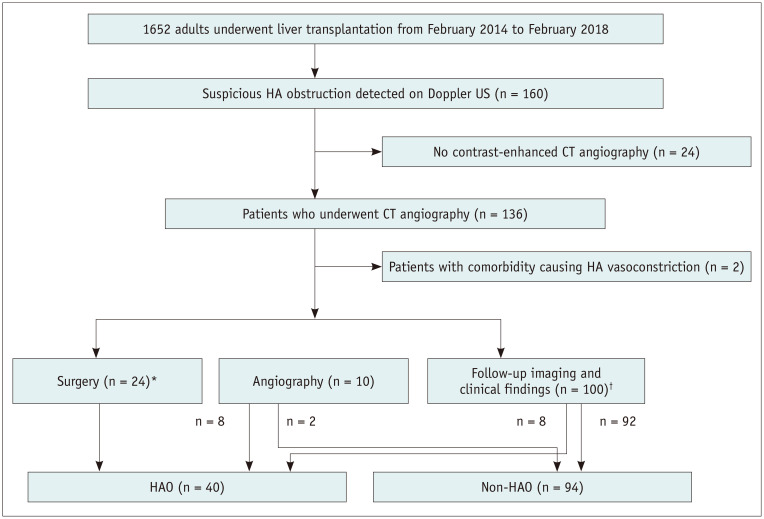
Fig. 1. Flow diagram describing the flow of the study population.
*The surgery included angioplasty (n = 20) and liver re-transplantation (n = 4), †Follow-up imaging and clinical findings determined HAO when there was persistent no flow or progressive change from the tardus parvus pattern to no flow on Doppler US follow-up studies, associated with non-anastomotic biliary complications, such as bile duct necrosis/biloma, development of multifocal subsegmental ischemia/infarction, and HAO at the anastomotic site with a collateral reconstruction of the intrahepatic artery branches on follow-up CT, and consistent clinical findings of graft dysfunction or even failure. Non-HAO was defined as normalization of Doppler US abnormalities and no association with complications described above within 6 months of follow-up. HA = hepatic artery, HAO = hepatic artery occlusion, US = ultrasound