Graphical abstract
Note- Fit path model for 941 participants. Standardized coefficients are shown for all participants with depression allowed to correlate with all exogenous and endogenous variables in the model. * p < .05, ** p < .01, *** p < .001.
Keywords: Sleep problems, Childhood trauma, Impaired control, Alcohol use, Alcohol related problems
Highlights
-
•
Emotional abuse was directly linked to more insomnia.
-
•
Insomnia was directly related to more impaired control over drinking (IC).
-
•
Insomnia was directly related to more alcohol-related problems.
-
•
Insomnia and IC mediated the pathway from emotional abuse to alcohol use.
-
•
Insomnia and IC mediated the pathway from emotional abuse to alcohol-problems.
Abstract
Introduction
Hyperarousal theory states that stressful negative events can result in a physiological response in the body leading to poor sleep quality. Childhood trauma is associated with many negative health consequences persisting into adulthood such as insomnia. Insomnia itself is a driver of poor physical and psychological health including excessive alcohol use. We examined the direct and indirect relationships between trauma (i.e., physical-neglect, physical, emotional, and sexual abuse) as well as emotionally supportive families on insomnia, impaired control over drinking, alcohol use, and alcohol-related problems.
Methods
We studied a sample of 941 college students (467 women, 474 men). For our data analysis, we used a structural equation model with model indirect commands and 20,000 iteration bootstrapping with asymmetric confidence intervals in Mplus to obtain our mediated effects.
Results
Higher levels of emotional abuse were directly associated with more insomnia. Further, higher levels of physical neglect were directly associated with more impaired control over drinking. We found several mediational pathways from this investigation as well. Higher levels of emotional abuse were indirectly linked to both more alcohol use and alcohol-related problems through increased insomnia and impaired control over drinking.
Conclusions
Our results were consistent with Hyperarousability Theory. We suggest that insomnia may contribute to dysregulated drinking and that combating emotional abuse could be a promising therapeutic target of intervention among college student social drinkers.
1. Introduction
“A ruffled mind makes a restless pillow” – Charlotte Bronte
Hyperarousal Theory presumes experiencing trauma will result in a fight-or-flight response leading to poor sleep quality (Kalmbach et al., 2018; Riemann et al., 2010). Insomnia refects trouble falling asleep, trouble staying asleep, or waking too early (Punnoose, Golub, & Burke, 2012) and impacts between 10 and 30% of adults (Roth, 2007). Chronic insomnia can increase impaired mood, fatigue, difficulty thinking, and interfer with job performance (Punnoose et al., 2012); it is comorbid with general anxiety (Neckelmann, Mykletun, & Dahl, 2007), social anxiety (Blumenthal, Taylor, Cloutier, Baxley, & Lasslett, 2019), depression (Staner, 2010), post-traumatic stress disorder (PTSD; Lamarche & De Koninck, 2007), suicidal ideation (Zuromski, Cero, & Witte, 2017), as well as substance abuse (Roane & Taylor, 2008). Importantly, childhood maltreatment may drive the development of insomnia during adulthood (Bader, Schaefer, Schenkel, Nissen, & Schwander, 2007).
1.1. Dimensions of childhood trauma and insomnia
Childhood trauma negatively effects both psychological and physiological health and may be partially responsible for insomnia development (Bader et al., 2007). Insomnia following trauma may be due to hyperarousal; the heightened activation of the hypothalamic-pituitaryadrenal (HPA) axis and sympathetic nervous system (Otte et al., 2005, Vgontzas et al., 2001). Presumably, individuals who experienced a traumatic event show persistent alterations to neuroendocrine functioning consistent with hyperarousal (Otte et al., 2005). Traumatic events can precipitate psychophysiological symptoms and the sensation of hyperarousal (Schell, Marshall, & Jaycox, 2004) and have been positively associated with insomnia (Heir et al., 2010, Felmingham et al., 2012).
Hyperarousal following childhood trauma can result in psychophysiological changes persisting over time. Life events that trigger a state, such as the state of hyperarousal from a fight-or-flight response following a stressful event, can develop into a trait, or a stable aspect of one’s behavior or personality (Perry, Pollard, Blakley, Baker, & Vigilante, 1995). For instance, Blumenthal et al. (2019) found individuals higher on the trait of social anxiety are at higher risk for alcohol use disorder (AUD) when the mediating mechanism of insomnia is present. In this present investigation, we set out to determine if insomnia was directly linked to impaired control over drinking and if insomnia mediated the indirect links between distinct childhood trauma dimensions and drinking outcomes (i.e. impaired control, alcohol use, alcohol-related problems).
1.2. Trauma, insomnia, and alcohol use
Insomnia following a traumatic event is a risk factor for impaired attention, inhibition, and poor decision making, which may predispose one to making riskier choices involving alcohol (Fortier-Brochu and Morin, 2014, Anderson and Platten, 2011) as well as other substance use (Jenkins et al., 2015, Short et al., 2021). Greater insomnia and the resulting functional impairments (e.g., impaired decision-making, reduced inhibition) are associated with greater negative consequences of alcohol use (Goodhines et al., 2019). Further, greater sleep latency (the time between going to bed and sleep onset) and increased rapid eye movement sleep are significant predictors of relapse to alcohol use (Brower & Perron, 2010).
The comorbidity of insomnia and childhood maltreatment suggests the presence of mediating variables within the childhood trauma to alcohol-related problems pathway. For instance, insomnia is associated with greater impulsivity (Schmidt, Gay, & Van der Linden, 2008). Impaired control over drinking (IC) is considered impulsivity specific to the drinking context (Patock-Peckham et al., 2001, Patock-Peckham and Morgan-Lopez, 2006; Patock-Peckham & Morgan-Lopez, 2006; Patock-Peckham et al., 2011, Patock-Peckham et al., 2018; Patock-Peckham et al., 2020) and is a well-validated construct (Heather et al., 1998, Marsh et al., 2002, Sa’nchez et al., 2020). Impaired control over drinking (IC) is the inability to limit alcohol consumption despite a-priori intentions to limit drinking behavior (Heather, Tebbutt, Mattick, & Zamir, 1993, p.701).
1.3. Childhood trauma and gender
It is critical to determine the environmental factors underlying AUDs such as childhood trauma prior to age 12. The distinct facets of trauma and their definitions and what each dimension is related to is depicted in Table 1. Albeit, AUDs are increasing greatly among women in more recent times (Grant et al., 2017), men still generally consume more alcohol than women (Erol & Karpyak, 2015). Thus, we included cisgender (men, women) as a covariate in our model. As depression is commonly considered bi-directionally associated with both insomnia (Buysse et al., 2008; Fang et al., 2019) and AUDs (McHugh & Weiss, 2019) we also included depression as a covariate in our model.
Table 1.
Facets of Trauma.
| Physical Neglect | The failure to provide necessary care so as to seriously endanger the physical health of the child | “When I was growing up, I didn’t have enough to eat” |
| Constructs Associated with this Facet: domestic violence, single parent households, poverty, substance abuse, & negative academic outcomes (DiLauro, 2004; Brown, Cohen & Salinger, 1998; Connell-Carrick, 2003; Sedlack et al., 2010; Drake & Pandey, 1996; Taussig, 2002; Nikulina, Widom, & Czaja, 2011) | ||
| Emotional Abuse | Any act which may diminish the sense of identity, dignity, and self-worth. | “When I was growing up, people in my family called me things like “stupid”, “lazy”, or “ugly”.” |
| Constructs Associated with this Facet: dissociation, depression, irritability, lower self-esteem, marital dissatisfaction, anxiety, eating disorders, substance abuse, posttraumatic stress disorder, intimate partner violence (Perry et al., 2007; Briere & Runtz, 1990; Teicher et al., 2006; Briere & Runtz, 1988; Hyman et al., 2006; Witkiewitz & Dodge-Reyome, 2001; Schneider et al., 2007; Berzenski & Yates, 2010) | ||
| Sexual Abuse | Abusive sexual behavior by one person upon another. | “When I was growing up, someone tried to make me do sexual things or watch sexual things.” |
| Constructs Associated with this Facet: increased somatization, health problems, depression, posttraumatic stress disorder, dissociation, substance abuse, self-injury (Jacobsen & Herald, 1990; Goodman et al., 1997; Springs & Freidrich, 1992; Putnam, 2003; Polunsly & Follette, 1995; Fergusson et al., 2008; Neumann et al., 1996; Klonsky & Moyer, 2008; Gratz, 2003) | ||
| Physical Abuse | Any intentional act causing injury or trauma by way of bodily contact. | “When I was growing up, people in my family hit me so hard that it left me with bruises or marks” |
| Constructs Associated with this Facet: own-child abuse, household disorganization, depressive episodes (Ertem et al., 2000; Elmer, 1967; Kim & Cicchetti, 2006; Kazdin et al., 1985) | ||
| Emotional Support | The ability to show empathy, compassion, and genuine concern for another person. | “When I was growing up, I knew that there was someone to take care of and protect me. |
| Constructs Associated with this Facet: resiliency, better psychological adjustment, less posttraumatic stress disorder symptoms, less female depressive symptoms, less future depression in adolescent females, lower levels of illness, less health decline, less helplessness (Valentine & Feinauer, 1993; Collishaw et al., 2007; Testa et al., 1992; Hyman et al., 2003; Powers et al., 2009; Stice et al., 2004; Zhao et al., 2010; Merrick et al., 2013; Kendall-Tackett, 2002) | ||
1.4. Objectives and hypotheses
This investigation sought to examine the indirect relationship between childhood trauma on both alcohol use and alcohol-related problems with insomnia and impaired control serving as potential mediators. Based upon Hyperarousal Theory (Kalmbach et al., 2018; Riemann et al., 2010), we hypothesized that physical, sexual, and emotional abuse as well as physical neglect would be indirectly linked to alcohol-related problems through both insomnia and impaired control. We predicted that a supportive family would be indirectly linked to decreased alcohol-related problems through both lower levels of insomnia and IC.
2. Method
2.1. Participants
Participants included 941 university students (467 women, 474 men) who were awarded course credit and the protocol was approved by the IRB. This sample was 56% male, with an average age of 20.41 years (SD = 3.27) and was 66% Caucasian, 14% Hispanic, 10% Asian, and 4% African American, and 6% reported “other” race/ethnicity.
2.2. Measures
2.2.1. The childhood trauma questionnaire
(CTQ; Bernstein et al., 2003) consists of 25-items, measuring physical neglect, emotional, physical, and sexual abuse as well as an emotionally supportive family retrospectively from childhood prior to age 12. Emotional abuse consists of 5-items including, “People in my family said hurtful or insulting things to me.” Physical abuse consists of 5-items including, “People in my family hit me so hard it left me with bruises or marks.” Sexual abuse consists of 5 items including, “Someone tried to touch me in a sexual way or tried to make me touch them.” Physical neglect consists of 5-items including, “I didn’t have enough to eat.” Emotionally supportive family members consisted of 8-items including, “I knew there was someone to take care of me and protect me.” The α reliabilities were physical neglect 0.71, emotional 0.84, physical 84, and sexual abuse as well as an emotionally supportive family 0.91.
2.2.2. The athens insomnia scale
(Soldatos, Dikeos, and Paparrigopoulous (2000)) is an 8 item scale measuring difficulty falling asleep, awakening during the night, awakening early in the morning, total sleep duration, and quality of sleep. Sample items include “sleep induction (time it takes you to fall asleep from turning-off the lights)”, “awakenings during the night“, and “sleepiness during the day.” The α reliability for this sample was 0.89.
2.2.3. Impaired control part III
Scale reflects 10-items from (Heather et al., 1993). Higher scores on this measure are reflective of a lack of perceived control over drinking (i.e., an inability to stop drinking at will). A sample item included, “Even if I intended having only one or two drinks, I would end up having many more.” The α reliability was 0.84.
2.2.4. Alcohol use (Quantity/Frequency Measure)
The quantity and frequency items were combined into a single Quantity/Frequency Scale by converting the frequency scales into equivalent occasions per month, which ranged from 1 = 0.5 times per month to 7 = 28 times per month, and the quantity levels into equivalent grams of alcohol, which ranged from 1 = 10 g per month to 5 = 70 g per month. These values were multiplied and the distribution of scores were transformed through a log10 transformation (Wood, Nagoshi, & Dennis, 1992).
2.2.5. Alcohol-related problems. Young adult alcohol problems screening test
(YAAPST) is a 27-item questionnaire that measures the negative consequences of alcohol use in college students (Hurlbut & Sher, 1992). This scale assesses current and lifetime alcohol-related issues. A sample item included, “Have you ever neglected your obligations, your family, your work, or school-work for two or more days in a row because of your drinking?” The α reliability was 0.83.
2.3. Statistical approach
A structural equation model was fit using Mplus v7.2 (Muthén & Muthén, 1998–2013). Fig. 1 displays the conceptual model with all hypothesized direct pathways. Model fit was determined by examining the Comparative Fit Index (CFI; Bentler, 1990) and Root Mean Square Error of Approximation (RMSEA; Browne and Cudeck, 1993, Hu and Bentler, 1998), as well as chi-square statistics. Mediation analyses were examined to investigate indirect influences of childhood trauma facets on drinking outcomes (i.e. IC, alcohol use, and alcohol-related problems) through the mediating mechanism of increased insomnia. Bootstrapping (K = 20,000) was used to examine indirect effects (Efron & Tibshirani, 1993) by using the model indirect command in Mplus; 95% confidence intervals around the estimates were also examined (Hancock and Liu, 2012, MacKinnon, 2008, Taylor et al., 2008).
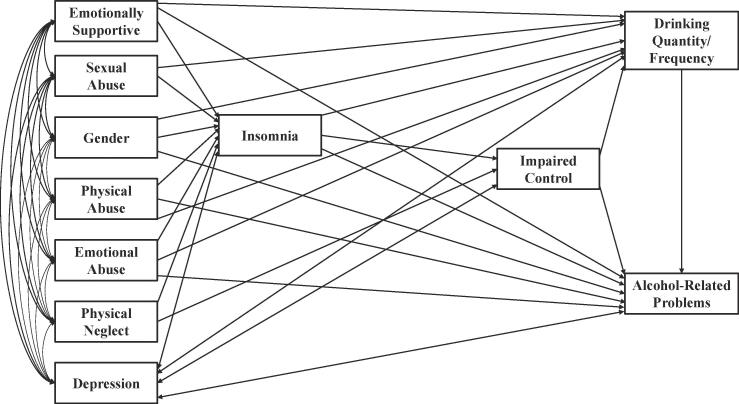
Fig. 1.
Conceptual model of all examined paths among the exogenous and endogenous variables in the model. Depression was allowed to correlate with all variables in the model, which is depicted with two-way arrows. Gender was allowed to correlate with all the exogenous variables in the model and serve as a predictor for all endogenous variables.
3. Results
3.1. Overall model fit
Descriptive statistics can be found on Table 1. All hypothesized paths were modeled in Fig. 1 and significant paths were modeled in Fig. 2. The model yielded a χ2 (8df) = 12.806, p = .1187; RMSEA = 0.025, 90% CI (0.000, 0.050); probability RMSEA < = 0.05 = 0.951; CFI = 0.996; TLI = 0.980. Table 2 depicts the means, standard deviations, and correlations among all variables in our model.
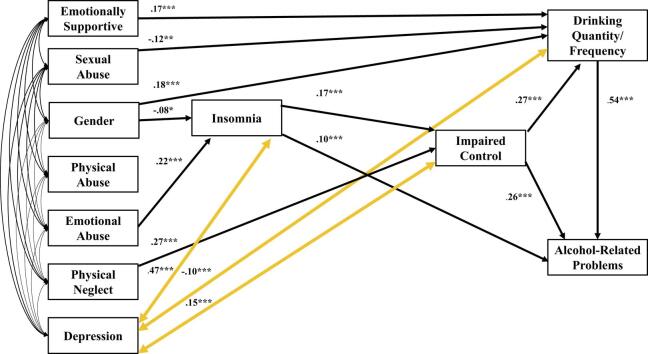
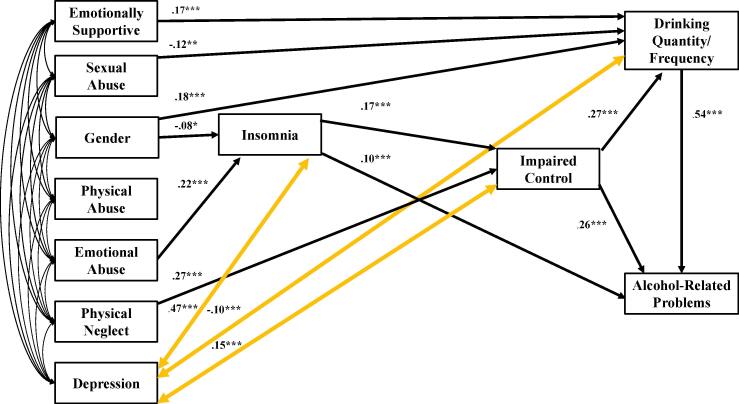
Fig. 2.
Fit Model in which standardized coefficients are shown. All exogenous variables were allowed to correlate freely in the model. In addition, we added gender and depression as a covariate. Note - *p < .05, ** p < .01, ***p < .001. N = 941; χ2 (6df) = 14.727, p = 0.0225; CFI = 0.989; RMSEA = 0.039; 90% CI (0.014, 0.065).
Table 2.
Means, standard deviations, and correlations among all variables.
| M | SD | Measures | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3.77 | 0.92 | 1. Emotionally Supportive Family | 1.00 | ||||||||||
| 1.35 | 0.80 | 2. Sexual Abuse | 0.16 | 1.00 | |||||||||
| 0.50 | 0.49 | 3. Gender | −0.08 | 0.03 | 1.00 | ||||||||
| 1.49 | 0.74 | 4. Physical Abuse | −0.41 | 0.50 | 0.13 | 1.00 | |||||||
| 1.73 | 0.83 | 5. Emotional Abuse | −0.59 | 0.45 | −0.05 | 0.58 | 1.00 | ||||||
| 1.48 | 0.67 | 6. Physical Neglect | −0.61 | 0.48 | 0.10 | 0.50 | 0.44 | 1.00 | |||||
| 35.52 | 10.92 | 7. Depression | −0.31 | 0.21 | −0.14 | 0.19 | 0.33 | 0.24 | 1.00 | ||||
| 6.96 | 4.54 | 8. Insomnia | −0.21 | 0.10 | −0.09 | 0.09 | 0.25 | 0.14 | 0.56 | 1.00 | |||
| 1.87 | 0.74 | 9. Impaired Cntrol | −0.20 | 0.16 | 0.08 | 0.16 | 0.12 | 0.29 | 0.30 | 0.21 | 1.00 | ||
| 1.90 | 0.67 | 10. Alcohol Use (drinking) q/f | 0.11 | −0.12 | 0.18 | −0.08 | −0.08 | −0.08 | −0.10 | 0.01 | 0.23 | 1.00 | |
| 0.60 | 0.58 | 11. Alcohol Related Problems | −0.01 | 0.03 | 0.14 | 0.06 | 0.07 | 0.03 | 0.09 | 0.16 | 0.41 | 0.61 | 1.00 |
3.2. Standardized direct effects
Being male was directly associated with experiencing more physical-neglect (β = 0.103, s.e. = 0.034; Z = 3.064, p = .002) as well as experiencing more physical-abuse (β = 0.126, s.e. = 0.033; Z = 3.770, p < .001) before the age of 12. In addition, being male was directly related to less insomnia ((β = −0.077, s.e. = 0.033; Z = -2.357, p = .018), albeit more alcohol use at 20 years of age (β = 0.184, s.e. = 0.032; Z = 5.749, p < .001). Being female was associated with a less emotionally supportive family (β = -0.077, s.e. = 0.034; Z = -2.281, p = .023).
Emotional-abuse was directly linked to more insomnia, (β = 0.224, s.e. = 0.048; Z = 4.701, p < .001). Both physical neglect (β = 0.267, s.e. = 0.035; Z = 7.559; p < .001) and insomnia (β = 0.171, s.e. = 0.034; Z = 5.057; p < .001) were directly linked to more IC.
Interestingly, an emotionally supportive family (β = 0.170, s.e. = 0.045; Z = 3.822, p < .001), as well as an emotionally abusive one at a trend level (β = 0.091, s.e. = 0.047; Z = 1.951, p = .051), were both directly linked to more alcohol use. Sexual abuse was directly linked to less alcohol use (β = -0.121, s.e. = 0.043; Z = -2.851, p = .004). Furthermore, higher levels of IC were directly linked to more alcohol use (β = 0.268, s.e. = 0.035; Z = 7.769, p < .001).
Emotional-abuse was directly linked to more alcohol-related problems at a trend level (β = 0.075, s.e. = 0.039; Z = 1.950, p = .051). In addition, higher levels of insomnia symptoms (β = 0.099, s.e. = 0.030; Z = 3.315, p = .001) impaired control (β = 0.258, s.e. = 0.032; Z = 8.131; p < .001) and alcohol use (β = 0.542, s.e. = 0.027; Z = 20.072, p < .001) were directly linked to more alcohol-related problems.
3.3 Table 3 depicts all the two and three path mediated effects. We used 95% confidence intervals for all indirect effects.
Table 3.
Mediated pathways.
| Pathway Effects | Indirect Effect | S.E. | Z-Score | P-Value | 95% Cl |
|---|---|---|---|---|---|
| Impaired Control (IC) | |||||
| Emotional abuse → Insomnia → IC | 0.034 | 0.010 | 3.317 | p < .001 | (0.017, 0.058) |
| Supportive Family → Insomnia → IC | -0.012 | 0.007 | −1.752 | p = .080 | (−0.029, 0.000)* |
| Gender → Insomnia → IC | −0.019 | 0.008 | −2,225 | p = .026 | (−0.038, −0.005) |
| Alcohol Use | |||||
| Insomnia → IC → Alcohol Use | 0.007 | 0.002 | 4.005 | p < .001 | (0.004, 0.010) |
| Emotional abuse → Insomnia → IC → Alcohol Use | 0.008 | 0.003 | 3.036 | p = .002 | (0.004, 0.015) |
| Gender → Insomnia → IC → Alcohol Use | −0.005 | 0.002 | −2.124 | p = .034 | (−0.010, −0.001) |
| Alcohol-Related Problems (ARP) | |||||
| Insomnia → IC → ARP | 0.006 | 0.001 | 3.888 | p < .001 | (0.003, 0.009) |
| Insomnia → IC → Alcohol Use → ARP | 0.003 | 0.001 | 3.860 | p < .001 | (0.002, 0.005) |
| Supportive Family → Insomnia – ARP | 0.058 | 0.016 | 3.728 | p < .001 | (0.028, 0.089) |
| Sexual abuse → Alcohol Use → ARP | −0.048 | 0.018 | −2.724 | p = .006 | (−0.084, −0.015) |
| Emotional abuse → Insomnia → IC → ARP | 0.007 | 0.002 | 2.969 | p = .003 | (0.003, 0.013) |
| Emotional abuse → Insomnia → IC → Alcohol Use → ARP | 0.004 | 0.001 | 2.947 | p = .003 | (0.002, 0.007) |
| Physical Neglect → IC → ARP | 0.058 | 0.010 | 5.954 | p < .001 | (0.041, 0.079) |
| Physical Neglect → IC → Alcohol Use → ARP | 0.033 | 0.006 | 5.244 | p < .001 | (0.022, 0.047) |
| Gender → Insomnia → IC → ARP | −0.004 | 0.002 | −2.103 | p = .035 | (−0.008, −0.001) |
| Gender → Insomnia → IC → Alcohol Use → ARP | −0.002 | 0.001 | −2.100 | p = .036 | (−0.005, −0.001) |
Note – IC = Impaired Control; ARP = Alcohol-Related Problems; Gender = 1 for Cisgender men and 0 for Cisgender women; * = no evidence of mediation as zero shows up in the interval.
4. Discussion
Hyperarousal theory presumes experiencing trauma will result in a chronic fight-or-flight reaction following a threat leading to negative health consequences such as insomnia (Riemann et al., 2010). In the extant literature, hyperarousability is associated with greater AUD in those suffering from PTSD, as well as increased rates of relapse (Dworkin et al., 2018, Livingston et al., 2020). Consistent with this theory, we found that those who experienced trauma via emotional abuse during childhood were significantly more likely to experience insomnia, and in turn, consume greater amounts of alcohol in emerging adulthood. We found childhood emotional abuse may indirectly increase AUDs through increased insomnia and impaired control. Emotional abuse has historically received less attention than other forms of child maltreatment, albeit recent literature suggests that it may be the most psychologically harmful (Dias et al., 2015, Teicher et al., 2006). Childhood emotional abuse predicts later psychological disorders through greater emotional dysregulation (Burns, Jackson, & Harding, 2010). Hyperarousal based insomnia is often a consequence of sustained emotional distress (Wassing et al., 2016), therefore emotional abuse may induce hyperarousal insomnia to a greater extent than other childhood maltreatment types. Insomnia mediated the pathway between childhood abuse and impaired control, which is a novel finding. Our model provides a novel conception of insomnia’s predictive capacity for impaired control over drinking. Schmidt et al. (2008) established the link between sleep deprivation and impulsivity. As impulsivity is significantly related to impaired control (Patock-Peckham and Morgan-Lopez, 2006, Patock-Peckham et al., 2011, Patock-Peckham et al., 2018; 2020), we extend this literature by showing how impaired control could be a more specific mechanism by which dysregulated alcohol consumption may occur in conjunction with insomnia. Presumably, people who have insomnia may not be able to stick with their original intentions to limit their own drinking.
Our study replicated the indirect association between emotional abuse and alcohol related problems (Schwandt et al., 2013, Patock-Peckham et al., 2020) and extended upon the developmental pathway by including insomnia and IC as mediators. As hypothesized, increased insomnia, impaired control, and in turn, alcohol use were directly linked to greater alcohol-related problems. The link between greater impaired control and more alcohol related problems is consistent with the literature (Frohe et al., 2020, Patock-Peckham et al., 2001, Patock-Peckham and Morgan-Lopez, 2006; 2011; 2018; 2020; Leeman, Patock-Peckham, & Potenza, 2012). This is important because it shows that poor sleep may lead to ignoring one’s own intentions to limit alcohol consumption.
Physical abuse was not significantly associated with insomnia in our college student sample. This is consistent with Boden, Horwood, and Fergusson (2007) who found that college students were less prone to experiencing physical abuse than the general population. Nevertheless, our finding was inconsistent with Anne Lown, Nayak, Korcha, and Greenfield (2011), who found that women who experienced childhood physical abuse were at a greater risk of alcohol use and related consequences than women who did not experience such abuse. Similarly, Rehan, Antfolk, Johansson, Jern, and Santtila (2017) found that, for both sexes, childhood physical abuse was associated with alcohol abuse. Thus, this finding requires replication in other college samples as it is possible that our rates of physical abuse are lower than the general population.
We hypothesized that having an emotionally supportive family would be associated with fewer alcohol-related-problems through lower levels of insomnia and IC. Yet, we found that an emotionally supportive family was directly linked to greater alcohol use. This finding may speak to the differences between drinking motives, such as social motives for drinking (Cooper, Russell, Skinner, & Windle, 1992) which are normative in a college student sample. While individuals with a history of childhood trauma may drink to cope with negative feelings (Jester, Steinberg, Heitzeg, & Zucker, 2015), which is consistent with the Self-Medication Theory (Conger, 1956, Hersh and Hussong, 2009), people without a history of trauma may have other drinking motives such as social motives. Given that our sample was comprised of college students, some individuals in this population may drink to conform to college drinking culture or to bond with their peers.
Physical neglect was linked to having greater impaired control over alcohol use, but not through insomnia as we hypothesized. The link between childhood physical neglect to IC is consistent with recent literature (Frohe et al., 2020, Patock-Peckham et al., 2020). The fact that individuals who experienced physical neglect do not develop insomnia may be due to differences in the psychophysiological consequences across trauma subtypes. The more directed nature of emotional abuse may induce a stress response that results in hyperarousal. Conceivably, emotionally abused individuals might ruminate over their untoward conversations more while trying to settle down and sleep. Consistent with the Theory of Behavioral Economics (Vuchinich & Heather, 2003), physical neglect may directly result in behavioral under-control. Because physically neglected children are deprived of basic reinforcers, when allowed open access in adulthood, they may have difficulty self-imposing limits. Because IC is the inability to adhere to self-imposed limits over alcohol consumption (Heather et al., 1993), childhood physical neglect may be directly associated with IC.
5. Sex differences
In our study, men were significantly more likely than women to experience physical neglect and physical abuse during their childhood, as well as to consume more alcohol in college. Moreover, in our study, women were significantly more likely than men to have a less emotionally supportive family. This was somewhat inconsistent with other studies examining other facets of abuse and care. For instance, Widom, Marmorstein, and Raskin White (2006) showed that women who experienced physical neglect were more likely than men to frequently consume large quantities of alcohol in young and middle adulthood. Further, Rehan et al. (2017) found that there were no sex differences in experiencing physical neglect or physical abuse, but women were statistically more likely than men to experience severe emotional abuse, emotional neglect, and sexual abuse.
6. Limitations
Although we are consistent with the literature showing a relationship between trauma and insomnia, we are lacking measurement of biomarkers of hyperarousal such as HPA axis elevation, hormone concentrations, sympathetic nervous system activation, through EEG, fMRI, or HRV. Future studies should collect biomarkers to better support the theory that childhood trauma results in insomnia because of hyperarousal. Second, our study used a college population, which is generally less likely to experience as many severe forms of physical abuses than a more general population (Tanaka, Georgiades, Boyle, & MacMillan, 2015). Moreover, while insomnia is often considered a consequence of heavy alcohol use or alcohol withdrawal, the relationship may be bidirectional (Chakravorty, Chaudhary, & Brower, 2016). Consider our model to be an exploratory look from just one direction from the insomnia to alcohol use and related problems pathways with a social drinking college sample only; these findings should be re-examined longitudinally.
7. Conclusion
Our study is the first demonstrating the mediating relationship between childhood trauma, insomnia, impaired control, and alcohol use and related problems. Our study is novel and extends the current literature in showing that emotional abuse suffered during childhood may precipitate alcohol abuse during adulthood, and that this relationship is indirectly mediated by insomnia and impaired control over alcohol use. The combination of childhood trauma and insomnia can create a perfect storm of risk factors that predispose one to alcohol abuse (Agorastos et al., 2019, Soehner and Harvey, 2012). Chronic fatigue and the negative health consequences of sleep deprivation stemming from insomnia can disrupt one’s ability to make responsible choices with alcohol, thus increasing the risk for negative consequences of alcohol use and related problems. The findings from this study demonstrate the importance of further research on how emotionally induced trauma relates to insomnia and to impaired control over drinking. This pathway is a novel therapeutic target in our quest to combat the development of AUDs.
Funding
NIH/NIAAA [Grant number K01AA02416001A1] to Julie A. Patock-Peckham and the Burton Family Foundation [Grant number FP11815] to the Social Addictions Impulse Lab supported this work.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Agorastos A., Pervanidou P., Chrousos G.P., Baker D.G. Developmental trajectories of early life stress and trauma: A narrative review on neurobiological aspects beyond stress system dysregulation. Frontiers in Psychiatry. 2019;10:118. doi: 10.3389/fpsyt.2019.00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson C., Platten C.R. Sleep deprivation lowers inhibition and enhances impulsivity to negative stimuli. Behavioural Brain Research. 2011;217(2):463–466. doi: 10.1016/j.bbr.2010.09.020. [DOI] [PubMed] [Google Scholar]
- Anne Lown E., Nayak M.B., Korcha R.A., Greenfield T.K. Child physical and sexual abuse: A comprehensive look at alcohol consumption patterns, consequences, and dependence from the National Alcohol Survey. Alcoholism: Clinical and Experimental Research. 2011;35(2):317–325. doi: 10.1111/j.1530-0277.2010.01347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bader K., Schaefer V., Schenkel M., Nissen L., Schwander J. Adverse childhood experiences associated with sleep in primary insomnia. Journal of Sleep Research. 2007;16(3):285–296. doi: 10.1111/j.1365-2869.2007.00608.x. [DOI] [PubMed] [Google Scholar]
- Bentler P.M. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bernstein D.P., Stein J.A., Newcomb M.D., Walker E., Pogge D., Ahluvalia T., Stokes J., Handelsman L., Medrano M., Desmond D., Zule W. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Blumenthal, H., Taylor, D.J., Cloutier, R.M., Baxley, C., Lasslett, H. (2019). The Links Between Social Anxiety Disorder, Insomnia Symptoms, and Alcohol Use Disorders: Findings From a Large Sample of Adolescents in the United States, Behavior Therapy, 50(1), 50-59. https://doi.org/10.1016/j.beth.2018.03.010. [DOI] [PubMed]
- Boden J.M., Horwood L.J., Fergusson D.M. Exposure to childhood sexual and physical abuse and subsequent educational achievement outcomes. Child Abuse & Neglect. 2007;31(10):1101–1114. doi: 10.1016/j.chiabu.2007.03.022. [DOI] [PubMed] [Google Scholar]
- Brower K.J., Perron B.E. Sleep disturbance as a universal risk factor for relapse in addictions to psychoactive substances. Medical Hypotheses. 2010;74(5):928–933. doi: 10.1016/j.mehy.2009.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne M.W., Cudeck R. In: Testing structural equation models. Bollen K.A., Lond J.S., editors. Sage; Newbury Park, CA: 1993. Alternative ways of assessing model fit; pp. 136–162. [Google Scholar]
- Burns E.E., Jackson J.L., Harding H.G. Child maltreatment, emotion regulation, and posttraumatic stress: The impact of emotional abuse. Journal of Aggression, Maltreatment & Trauma. 2010;19(8):801–819. [Google Scholar]
- Buysse D.J., Angst J., Gamma A., Ajdacic V., Eich D., Rossier W. Prevalence, Course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31(4):473–480. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger J.J. Alcoholism: Theory, problem and challenge. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956;13:296–305. [PubMed] [Google Scholar]
- Cooper M.L., Russell M., Skinner J.B., Windle M. Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment. 1992;4(2):123. [Google Scholar]
- Chakravorty S., Chaudhary N.S., Brower K.J. Alcohol dependence and its relationship with insomnia and other sleep disorders. Alcoholism: Clinical and Experimental Research. 2016;40(11):2271–2282. doi: 10.1111/acer.13217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dias A., Sales L., Hessen D.J., Kleber R.J. Child maltreatment and psychological symptoms in a Portuguese adult community sample: The harmful effects of emotional abuse. European Child & Adolescent Psychiatry. 2015;24(7):767–778. doi: 10.1007/s00787-014-0621-0. [DOI] [PubMed] [Google Scholar]
- Dworkin E.R., Wanklyn S., Stasiewicz P.R., Coffey S.F. PTSD symptom presentation among people with alcohol and drug use disorders: Comparisons by substance of abuse. Addictive Behaviors. 2018;76:188–194. doi: 10.1016/j.addbeh.2017.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efron B., Tibshirani T.J. Chapman & Hall; New York: 1993. An introduction to the bootstrap. [Google Scholar]
- Erol A., Karpyak V.M. Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug and Alcohol Dependence. 2015;156:1–13. doi: 10.1016/j.drugalcdep.2015.08.023. [DOI] [PubMed] [Google Scholar]
- Felmingham K.L., Rennie C., Gordon E., Bryant R.A. Autonomic and cortical reactivity in acute and chronic posttraumatic stress. Biological Psychology. 2012;90(3):224–227. doi: 10.1016/j.biopsycho.2012.03.011. [DOI] [PubMed] [Google Scholar]
- Fortier-Brochu É., Morin C.M. Cognitive impairment in individuals with insomnia: Clinical significance and correlates. Sleep. 2014;37(11):1787–1798. doi: 10.5665/sleep.4172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frohe T., Leeman R.F., Cheong J., Belton D.A., Patock-Peckham J.A. Novel associations among trauma, mindfulness, and impaired control over alcohol use. Mindfulness. 2020;11(3):606–614. doi: 10.1007/s12671-019-01285-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodhines P.A., Gellis L.A., Kim J., Fucito L.M., Park A. Self-medication for sleep in college students: Concurrent and prospective associations with sleep and alcohol behavior. Behavioral Sleep Medicine. 2019;17(3):327–341. doi: 10.1080/15402002.2017.1357119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B.F., Chou S.P., Saha T.D., Pickering R.P., Kerridge B.T., Ruan W.J., Huang B., Jung J., Zhang H., Fan A., Hasin D.S. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001–2002 to 2012–2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911–923. doi: 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hancock G.R., Liu M. Bootstrapping standard errors and data-model fit statistics in structural equation modeling. Handbook of Structural Equation Modeling. 2012:296–306. [Google Scholar]
- Heather N., Booth P., Luce A. Impaired Control Scale: cross-validation and relationships with treatment outcome. Addiction. 1998;93(5):761–771. doi: 10.1046/j.1360-0443.1998.93576112.x. [DOI] [PubMed] [Google Scholar]
- Heather N., Tebbutt J.S., Mattick R.P., Zamir M. Development of a scale for measuring impaired control over alcohol consumption: A preliminary report. Journal of Studies on Alcohol. 1993;54(6):700–709. doi: 10.15288/jsa.1993.54.700. [DOI] [PubMed] [Google Scholar]
- Heir T., Piatigorsky A., Weisæth L. Posttraumatic stress symptom clusters associations with psychopathology and functional impairment. Journal of Anxiety Disorders. 2010;24(8):936–940. doi: 10.1016/j.janxdis.2010.06.020. [DOI] [PubMed] [Google Scholar]
- Hersh M.A., Hussong A.M. The association between observed parental emotion socialization and adolescent self-medication. Journal of Abnormal Child Psychology. 2009;37(4):493–506. doi: 10.1007/s10802-008-9291-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L., Bentler P.M. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3(4):424–453. doi: 10.1037/1082-989X.3.4.424. [DOI] [Google Scholar]
- Hurlbut S.C., Sher K.J. Assessing alcohol problems in college students. Journal of American College Health. 1992;41(2):49–58. doi: 10.1080/07448481.1992.10392818. [DOI] [PubMed] [Google Scholar]
- Jenkins M.M., Colvonen P.J., Norman S.B., Afari N., Allard C.B., Drummond S.P. Prevalence and mental health correlates of insomnia in first-encounter veterans with and without military sexual trauma. Sleep. 2015;38(10):1547–1554. doi: 10.5665/sleep.5044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jester, J. M., Steinberg, D. B., Heitzeg, M. M., & Zucker, R. A. (2015). Coping expectancies, not enhancement expectancies, mediate trauma experience effects on problem alcohol use: A. [DOI] [PMC free article] [PubMed]
- Kalmbach D.A., Cuamatzi-Castelan A.S., Tonnu C.V., Tran K.M., Anderson J.R., Roth T., Drake C.L. Hyperarousal and sleep reactivity in insomnia: Current insights. Nature and Science of Sleep. 2018;10:193–201. doi: 10.2147/NSS.S138823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamarche L.J., De Koninck J. Sleep disturbance in adults with posttraumatic stress disorder: A review. The Journal of Clinical Psychiatry. 2007;68(8):1257–1270. doi: 10.4088/jcp.v68n0813. [DOI] [PubMed] [Google Scholar]
- Leeman R.F., Patock-Peckham J.A., Potenza M.N. Impaired control over alcohol use: An under-addressed risk factor for problem drinking in young adults? Experimental and Clinical Psychopharmacology. 2012;20(2):92. doi: 10.1037/a0026463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston N.A., Mahoney C.T., Ameral V., Brief D., Rubin A., Enggasser J.…Keane T. Changes in alcohol use, PTSD hyperarousal symptoms, and intervention dropout following veterans’ use of VetChange. Addictive behaviors. 2020;107:106401. doi: 10.1016/j.addbeh.2020.106401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon D.P. Taylor & Francis Group/Lawrence Erlbaum Associates, New York, NY; New York, NY: 2008. Introduction to statistical mediation analysis. [Google Scholar]
- Marsh A., Smith L., Saunders B., Piek J. The impaired control scale: confirmation of factor structure and psychometric properties for social drinkers and drinkers in alcohol treatment. Addiction. 2002;97:1339–1346. doi: 10.1046/j.1360-0443.2002.00190.x. [DOI] [PubMed] [Google Scholar]
- McHugh R.K., Weiss R.D. Alcohol use disorder and depressive disorders. Alcohol Research Current Reviews. 2019;40(1):1–8. doi: 10.35946/arcr.v40.1.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L.K., & Muthén, B.O. (1998-2013). Mplus user's guide (6th ed.). Los Angeles, CA: Author.
- Neckelmann D., Mykletun A., Dahl A.A. Chronic insomnia as a risk factor for developing anxiety and depression. 2007;30)7:873–880. doi: 10.1093/sleep/30.7.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otte, C., Lenoci, M., Metzler, T., Yehuda, R., Marmar, C. R., & Neylan, T. C. (2005). Hypothalamic–pituitary–adrenal axis activity and sleep in posttraumatic stress disorder. Neuropsychopharmacology, 30(6), 1173-1180. [DOI] [PubMed]
- Patock-Peckham J.A., Morgan-Lopez A.A. College drinking behaviors: Mediational link between parenting styles, impulse control, and alcohol-related outcomes. Psychology of Addictive Behaviors. 2006;20(2):117–125. doi: 10.1037/0893-164X.20.2.117. [DOI] [PubMed] [Google Scholar]
- Patock-Peckham J.A., Belton D.A., D'Ardenne K., Tein J.Y., Bauman D.C., Infurna F.J., McClure S.M. Dimensions of childhood trauma and their direct and indirect links to PTSD, impaired control over drinking, and alcohol-related-problems. Addictive Behaviors Reports. 2020;12:100304. doi: 10.1016/j.abrep.2020.100304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patock-Peckham J.A., Canning J.R., Leeman R.F. (2018). Shame is bad and guilt is good: An examination of the impaired control over drinking pathway to alcohol use and related problems. Personality and Individual Differences, 121, 62-66. doi: 10.1016/j.paid.2017.09.023. [DOI] [PMC free article] [PubMed]
- Patock-Peckham J.A., Cheong J., Balhorn M.E., Nagoshi C.T. A social learning perspective: A model of parenting styles, self-regulation, perceived drinking control, and alcohol use and problems. Alcoholism: Clinical & Experimental Research. 2001;25)9:1284–1292. [PubMed] [Google Scholar]
- Patock-Peckham J.A., King K.M., Morgan-Lopez A.A., Ulloa E.C., Filson Moses J.M. Gender-specific mediational links between parenting styles, parental monitoring, impulsiveness, drinking control, and alcohol-related problems. Journal of Studies on Alcohol and Drugs. 2011;72(2):247–258. doi: 10.15288/jsad.2011.72.247. [DOI] [PubMed] [Google Scholar]
- Perry B.D., Pollard R.A., Blakley T.L., Baker W.L., Vigilante D. Childhood trauma, the neurobiology of adaptation, and “use-dependent” development of the brain: How “states” become “traits”. Infant mental health journal. 1995;16(4):271–291. [Google Scholar]
- Punnoose A.R., Golub R.M., Burke A.E. Insomnia. The. Journal of the American Medical Association. 2012;307)24:2653. doi: 10.1001/jama.2012.6219. [DOI] [PubMed] [Google Scholar]
- Rehan W., Antfolk J., Johansson A., Jern P., Santtila P. Experiences of severe childhood maltreatment, depression, anxiety and alcohol abuse among adults in Finland. PLoS ONE. 2017;12(5):e0177252. doi: 10.1371/journal.pone.0177252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riemann D., Spiegelhalder K., Feige B., Voderholzer U., Berger M., Perlis M., Nissen C. The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Medicine Reviews. 2010;14(1):19–31. doi: 10.1016/j.smrv.2009.04.002. [DOI] [PubMed] [Google Scholar]
- Roane B.M., Taylor D.J. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31(10):1351–1356. [PMC free article] [PubMed] [Google Scholar]
- Roth T. Insomnia: Definition, Prevalence, Etiology, and Consequences. Journal of Clinical Sleep Medicine. 2007;3(5):S7–S10. [PMC free article] [PubMed] [Google Scholar]
- Sa’nchez E., Cruz Fuentez C., Benjet C., Medina-Mora M.E. Impaired control in heavy drinking and its association with alcohol craving and alcohol use severity. Salud Mental. 2020;43(4) doi: 10.17711/sSM0185-3325.2020.021. [DOI] [Google Scholar]
- Schell T.L., Marshall G.N., Jaycox L.H. All symptoms are not created equal: The prominent role of hyperarousal in the natural course of posttraumatic psychological distress. Journal of Abnormal Psychology. 2004;113(2):189. doi: 10.1037/0021-843X.113.2.189. [DOI] [PubMed] [Google Scholar]
- Schmidt R.E., Gay P., Van der Linden M. Facets of Impulsivity are differentially linked to insomnia: Evidence from an exploratory study. Behavioral Sleep Medicine. 2008;6(3):178–192. doi: 10.1080/15402000802162570. [DOI] [PubMed] [Google Scholar]
- Schwandt M.L., Heilig M., Hommer D.W., George D.T., Ramchandani V.A. Childhood trauma exposure and alcohol dependence severity in adulthood: Mediation by emotional abuse severity and neuroticism. Alcoholism: Clinical and Experimental Research. 2013;37(6):984–992. doi: 10.1111/acer.12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short N.A., Zvolensky M.J., Schmidt N.B. A pilot randomized clinical trial of Brief Behavioral Treatment for insomnia to reduce problematic cannabis use among trauma-exposed young adults. Journal of Substance Abuse Treatment. 2021 doi: 10.1016/j.jsat.2021.108537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soehner A.M., Harvey A.G. Prevalence and functional consequences of severe insomnia symptoms in mood and anxiety disorders: Results from a nationally representative sample. Sleep. 2012;35(10):1367–1375. doi: 10.5665/sleep.2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soldatos C.R., Dikeos D.G., Paparrigopoulous T.J. Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. Journal of Psychosomatic Research. 2000;48(6):555–560. doi: 10.1016/s0022-3999(00)00095-7. [DOI] [PubMed] [Google Scholar]
- Staner L. Comorbidity of insomnia and depression. Sleep Medicine Review. 2010;14:35–46. doi: 10.1016/j.smrv.2009.09.003. [DOI] [PubMed] [Google Scholar]
- Tanaka M., Georgiades K., Boyle M.H., MacMillan H.L. Child maltreatment and educational attainment in young adulthood: Results from the Ontario Child Health Study. Journal of Interpersonal Violence. 2015;30(2):195–214. doi: 10.1177/0886260514533153. [DOI] [PubMed] [Google Scholar]
- Taylor A.B., MacKinnon D.P., Tein J. Tests of the three-path mediated effect. Organizational Research Methods. 2008;11(2):241–269. doi: 10.1177/1094428107300344. [DOI] [Google Scholar]
- Teicher M.H., Samson J.A., Polcari A., McGreenery C.E. Sticks, stones, and hurtful words: Relative effects of various forms of childhood maltreatment. American Journal of Psychiatry. 2006;163(6):993–1000. doi: 10.1176/ajp.2006.163.6.993. [DOI] [PubMed] [Google Scholar]
- Vgontzas A.N., Bixler E.O., Lin H.M., Prolo P., Mastorakos G., Vela-Bueno A.…Chrousos G.P. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: Clinical implications. The Journal of Clinical Endocrinology & Metabolism. 2001;86(8):3787–3794. doi: 10.1210/jcem.86.8.7778. [DOI] [PubMed] [Google Scholar]
- Vuchinich R.E., Heather N., editors. Choice, behavioral economics and addiction. Elsevier; 2003. [Google Scholar]
- Wassing R., Benjamins J.S., Dekker K., Moens S., Spiegelhalder K., Feige B.…Van Someren E.J. Slow dissolving of emotional distress contributes to hyperarousal. Proceedings of the National Academy of Sciences. 2016;113(9):2538–2543. doi: 10.1073/pnas.1522520113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom C.S., Marmorstein N.R., Raskin White H. Childhood victimization and illicit drug use in middle adulthood. Psychology of Addictive Behaviors. 2006;20(4):394. doi: 10.1037/0893-164X.20.4.394. [DOI] [PubMed] [Google Scholar]
- Wood M.D., Nagoshi C.T., Dennis D.A. Alcohol norms and expectations as predictors of alcohol use and problems in a college student sample. The American Journal of Drug and Alcohol Abuse. 1992;18(4):461–476. doi: 10.3109/00952999209051042. [DOI] [PubMed] [Google Scholar]
- Zuromski K.L., Cero I., Witte T.K. Insomnia symptoms drive changes in suicide ideation: A latent difference score model of community adults over a brief interval. Journal of Abnormal Psychology. 2017;126(6):739. doi: 10.1037/abn0000282. [DOI] [PubMed] [Google Scholar]