3,9,14,18,24,28,32,34,38,42,43,45,46,48,51,54)); 11 for depression (3,9,14,18,28,32,34,38,43,46,51); five for stress (3,14,28,32,46) and four for insomnia (9,32,46,49).
Out of the total 49 included studies, 30 studies had “Good” quality (11 studies had score 5 and 19 studies had score 4), 18 studies were grades as “average” quality with score 3 and one study had poor quality with score 2 [Supplementary Table S2]. Most of the eligible studies collected their data using social media platform. These studies could include data for social media users not from any well-defined population and hence, these studies did not have representative sample. Formal sample size calculation or power assessment was done only for two studies. Further, we found a wide heterogeneity in the reported results. These facts lower the confidence in our graded evidence. The moderate grade for evidence of anxiety and depression suggests that further studies may less likely to change the current evidence [Table S3]. We could not find significant publication bias for any of the outcomes.
Table S2.
Quality assessment of eligible studies
| Study | Sample representative | Sample size | Outcome assessment | Nonresponse rate | Quality score |
|---|---|---|---|---|---|
| Cao W | 1 | 1 | 2 | 1 | 5 |
| Wang C | 0 | 1 | 2 | 1 | 4 |
| Lai J | 1 | 1 | 2 | 1 | 5 |
| Wang Y | 0 | 0 | 2 | 1 | 3 |
| Huang JZ | 1 | 0 | 2 | 1 | 4 |
| Qui J | 0 | 1 | 2 | 0 | 3 |
| Lu W | 1 | 1 | 2 | 1 | 5 |
| Nguyen HC | 1 | 1 | 2 | 1 | 5 |
| Zhang WR | 0 | 1 | 2 | 0 | 3 |
| Zhang Y | 0 | 0 | 2 | 0 | 2 |
| Ahmed MZ | 0 | 1 | 2 | 0 | 3 |
| Chen Y | 1 | 0 | 2 | 0 | 3 |
| Chew NWS | 1 | 1 | 2 | 1 | 5 |
| Lei L | 0 | 1 | 2 | 0 | 3 |
| Moghanibasi AM | 0 | 1 | 2 | 0 | 3 |
| Sacham M | 1 | 0 | 2 | 0 | 3 |
| Tan W | 0 | 1 | 2 | 0 | 3 |
| Yuvan S | 0 | 1 | 2 | 0 | 3 |
| Zhu S | 0 | 1 | 2 | 0 | 3 |
| Yin Q | 0 | 0 | 2 | 1 | 3 |
| Li J | 1 | 1 | 2 | 1 | 5 |
| Zhou SJ | 1 | 1 | 2 | 1 | 5 |
| Liang L | 0 | 0 | 2 | 1 | 3 |
| Zhang J | 0 | 0 | 2 | 1 | 3 |
| Hao F | 0 | 0 | 2 | 1 | 3 |
| Jahanshahi, AA | 0 | 1 | 2 | 1 | 4 |
| Ren Y | 0 | 1 | 2 | 1 | 4 |
| Xingxing Li | 0 | 1 | 2 | 1 | 4 |
| González-Sanguino C | 1 | 1 | 2 | 1 | 5 |
| Du J | 0 | 0 | 2 | 1 | 3 |
| Voitsidis P | 0 | 1 | 2 | 1 | 4 |
| Odriozola-González P | 0 | 1 | 2 | 1 | 4 |
| Abdessater M | 1 | 1 | 2 | 1 | 5 |
| Sherman A. Lee | 0 | 1 | 2 | 1 | 4 |
| Chen-Yun Liu | 1 | 1 | 2 | 1 | 5 |
| Ferit Durankus | 0 | 0 | 2 | 1 | 3 |
| Tawfiq Choudhury | 0 | 0 | 2 | 1 | 3 |
| Nicola Cellini | 0 | 1 | 2 | 1 | 4 |
| Selçuk Özdin | 0 | 1 | 2 | 1 | 4 |
| Junling Gao | 0 | 1 | 2 | 1 | 4 |
| Naiara Ozamiz-Etxebarria | 0 | 1 | 2 | 1 | 4 |
| Michael Y Ni | 0 | 1 | 2 | 1 | 4 |
| Andrea Amerio | 0 | 1 | 2 | 1 | 4 |
| Chenxi Zhang | 0 | 1 | 2 | 1 | 4 |
| Juhong Zhu | 1 | 1 | 2 | 1 | 5 |
| Cristina Mazza | 0 | 1 | 2 | 1 | 4 |
| Ugo Consolo | 0 | 1 | 2 | 1 | 4 |
| Yun Li | 0 | 1 | 2 | 1 | 4 |
| Huang Y | 0 | 1 | 2 | 1 | 4 |
Table S3.
Grading of confidence in the reported results for various outcomes
| Number of studies | Certainty assessment |
Effect |
Certainty | Importance | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Number of events | Number of individuals | Rate (95% CI) | |||
| Anxiety | |||||||||||
| 43 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Publication bias strongly suspected strong association all plausible residual confounding would reduce the demonstrated effectc | 27,525 | 90,080 | Event rate 26.59 per 100 (22.81-30.36) | ⨁⨁◯◯ LOW | Important |
| Anxiety among frontline health care workers | |||||||||||
| 10 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Strong association all plausible residual confounding would reduce the demonstrated effect | 2065 | 6545 | Event rate 27.2 per 100 (18.1-36.31) | ⨁⨁⨁◯ Moderate | Important |
| Anxiety among second line health care worker | |||||||||||
| 7 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Strong association all plausible residual confounding would reduce the demonstrated effect | 3199 | 12,124 | Event rate 26.89 per 100 (20.35-33.43) | ⨁⨁⨁◯ moderate | Important |
| Anxiety among general population | |||||||||||
| 24 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Publication bias strongly suspected strong association all plausible residual confounding would reduce the demonstrated effectc | 21,778 | 68,742 | Event rate 25.87 per 100 (20.51-31.24) | ⨁⨁◯◯ low | Important |
| Mild anxiety | |||||||||||
| 18 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Publication bias strongly suspected strong association all plausible residual confounding would reduce the demonstrated effectc | Event rate 16.69 per 100 (12.27-21.11) | ⨁⨁◯◯ Low | Not important | ||
| Moderate anxiety | |||||||||||
| 18 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Publication bias strongly suspected all plausible residual confounding would reduce the demonstrated effectc | Event rate 7.34 per 100 (4.4-10.27) | ⨁◯◯◯ very low | Important | ||
| Severe anxiety | |||||||||||
| 17 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Publication bias strongly suspected all plausible residual confounding would reduce the demonstrated effectc | Event rate 5.39 per 100 (3.19-7.59) | ⨁◯◯◯ very low | Critical | ||
| Depression | |||||||||||
| 43 | Observational studies | Seriousd | Very seriousb | Not serious | Not serious | Publication bias strongly suspected strong association all plausible residual confounding would reduce the demonstrated effectc | 21,019 | 77,932 | Event rate 26.17 per 100 (21.84-30.5) | ⨁⨁◯◯ Low | Critical |
| Depression among frontline health care worker | |||||||||||
| 9 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Strong association all plausible residual confounding would reduce the demonstrated effect | 1927 | 5958 | Event rate 32.1 per 100 (17.97-46.22) | ⨁⨁⨁◯ moderate | Critical |
| Depression among second line health care workers | |||||||||||
| 5 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Strong association all plausible residual confounding would reduce the demonstrated effect | 815 | 4625 | Event rate 15.72 per 100 (11.28-20.15) | ⨁⨁⨁◯ moderate | Critical |
| Depression among general population | |||||||||||
| 25 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Publication bias strongly suspected strong association all plausible residual confounding would reduce the demonstrated effectc | 17,496 | 62,195 | Event rate 25.87 per 100 (20.22-31.53) | ⨁⨁◯◯ low | Critical |
| Mild depression | |||||||||||
| 12 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Publication bias strongly suspected strong association all plausible residual confounding would reduce the demonstrated effectc | Event rate 20.81 per 100 (13.94-27.69) | ⨁⨁◯◯ Low | Not important | ||
| Moderate depression | |||||||||||
| 13 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Publication bias strongly suspected all plausible residual confounding would reduce the demonstrated effectc | Event rate 7.41 per 100 (4.93-9.9) | ⨁◯◯◯ very low | Important | ||
| Severe depression | |||||||||||
| 12 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Publication bias strongly suspected all plausible residual confounding would reduce the demonstrated effectc | Event rate 4.61 per 100 (2.65-6.58) | ⨁◯◯◯ very low | Critical | ||
| Stress | |||||||||||
| 20 | Observational studies | Seriousa | Very seriousb | Seriousd | Not serious | Strong association all plausible residual confounding would reduce the demonstrated effect | 25,210 | 79,138 | Event rate 26.16 per 100 (17.73-34.59) | ⨁⨁◯◯ low | Important |
| Stress among frontline health care worker | |||||||||||
| 3 | Observational studies | Seriouse | Very seriousb | Seriousd | Seriousc | Strong association all plausible residual confounding would reduce the demonstrated effect | 1165 | 1903 | Event rate 55.63 0.36 110.9 per 100 (0.36-100) | ⨁◯◯◯ very low | Important |
| Stress among second line health care worker | |||||||||||
| 3 | Observational studies | Seriousa | Very seriousb | Seriousd | Seriousc | All plausible residual confounding would reduce the demonstrated effect | 86 | 1244 | Event rate 7.01 per 100 (3.11-10.92) | ⨁◯◯◯ very low | Important |
| Stress among general population | |||||||||||
| 13 | Observational studies | Seriousa | Very seriousb | Seriousd | Not serious | Strong association all plausible residual confounding would reduce the demonstrated effect | 23,892 | 73,506 | Event rate 25.54 per 100 (17.8-33.29) | ⨁⨁◯◯ low | Important |
| Insomnia | |||||||||||
| 11 | Observational studies | Seriousa | Very seriousb | Not serious | Not serious | Strong association all plausible residual confounding would reduce the demonstrated effect | 7490 | 27,775 | Event rate 32.87 per 100 (23.94-41.8) | ⨁⨁⨁◯ moderate | Important |
| Insomnia among frontline health care worker | |||||||||||
| 3 | Observational studies | Seriousa | Seriousb | Not serious | Seriousd | Publication bias strongly suspected strong associationc | 1362 | 3828 | Event rate 34.44 per 100 (32.54-36.34) | ⨁◯◯◯ very low | Important |
| Insomnia among second line health care worker | |||||||||||
| 2 | Observational studies | Very seriousb, d | Seriousb | Not serious | Seriousd | Strong association all plausible residual confounding would reduce the demonstrated effect | 1270 | 3505 | Event rate 33.96 per 100 (32.48-35.43) | ⨁⨁◯◯ low | Important |
| Insomnia among general population | |||||||||||
| 6 | Observational studies | Seriousb | Seriousb | Not serious | Not serious | Strong association all plausible residual confounding would reduce the demonstrated effect dose response gradient | 4858 | 20,442 | Event rate 29.36 per 100 (17.02-41.69) | ⨁⨁⨁⨁ high | Important |
aNonrandom sampling was used for most of the studies, bHeterogeneity index measured using I2 statistic is very high, cFew number of studies, dThere was wide variety in the scales and definition of stress among studies, eThe quality assessed by new Castel Ottawa scale is poor. CI: Confidence interval
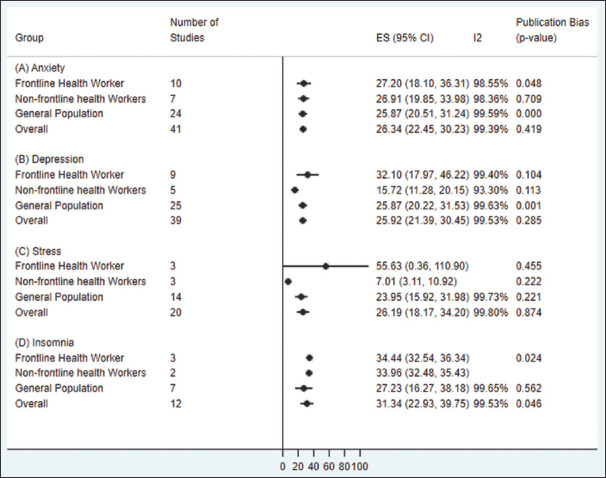
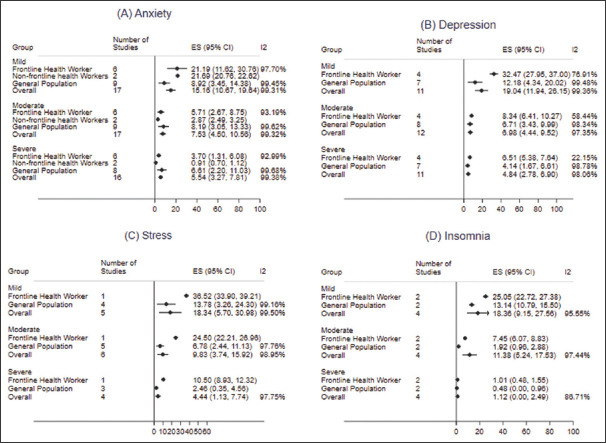
Overall pooled prevalence of anxiety was 26.3% (95% confidence interval [CI]: 22.4%–30.2%) which was observed relatively higher among the FHWs (27.2%; 95% CI: 18.1%–36.3%) followed by NFHW (26.9%; 95% CI: 19.5%–34.0%) and general population (25.9%; 95% CI: 20.5%–31.2%) [Figure 2a]. Meta-analysis of prevalence on severity scale based on 17 available studies resulted that most of the individuals had mild anxiety (15.2%; 95% CI: 10.7%–9.6%). Moderate anxiety (7.5%; 95% CI: 4.5%–10.6%) and severe anxiety (5.5%; 95% CI: 3.3%–7.8%) were observed among very few individuals [Figure 3a]. However, moderate and severe anxiety were observed highest among the general population.
Figure 2.
Prevalence of (A) Anxiety, (B) Depression, (C) Stress and (D) Insomnia among various population groups.
Figure 3.
Severity of (A) anxiety, (B) Depression, (C) Stress and (D) Insomnia among various population groups
A total of 25.9% (95% CI: 21.4%–30.5%) were identified to have depression [Figure 2b]. This prevalence was found highest among FHWs (32.1%; 95% CI: 18.0%–46.2%) followed by general population (25.9%; 95% CI: 21.4%–30.5%) and NFHW (15.7%; 95% CI: 11.3%–20.1%) [Figure 2b]. On the severity scale of depression, 19% of the individuals had mild depression, 7.0% had moderate, and very few (4.8%) were severe cases [Figure 3b]. Further, depression burden was observed highest among the frontline health workers in all the three groups of mild, moderate, and severe [Figure 3b].
[Figure 2c] showed the overall stress prevalence as 26.2% (95% CI: 18.2%–34.2%). Our pooled effect of stress prevalence was found highest among the FHWs (55.6%; 95% CI: 0.36%–100%) followed by general population (23.9%; 95% CI: 15.9%–32.0%) and NFHW (7.0%; 95% CI: 3.1%–10.9%). Based on five reported studies, pooled stress prevalence resulted into 18.3% mild, 9.8% moderate, and only 4.4% severe stress levels [Figure 3c].
Overall insomnia burden was found as 31.3% (95% CI: 22.9%–39.7%) [Figure 2d]. Pooled effect of insomnia prevalence among the general population was observed as 27.2% (95% CI: 16.3%–38.2%), a lower than the prevalence among FHWs (34.4%; 95% CI: 32.5%–36.3%) and NFHWs (34.0%; 95% CI: 32.5%–35.4%) [Figure 2d]. Further on the severity graded scale, mild, moderate, and severe level of insomnia were observed as 18.4%, 11.4%, and 1.1%, respectively [Figure 3d].
DISCUSSION
This systematic review and meta-analysis were based on the data extracted from 49 different studies. Most of these studies were conducted in China, the country where COVID-19 emerged, although studies conducted in Taiwan, Vietnam, Singapore, Italy, Israel, Iran, Greece, Spain, USA, Turkey, and England were also included. Studies varied in sample size from 57 to 52730. One largest study[30] incorporated information for multiple countries such as China, Macau, Hong Kong, and Taiwan. Most of the studies reported prevalence of anxiety and depression and very few reported for stress and insomnia. Various scales were used to measure these outcomes but most of the variability found for stress outcome. All the included studies were performed with cross-sectional design and majority of these studies were based on web-based survey and therefore lacking random sampling method of data collection. Grade approach suggested there is moderate level of confidence in our finding for anxiety, depression, and insomnia but low level of confidence for stress.
The burden of anxiety, depression, stress, and insomnia were found highest among the FHWs. We also found that after FHWs, the burden of depression and stress was highest among the general population, and the burden of anxiety and insomnia was highest among the NFHWs.
During this pandemic, a handful of reviews and meta-analyses on the prevalence of mental health outcomes were reported among the healthcare workers and general population. However, all these reviews are based on the small number of studies, majorly based on Chinese studies and focusing on a particular population. In addition to the Chinese studies, our review attempted to include the most updated global studies targeting wide range of the population. We also attempted the overall prevalence based on the graded scale of severity for all the outcomes [Table S3]. The burden of the mild stage was observed as highest followed by moderate and severe stages for all four outcomes. Similar exploration on graded scale was also attempted among the various subpopulations, i.e. FHWs, NFHWs, general population, COVID-19-infected patients, and quarantine people.
According to the recent report of Our World in Data, the prevalence of anxiety disorder and depression was observed as 3.8% and 3.4%, respectively. Our finding suggests how the psychological pressure during the pandemic public health crisis increased the mental health burden. According to a recent meta-analysis report in 2017,[57] insomnia prevalence in the general population of China observed as 15% which was far lower than the insomnia prevalence among the general population observed in our study during the COVID-19 pandemic. Similarly, the global prevalence of posttraumatic stress disorder was reported as 15.3%.[58] These reports and our finding suggests that the burden of insomnia and stress in the general population, increased almost to double, was certainly a consequences of COVID-19 fear.
During the crucial public health emergency of COVID-19, the frontlines healthcare professionals feel fear of getting sick and spreading the infection to their families, other patients, and coworkers. Our comparative analysis results show that the prevalence of all four mental health outcomes was significantly high among the frontline healthcare professionals as compared to the general population. These findings suggest the positive correlation between the management of COVID-19 patients by healthcare professionals and increased psychological responses among them.
Although surveys and studies in the current COVID-19 emergency confirmed new psychological responses might have accelerated the existing burden of mental health outcome during the COVID-19 outbreak, this burden may further increase and may stay longer depending on the time required to control the infection. Studies on the risk factors associated with the various mental health problems is need to be explored to manage with evidence-based interventions. Some of the individual-level risk factors may also get effected by the country-level parameters such as countries' policies on virus prevention at the community level, healthcare infrastructure, climatic condition, concurrent burden of COVID-19 and its spreading speed. Policymakers need to make effective decisions about where to focus their efforts to mitigate such burden.
CONCLUSION
Overall COVID-19 pandemic has been impacting on the mental health of the worldwide general population, but frontline healthcare warriors had shown relatively having more stress, anxiety, depression, and insomnia as compared to general healthcare workers and general. However, mostly, these mental ailments are mild to moderate in severity. Our finding suggests that the new psychological reactions and sudden increment in the burden of mental health outcomes during the COVID-19 pandemic is prompting toward another global health emergency. Therefore, a call of urgent attention and pan-region intervention are required to manage the current burden of mental health outcomes and further for future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank the Department of Research, Kalinga Institute of Medical Sciences, KIIT University to make available all the resources to conduct this study.
REFERENCES
- 1.Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–6. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alshabanat A, Zafari Z, Albanyan O, Dairi M, FitzGerald JM. Asthma and COPD Overlap Syndrome (ACOS): A systematic review and meta analysis. PLoS One. 2015;10:e0136065. doi: 10.1371/journal.pone.0136065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pathak M, Dwivedi SN, Thakur B. Comparative role of various methods of estimating between study variance for meta-analysis using random effect method. Clin Epidemiol Glob Health. 2020;8:85–189. [Google Scholar]
- 6.Pathak M, Dwivedi SN, Deo SV, Sreenivas V, Thakur B. Which is the preferred measure of heterogeneity in meta-analysis and why? A revisit. Biostat Biom Open Acc. 2017;1:1–7. [Google Scholar]
- 7.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldet G, Howick J. Understanding GRADE: An introduction. J Evid Based Med. 2013;6:50–4. doi: 10.1111/jebm.12018. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, Ahmad A. Epidemic of COVID-19 in China and associated Psychological Problems. Asian J Psychiatry. 2020;51:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29:e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Durankuş F, Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: A preliminary study. J Matern-Fetal Neonatal Med. 2020 doi: 10.1080/14767058.2020.1763946. [Epub ahead of print];1-7. doi:10.1080/14767058.2020.1763946. [DOI] [PubMed] [Google Scholar]
- 12.Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15:e0231924. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172–6. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–6. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang Y, Zhao N. Chinese mental health burden during the COVID-19 pandemic. Asian J Psychiatry. 2020;51:102052. doi: 10.1016/j.ajp.2020.102052. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 16.Jahanshahi AA, Dinani MM, Madavani AN, Li J, Zhang SX. The distress of Iranian adults during the Covid-19 pandemic – More distressed than the Chinese and with different predictors. Brain Behav Immun. 2020;87:124–5. doi: 10.1016/j.bbi.2020.04.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee SA, Jobe MC, Mathis AA. Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol Med. 2020 doi: 10.1017/S003329172000121X. [Epub ahead of print]:1-2. doi: 10.1017/S003329172000121X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Med Sci Monit. 2020;26:e924609. doi: 10.12659/MSM.924609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li J, Yang Z, Qiu H, Wang Y, Jian L, Ji J, et al. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry. 2020;19:249–50. doi: 10.1002/wps.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Y, Qin Q, Sun Q, Sanford LD, Vgontzas AN, Tang X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin Sleep Med. 2020;16:1417–8. doi: 10.5664/jcsm.8524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liang L, Ren H, Cao R, Hu Y, Qin Z, Li C, et al. The effect of COVID-19 on youth mental health. Psychiatr Q. 2020;91:841–52. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. Int J Environ Res Public Health. 2020;17:3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr. 2020;51:102076. doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nguyen HC, Nguyen MH, Do BN, Tran CQ, Nguyen TTP, Pham KM, et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: The potential benefit of health literacy. J Clin Med. 2020;9:965. doi: 10.3390/jcm9040965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ni MY, Yang L, Leung CMC, Li N, Yao XI, Wang Y, et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: Cross-sectional survey. JMIR Ment Health. 2020;7:e19009. doi: 10.2196/19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Odriozola-González P, Planchuelo-Gómez Á, Irurtia MJ, de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020;290:113108. doi: 10.1016/j.psychres.2020.113108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. 2020;36:e00054020. doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- 29.Özdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry. 2020;66:504–11. doi: 10.1177/0020764020927051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen Psychiatr. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ren Y, Zhou Y, Qian W, Li Z, Liu Z, Wang R, et al. Letter to the Editor “A longitudinal study on the mental health of general population during the COVID-19 epidemic in China”. Brain Behav Immun. 2020;87:132–3. doi: 10.1016/j.bbi.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tan W, Hao F, McIntyre RS, Jiang L, Jiang X, Zhang L, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. 2020;87:84–92. doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Voitsidis P, Gliatas I, Bairachtari V, Papadopoulou K, Papageorgiou G, Parlapani E, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020;289:113076. doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2021;26:13–22. doi: 10.1080/13548506.2020.1746817. [DOI] [PubMed] [Google Scholar]
- 35.Yuan S, Liao Z, Huang H, Jiang B, Zhang X, Wang Y, et al. Comparison of the indicators of psychological stress in the population of Hubei province and non-endemic provinces in china during two weeks during the coronavirus disease 2019 (COVID-19) outbreak in February 2020. Med Sci Monit Int Med J Exp Clin Res. 2020;26:e923767. doi: 10.12659/MSM.923767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, et al. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. 2020;87:49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: A cross-sectional study. Int J Environ Res Public Health. 2020;17:2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020;29:749–58. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu S, Wu Y, Zhu CY, Hong WC, Yu ZX, Chen ZK, et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav Immun. 2020;87:56–8. doi: 10.1016/j.bbi.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abdessater M, Rouprêt M, Misrai V, Matillon X, Gondran-Tellier B, Freton L, et al. COVID19 pandemic impacts on anxiety of French urologist in training: Outcomes from a national survey. Prog Urol. 2020;30:448–55. doi: 10.1016/j.purol.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Amerio A, Bianchi D, Santi F, Costantini L, Odone A, Signorelli C, et al. COVID-19 pandemic impact on mental health: A web-based cross-sectional survey on a sample of Italian general practitioners. Acta Bio-Medica Atenei Parm. 2020;91:83–8. doi: 10.23750/abm.v91i2.9619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen Y, Zhou H, Zhou Y, Zhou F. Prevalence of self-reported depression and anxiety among pediatric medical staff members during the COVID-19 outbreak in Guiyang, China. Psychiatry Res. 2020;288:113005. doi: 10.1016/j.psychres.2020.113005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Choudhury T, Debski M, Wiper A, Abdelrahman A, Wild S, Chalil S, et al. COVID-19 pandemic: Looking after the mental health of our healthcare workers. J Occup Environ Med. 2020;62:e373–6. doi: 10.1097/JOM.0000000000001907. [DOI] [PubMed] [Google Scholar]
- 44.Du J, Dong L, Wang T, Yuan C, Fu R, Zhang L, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. 2020;67:144–5. doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38:192–5. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- 46.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li X, Yu H, Bian G, Hu Z, Liu X, Zhou Q, et al. Prevalence, risk factors, and clinical correlates of insomnia in volunteer and at home medical staff during the COVID-19. Brain Behav Immun. 2020;87:140–1. doi: 10.1016/j.bbi.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol Infect. 2020;148:e98. doi: 10.1017/S0950268820001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wu K, Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Monit Basic Res. 2020;26:e924085. doi: 10.12659/MSMBR.924085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yin Q, Sun Z, Liu T, Ni X, Deng X, Jia Y, et al. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019 (COVID-19) Clin Psychol Psychother. 2020;27:384–95. doi: 10.1002/cpp.2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. Survey of Insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, et al. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front Psychiatry. 2020;11:386. doi: 10.3389/fpsyt.2020.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chew NW, Lee GK, Tan BY, Jing M, Goh Y, Ngiam NJ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–65. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Consolo U, Bellini P, Bencivenni D, Iani C, Checchi V. Epidemiological aspects and psychological reactions to COVID-19 of dental practitioners in the northern Italy districts of Modena and Reggio Emilia. Int J Environ Res Public Health. 2020;17:3459. doi: 10.3390/ijerph17103459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shacham M, Hamama-Raz Y, Kolerman R, Mijiritsky O, Ben-Ezra M, Mijiritsky E. COVID-19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. Int J Environ Res Public Health. 2020;17:2900. doi: 10.3390/ijerph17082900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89:242–50. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cao XL, Wang SB, Zhong BL, Zhang L, Ungvari GS, Ng CH, et al. The prevalence of insomnia in the general population in China: A meta-analysis. PLoS One. 2017;12:e0170772. doi: 10.1371/journal.pone.0170772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. Lancet. 2019;394:240–8. doi: 10.1016/S0140-6736(19)30934-1. [DOI] [PMC free article] [PubMed] [Google Scholar]