Abstract
Background
School closures and home confinement due to the ongoing COVID-19 pandemic may lead to disrupted sleep patterns. Consequently, it could increase the risk of children and adolescents’ mental health disorders.
Methods
In this prospective study, we randomly selected ten schools in Shanghai and conducted cluster sampling of students from each school. The first wave of the survey was conducted between January 3 and 21, 2020. Approximately two months after the COVID-19 outbreak declared, a second wave of the survey was conducted. In total, 2427 individuals were surveyed in both waves using the same sampling method. Participants’ mental health status (depression, anxiety and stress), sleep patterns and other demographic information were measured in both waves. Multivariate regression analysis was used to examine the associations between sleep patterns and mental health status.
Results
During the COVID-19 pandemic, a total of 873 participants (19.9%), 1100 participants (25.1%), and 670 participants (15.3%) reported depression, anxiety, and stress symptoms, respectively. Significant changes of both sleep duration and sleep-wake cycle patterns were observed before and during the COVID-19 pandemic. Moreover, shorter sleep duration and late to rise patterns (including early to bed late to rise and late to bed late to rise) were found to be associated with higher odds of having mental illnesses during the pandemic.
Conclusion
These results suggest there is a pressing need to monitor children's and adolescents’ health behavior and mental health and develop timely evidence‐based strategies and interventions to mitigate adverse behavioral and psychological impacts caused by these unprecedented challenges.
Keywords: Sleep patterns, Mental health, Children and adolescents, COVID-19, School closure
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has caused many countries to enter nationwide or localized lockdown status. To reduce the transmission of COVID-19, many countries had carried out school closure measures. According to the United Nations Educational, Scientific and Cultural Organization (UNESCO), as of March 18, 2021, schools in 29 countries have been closed, and the affected students account for 9.8% of the total number of registered students in the world (https://en.unesco.org/covid19/educationresponse). This is impacting over 61% of the world's student population. When the daily routine of attending schools is disrupted due to school closures, children and adolescents who are confined to the home are vulnerable to becoming anxious and developing mental health problems such as anxiety, depression and stress due to fear, self-isolation and disrupted sleep (Lee, 2020; Orgilés et al., 2020; Sprang and Silman, 2013; Xie et al., 2020). One recent web-based study suggested that people younger than 35 were more likely to develop anxiety and depressive symptoms than those who were older during the COVID-19 outbreak in China (Huang and Zhao, 2020). It is concerning that children and adolescents are particularly vulnerable to the mental health effects of the COVID-19 pandemic as they may not be able to communicate their feelings like adults (Fegert et al., 2020; Wang et al., 2020a); also, they may have limited coping strategies. As such, for children and adolescents, more research on targeted interventions and health care to mitigate the effects of the pandemic on mental health is warranted (Marques de Miranda et al., 2020).
It has been anticipated that disrupted sleep patterns due to school closures and home confinement can have negative effects on children and adolescents’ mental health (Altena et al., 2020; Wang et al., 2020b). Sleep pattern changes including sleep duration and sleep-wake cycle changes were reported during or after previous viral epidemic outbreak events such as Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) (Chen et al., 2006; Lee et al., 2018). Sleep disruption is one of the significant problems caused by the pandemic, and it will affect the mental health of the general public (Jung et al., 2020). A causal effect of sleep disruption on mental health outcomes among college students was uncovered by a large randomized control trial at 26 UK universities (Freeman et al., 2017). The interaction between disturbed sleep patterns and mental health might further aggravate the degree of mental illness.
During the ongoing COVID-19 pandemic, evidence on sleep pattern changes in children and adolescents and their potential associations with mental health remain scarce. In this study, we surveyed over 4300 students who were out of school during the COVID-19 pandemic in Shanghai, the largest city in China, to investigate the sleep pattern changes and examine the associations of sleep patterns with mental health. The results show that school closure and family grounding may disrupt the normal sleep pattern, and the interruption of sleep pattern has an adverse effect on the mental health of adolescents. As China was the first country to fight against and contain COVID-19, evidence established by this study will be informative and helpful to other countries that are currently making efforts to mitigate the impact of the pandemic.
2. Methods
2.1. Participants
We conducted a prospective study among children and adolescents aged 6–17 years randomly selected from seven districts with a high population density in Shanghai, China. The data were collected through an online questionnaire platform Questionnaire Star. A total of 7544 children and adolescents from ten randomly sampled schools participated in the first wave of the survey conducted between January 3 and 21, 2020, right before the COVID-19 outbreak (a public health emergency was enacted in Shanghai on January 24, 2020). Approximately two months after the COVID-19 outbreak declared, a second wave of the survey was conducted among 4793 children and adolescents from seven schools, which included five out of the ten schools from the first wave of the survey and one newly joined school. It took place from March 13 to 23, 2020 (when the public health emergency response was downgraded from the highest level to level two in Shanghai). In total, 2427 children and adolescents were surveyed in both waves. During both waves of the survey, children's and adolescents’ mental health status, sleep patterns and other demographic information were measured. Meanwhile, their parents were invited to complete a questionnaire on their own sleep patterns and socioeconomic status, including maternal and/ or paternal age, maternal and/ or paternal education, and annual household income. The response rates were 0.83 and 0.93 in each wave of the survey, respectively.
2.2. Ethical considerations
Ethics approval was obtained from the Ethics Committee of Shanghai Jiaotong University School of Medicine (SJUPN-201813). Written, informed consent was obtained from caregivers of all participants.
2.3. Outcome measure
In the second wave of the survey (i.e., during the COVID-19 pandemic), the mental health of children and adolescents was assessed using a Chinese version of the 21-item self-reported short form of the 42-item Depression Anxiety Stress Scales (DASS) (Lovibond, Lovibond, & Psychology Foundation of, 1995), which consists of three 7-item self-report scales that assess symptoms of depression, anxiety and stress. The Chinese version of DASS-21 has been validated in adolescent populations in China (Mellor et al., 2015; Zhang et al., 2016). This survey of children and adolescents during the pandemic showed that the Cronbach's alpha of the depression, anxiety and stress subscale of DASS-21 were 0.913, 0.883 and 0.898, respectively. Participants were asked to rate the extent to which they had experienced each item over the past week on a four-point severity/frequency scale. The scale ranges from 0 (did not apply to me at all) to 3 (applied to me very much or most of the time). Subscale scores for each separate symptom - that is, depression, anxiety and stress - were calculated by summing the scores for the relevant items and multiplying by two. Cut-off scores defining normal/mild/moderate/severe and extremely severe have been developed, as shown in Table 1 . Summed scores equal to or over 10, 8 and 15 are considered clinically significant for the depression, anxiety and stress scales, respectively.
Table 1.
DASS severity ratings.
| Severity | Depression | Anxiety | Stress |
|---|---|---|---|
| Normal | 0–9 | 0–7 | 0–14 |
| Mild | 10–13 | 8–9 | 15–18 |
| Moderate | 14–20 | 10–14 | 19–25 |
| Severe | 21–27 | 15–19 | 26–33 |
| Extremely Severe | 28+ | 20+ | 34+ |
2.4. Sleep patterns measure
The sleep patterns of students were assessed using self-administered questionnaires during both waves of the survey. Parents’ sleep patterns were gathered in the second wave of the survey as well. Specific questions referring to sleep patterns were created and posed to students and their parents: (1) Over the past month, regular wake-up time during schooldays/ workdays (i.e., Monday to Friday); (2) over the past month, regular bedtime during schooldays/ workdays; (3) over the past month, regular wake-up time during weekends and (4) over the past month, regular bedtime during weekends. Wake-up time was defined as the end of the first sleeping bout of the day and bedtime was defined as the start of the last sleeping bout of the day. Sleep duration was thus calculated in each 24 h period. In addition, using median splits for bedtime and wake-up time, the sleep timing behavior of participants was classified into one of the four sleep timing behavior categories: early to bed early to rise (EE), early to bed late to rise (EL), late to bed early to rise (LE) and late to bed late to rise (LL).
2.5. Socio-demographic position
Socio-demographic information on the children and their parents was obtained in the second wave of the survey, including children's sex, children's age, parents’ age, parents’ education attainment level and annual household income.
2.6. Statistical analysis
For the 2427 participants who were surveyed in both waves, the distributions of their sleep duration were assessed against normality using Shapiro-Wilk test and Q-Q plots stratified by weekdays and weekends. When sleep duration demonstrated a non-normal distribution, Wilcoxon signed-rank test was used to compare the sleep duration before and during the COVID-19 pandemic. Sleep-wake cycle patterns (i.e., EE, EL, LE or LL) were compared between two stages (i.e., before and during the pandemic) using McNemar's Chi-squared test.
For all 4391 participants surveyed in the second wave, their sleep duration was compared between weekdays and weekends using Wilcoxon signed-rank test. Weekly weighted average sleep duration (i.e., average of five weekdays and two weekend days) was calculated by adding weekday sleep duration multiplied by 5/7 and weekend sleep duration multiplied by 2/7. Participants in the second wave were classified into five categories of weekly weighted average sleep duration:<8 h, 8,9 h,9,10 h,10,11 h and ≥11 h. Differences in the proportions of socio-demographic characteristics, parents’ sleep duration and mental health status (depression, anxiety and stress) of children and adolescents across the four sleep duration categories were tested using Chi-squared test. A multivariate logistic regression analysis was used to examine the associations between sleep duration and multiple mental health outcomes including depression, anxiety and stress, adjusting for sex, age, maternal education, paternal education and parents’ weekly sleep duration. One of the sleep duration categories, 8,9 h, was used as the reference category (recommended level) in the logistic regression analysis, as it was reported that more than 60% of Chinese children and adolescents aged between 6 and 17 years slept for less than 8 h per day in a nationwide survey in 2019 (http://report.iresearch.cn/report_pdf.aspx?id=3355). In addition, a multivariate regression analysis was used to examine the associations between sleep-wake cycle patterns and mental health status with adjusting for sex, age, maternal education, paternal education and parents’ sleep-wake cycle patterns, stratified by weekdays and weekends. To reduce the risk of bias from missing data, multiple imputation was conducted using multivariate imputation by chained equations algorithm and 10 imputed datasets were generated (van Buuren and Groothuis-Oudshoorn, 2011). All statistical analyses were performed using SPSS (IBM SPSS 25.0, SPSS Inc). P value less than 0.05 was considered as statistically significant in all analyses.
3. Results
During the COVID-19 pandemic, among the 4391 children and adolescents surveyed in the second wave, a total of 873 participants (19.9%), 1100 participants (25.1%), and 670 participants (15.3%) reported depression, anxiety, and stress symptoms, respectively. The age and gender specific prevalence of these mental health disorders can be found in the online supplementary materials.
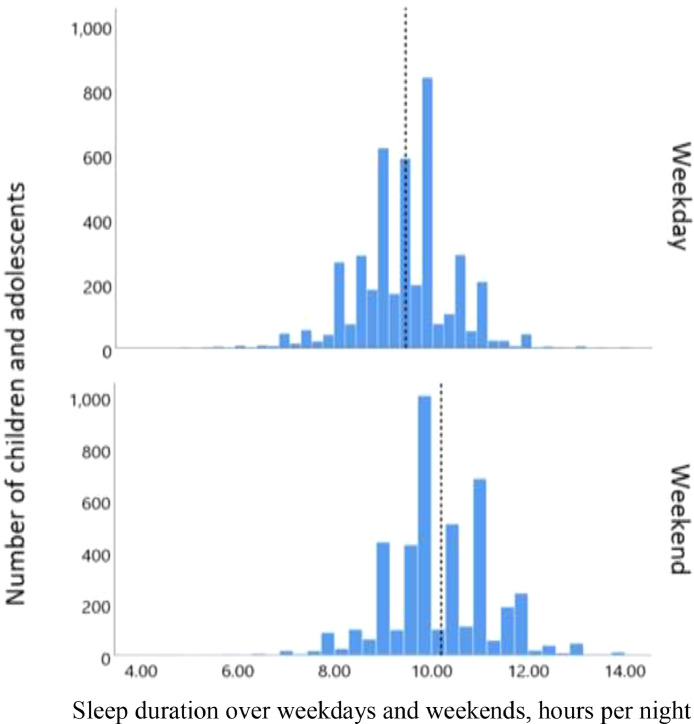
As shown in Fig. 1 , the median sleep duration during weekdays was 8.7 h before the pandemic and 9.5 h during the pandemic, and equivalently 10 h during weekends before and during the pandemic. Wilcoxon signed-rank test suggested that there were statistically significant differences (p < 0.001) in sleep duration during weekdays and weekends between the two phases (i.e., before and during the COVID-19 pandemic).
Fig. 1.
Sleep duration before and during the COVID-19 pandemic (N = 2427).
Percentage for children and adolescents with different sleep patterns (%).
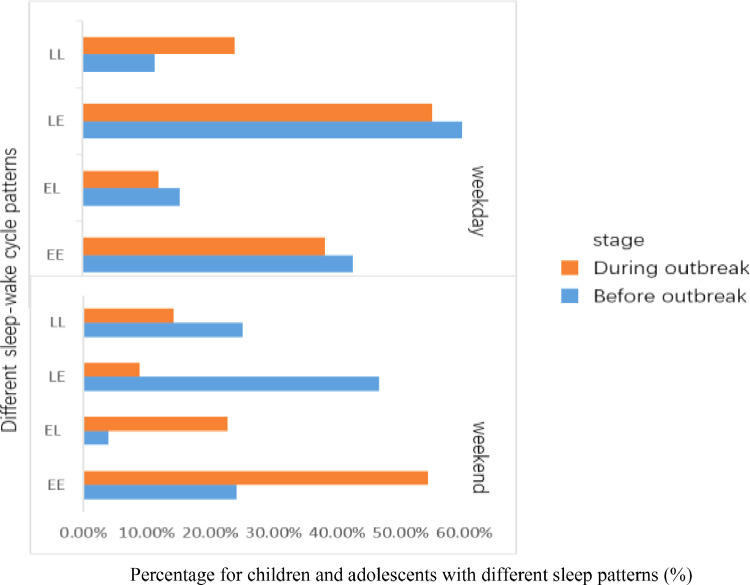
Children and adolescents were more likely to follow LE and EE patterns during weekdays and an LE pattern during weekends before the COVID-19 pandemic (i.e., normal mode). After the pandemic and subsequent school closures began, more children and teenagers switch to an LL pattern mode on weekdays and EL and EE patterns on weekends. These changes were assessed as statistically significant using McNemar's Chi-squared test (p < 0.05) (Fig. 2 ).
Fig. 2.
Different sleep-wake cycle patterns for children and adolescents before and during the COVID-19 pandemic (N = 2427).
Sleep duration over weekdays and weekends, hours per night.
For the 4391 participants surveyed in the second wave, the median sleep durations were 9.4 h and 10.2 h during weekdays and weekends, respectively (Fig. 3 ). Differences in sleep duration distribution between weekdays and weekends were suggested by the results of Wilcoxon signed-rank test (p < 0.05). The age and gender specific median weekly sleep duration during the pandemic can be found in the online supplementary materials.
Fig. 3.
Sleep duration distribution over weekdays and weekends during the COVID-19 pandemic (N = 4391).
The univariate analysis suggested that children's and adolescents’ sex, age, paternal education, annual household income, parents’ weekday sleep duration and children's mental health status (depression, anxiety and stress) significantly differed across the four sleep duration categories, as shown in Table 2 .
Table 2.
Socio-demographic characteristics and mental health status of children and adolescents (N = 4391).
| Characteristics | Reported weekly weighted average sleep duration, h/ night |
χ2 | P value | ||||
|---|---|---|---|---|---|---|---|
| <8 | 8,9 | 9,10 | 10,11 | ≥11 | |||
| Sex | 13.891 | 0.008 | |||||
| Male | 64(43.0%) | 332(45.9%) | 1009(52.0%) | 551(51.1%) | 161(55.1%) | ||
| Female | 85(57.0%) | 392(54.1%) | 933(48.0%) | 527(48.9%) | 131(44.9%) | ||
| Age | 817.05 | <0.001 | |||||
| ≤9 | 2(1.6%) | 8(1.2%) | 160(9.8%) | 358(27.4%) | 88(30.6%) | ||
| 10–12 | 14(10.9%) | 110(16.5%) | 507(31.0%) | 462(35.3%) | 85(29.5%) | ||
| 13−15 | 80(62.0%) | 445(66.7%) | 918(56.1%) | 479(36.6%) | 115(39.9%) | ||
| ≥16 | 33(25.6%) | 104(15.6%) | 52(3.2%) | 9(0.7%) | 0(0.0%) | ||
| Maternal education | 22.386 | 0.004 | |||||
| Secondary school or lower | 12(14.3%) | 46(9.5%) | 156(9.7%) | 84(8.9%) | 36(14.0%) | ||
| High school | 66(78.6%) | 403(82.9%) | 1377(85.9%) | 830(87.9%) | 211(82.1%) | ||
| College or higher | 6(7.1%) | 37(7.6%) | 70(4.4%) | 30(3.2%) | 10(3.9%) | ||
| Paternal education | 20.885 | 0.007 | |||||
| Secondary school or below | 8(9.5%) | 37(7.6%) | 133(8.3%) | 62(6.6%) | 28(10.9%) | ||
| High school | 63(75.0%) | 399(82.1%) | 1349(84.2%) | 821(87.0%) | 215(83.7%) | ||
| College or above | 13(15.5%) | 50(10.3%) | 121(7.6%) | 61(6.5%) | 14(5.5%) | ||
| Annual household income (CNY) | 19.421 | 0.247 | |||||
| <100k | 18(21.4%) | 72(14.8%) | 201(12.5%) | 127(13.5%) | 41(16.0%) | ||
| 100k to 200k | 26(31.0%) | 157(32.3%) | 517(32.6%) | 309(32.7%) | 92(35.8%) | ||
| 200k to 400k | 24(28.6%) | 139(28.6%) | 515(32.1%) | 319(33.8%) | 76(29.6%) | ||
| >400k | 7(8.3%) | 67(13.8%) | 229(14.3%) | 122(12.9%) | 32(12.5%) | ||
| Others | 9(10.7%) | 51(10.5%) | 141(8.8%) | 67(7.1%) | 16(6.2%) | ||
| Parents weekly weighted average sleep duration (h/night) | 303.696 | <0.001 | |||||
| <8 | 48(36.6%) | 169(26.9%) | 233(13.6%) | 96(10.0%) | 24(9.3%) | ||
| 8,9 | 44(33.6%) | 270(42.9%) | 732(42.6%) | 334(34.9%) | 69(26.6%) | ||
| 9,10 | 29(22.1%) | 165(26.2%) | 646(37.6%) | 402(42.1%) | 112(43.2%) | ||
| 10,11 | 7(5.3%) | 20(3.2%) | 80(4.7%) | 95(9.9%) | 28(10.8%) | ||
| ≥11 | 3(2.3%) | 5(0.8%) | 28(1.6%) | 29(3.0%) | 26(10.0%) | ||
| 61.624 | <0.001 | ||||||
| Depression | |||||||
| No | 90(60.4%) | 557(76.93%) | 1628(83.83%) | 889(82.47%) | 237(81.16%) | ||
| Yes | 59(39.6%) | 167(23.07%) | 314(16.17%) | 189(17.53%) | 55(18.84%) | ||
| Anxiety | 77.985 | <0.001 | |||||
| No | 76(51.0%) | 506(69.9%) | 1532(78.9%) | 840(77.9%) | 228(78.1%) | ||
| Yes | 73(49.0%) | 218(30.1%) | 410(21.1%) | 238(22.1%) | 64(21.9%) | ||
| Stress | 93.76 | <0.001 | |||||
| No | 95(63.8%) | 581(80.3%) | 1721(88.6%) | 938(87.0%) | 256(87.7%) | ||
| Yes | 54(36.2%) | 143(19.8%) | 221(11.4%) | 140(13.0%) | 36(12.3%) | ||
In the multivariate analysis of the association of sleep duration with mental health outcomes, as shown in Table 3 , Model 1 (without adjustment) suggested that compared to a daily 8,9 h sleep duration, children and adolescents who slept less than 8 h were more likely to have mental illnesses such as depression. After adjusting for potential confounding variables and covariates, the analysis of multiply imputed data using Model 2 (with adjustment) consistently revealed that children and adolescents who had less than 8 h sleep time had significantly higher odds of having depression (2.23-fold increase, adjusted OR = 2.23, 95% CI: 1.33, 3.73), anxiety (2.53-fold increase, adjusted OR = 2.53, 95% CI: 1.55, 4.12), and stress (2.78-fold increase, adjusted OR = 2.78, 95% CI: 1.68,4.61), respectively compared with those had 8–9 h of daily sleep, 9,10 h seems to be the best sleep duration, and its adjusted ORs of anxiety and depression are the smallest compared with 8–9 h of daily sleep, anxiety (adjusted OR =0.75, 95% CI: 0.58, 0.97), and stress (adjusted OR = 0.61, 95% CI: 0.45,0.83), but there is no significant difference in depression. There was no significant difference in anxiety, depression and stress among 10,11 h, ≥ 11 h and 8,9 h sleep duration groups. As shown in Table 4 , the multivariate regression analysis results of the associations between sleep-wake cycle patterns and mental health outcomes revealed that during weekdays compared to children and adolescents who followed an EE sleep-wake cycle pattern, those who followed an LE pattern were 1.71 folds more likely to have depression (adjusted OR = 1.71, 95% CI: 1.16, 2.53), there was no significant difference in anxiety and stress. Those who followed an LL pattern were 3.03 folds more likely to have depression (adjusted OR = 3.03, 95% CI: 2.07, 4.43), 2.14 folds more likely to have anxiety (adjusted OR =2.14, 95% CI: 1.47, 3.10) and 1.86 folds more likely to have stress (adjusted OR = 1.86, 95% CI: 1.18, 2.94). No significant differences in mental health outcomes were found between EE and EL patterns. Interestingly, on weekends, children and adolescents who follow the LL model are still more likely to have adverse psychological outcomes than those who follow the EE model, 2.19 folds more likely to have depression (adjusted OR = 2.19, 95% CI: 1.7, 2.81) and 1.78 folds more likely to have anxiety (adjusted OR = 1.78, 95% CI: 1.41, 2.25), and 1.97 folds more likely to have stress (adjusted OR = 1.97, 95% CI: 1.49, 2.61). Compared with children and adolescents who follow EE pattern, children and adolescents who follow EL and LE pattern on weekends are more likely to suffer from depression and anxiety, respectively. In other adverse mental health outcomes, children and adolescents did not show a higher risk.
Table 3.
Associations between sleep duration and mental health outcomes.
| Sleep duration | Model 1 |
Model 2 |
||||
|---|---|---|---|---|---|---|
| OR (95% CI) |
OR (95% CI) |
|||||
| Depression | Anxiety | Stress | Depression | Anxiety | Stress | |
| <8 | 2.81(1.66,4.75) | 3.07 (1.87,5.07) | 3.09(1.80,5.30) | 2.23(1.33,3.73) | 2.53(1.55,4.12) | 2.78(1.68,4.61) |
| 8,9(ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| 9,10 | 0.85(0.63,1.14) | 0.80(0.61,1.04) | 0.71(0.51,0.98) | 0.77(0.58,1.03) | 0.75(0.58,0.97) | 0.61(0.45,0.83) |
| 10,11 | 0.92(0.67,1.26) | 0.89(0.67,1.19) | 0.83(0.59,1.18) | 0.86(0.64,1.16) | 0.87(0.67,1.14) | 0.74(0.54,1.02) |
| ≥11 | 0.92(0.60,1.44) | 0.83(0.55,1.23) | 0.59(0.35,1.00) | 0.94(0.62,1.42) | 0.87(0.59,1.28) | 0.66(0.41,1.06) |
Model 1 without adjusting for confounders or covariates based on complete data.
Model 2 adjusting for sex, age, maternal education, paternal education and parental weekly sleep duration based on multiply imputed data.
Table 4.
Associations between sleep-wake cycle patterns and mental health outcomes∗.
| Sleep-wake cycle patterns |
Model 1 OR (95% CI) |
|||||
|
Weekdays |
Weekends |
|||||
|
OR (95% CI) |
OR (95% CI) |
|||||
| Depression | Anxiety | Stress | Depression | Anxiety | Stress | |
| EE (ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| EL | 1.36(0.48,3.91) | 1.71(0.66,4.41) | 1.30(0.36,4.73) | 3.05(1.32,7.09) | 3.111(1.39,6.96) | 2.35(0.84,6.52) |
| LE | 1.64(1.29,2.08) | 1.48(1.20,1.83) | 1.35(1.04,1.77) | 1.31(1.01,1.69) | 1.28(1.02,1.605) | 1.21(0.90,1.62) |
| LL | 2.24(1.30,3.86) | 2.08(1.24,3.48) | 1.35(0.67,2.70) | 2.51(1.81,3.48) | 2.28(1.69,3.08) | 2.53(1.76,3.65) |
| Sleep-wake cycle patterns |
Model 2 OR (95% CI) |
|||||
|
Weekdays |
Weekends |
|||||
|
OR (95% CI) |
OR (95% CI) |
|||||
| Depression | Anxiety | Stress | Depression | Anxiety | Stress | |
| EE (ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| EL | 1.24(0.95,1.62) | 1.15(0.90,1.48) | 1.05(0.77,1.44) | 1.42(1.11,1.81) | 1.25(1.00,1.56) | 1.17(0.88,1.55) |
| LE | 1.71(1.16,2.53) | 1.37(0.96,1.96) | 1.39(0.91,2.1) | 1.30(0.92,1.85) | 1.14(0.83,1.57) | 1.49(1.02,2.16) |
| LL | 3.03(2.07,4.43) | 2.14(1.47,3.10) | 1.86(1.18,2.94) | 2.19(1.7,2.81) | 1.78(1.41,2.25) | 1.97(1.49,2.61) |
Model 1 without adjusting for confounders or covariates based on complete data.
Model 2 adjusting for sex, age, maternal education, paternal education and children and adolescents weekly sleep duration based on multiply imputed data.
4. Discussion
In the present study, 19.9%, 25.1%, and 15.3% of children and adolescents were reported to have depression, anxiety, and stress symptoms, respectively, during the COVID-19 pandemic in Shanghai, China. The prevalence of depression was lower than that reported in a previous study carried out in the epidemic center, Wuhan, China (22.6%) (Xie et al., 2020) but higher than a meta-analyzed prevalence of depression (17.2%) among primary school students in China (Xu et al., 2020). Significant changes of both sleep duration and sleep-wake cycle patterns were observed before and during the COVID-19 pandemic. In addition, shorter sleep duration and late to bed and late to rise patterns were found to be associated with a higher risk of mental illness during the pandemic.
It has been widely anticipated that the COVID-19 pandemic will have an imperative impact on children ’s and adolescents’ sleep and mental health (Altena et al., 2020; Becker and Gregory, 2020; Golberstein et al., 2020). School closure and home confinement might disrupt regular sleep patterns. During this period, sleep and circadian rhythms markedly changed, also reporting a lower sleep quality. The increase in sleep difficulties was stronger for people with a higher level of depression, anxiety, and stress symptomatology, and associated with the feeling of elongation of time (Cellini et al., 2020). These sleep patterns are established and maintained to align with normal school time such as early wake up due to morning commute. In the present study, children and adolescents had longer sleep duration and were more prone to follow a late to bed late to rise the sleep-wake cycle pattern over weekdays during the pandemic than before it. In addition, the association between sleep patterns and mental health outcomes was almost as strong on weekdays as on weekends, suggesting that a healthy and appropriate sleep pattern should be followed every day and the effect of weekends should not be ignored, even though weekends are only two days. Furthermore, less physical activity, more screen time, more often exposure to stressful news via social media and family financial difficulties due to the pandemic and home confinement might worsen children and adolescents’ sleep disruption (Lee, 2020; Tsai et al., 2018; Wang et al., 2020a). As another imperative adverse effect of the pandemic, mental health problem has been widely recognized as one of the public health challenges emerging over the COVID-19 pandemic (Holmes et al., 2020; Luo et al., 2020). Recent studies across diverse populations from different countries reported an overall high psychological impact of the pandemic among healthcare workers, the general public and patients with pre-existing conditions or COVID-19 infection (Luo et al., 2020). Thus, immediate actions and longer term strategic and mechanistically driven interventions are called for to mitigate its consequences, especially in vulnerable groups such as children and adolescent populations (Golberstein et al., 2020; Holmes et al., 2020).
Sleep plays an important role in mental health of children and adolescents (Gregory and Sadeh, 2016). It has been reported in previous studies that disrupted sleep patterns have an adverse effect on youth mental health (Liu and Buysse, 2006; Liu et al., 2007; Lovato and Gradisar, 2014; Shanahan et al., 2014). The mechanisms underlying the relationship between sleep disruption and mental health include genetic and environmental perspectives (Barclay and Gregory, 2013; Van den Oord et al., 2000). Circadian genes such as ARNTL, PER1, PER2, and DBP were reported to be involved in daily rhythmic events including sleep-wake cycle and risk loci for major depressive disorder (Bunney et al., 2015; Li et al., 2013). In the context of the COVID-19 pandemic, sleep disruption and its consequent impact on mental health are more likely to be explained from an environmental perspective (Chen et al., 2014; Wang et al., 2020a). Circadian rhythm, an endogenous timing system established to adapt to regular environmental changes such as light and temperature, might be altered over the pandemic due to school closure and mobility restrictions. Consequently, it can influence sleep duration and sleep-wake cycles, which is evident in the present study. Furthermore, mental health problems will be caused by disrupted circadian rhythms and sleep patterns (Alvaro et al., 2013; Freeman et al., 2017; Lovato and Gradisar, 2014).
There are certain strengths and limitations of this study. This study utilized a unique data source, that is, one survey right before the COVID-19 outbreak and the other during the pandemic, to provide informative evidence such as prevalence of mental health problems during the pandemic and sleep pattern changes before and during the pandemic in children and adolescents. High response rates of both waves of the survey yielded high quality usable data and representative results. There were several limitations in this study. Firstly, reliance on self-reported information suffers from potential recall errors and reporting biases. Secondly, this survey lacks related indicators of sleep disorders and measures of sleep habits. We can't confirm that sleep duration computed as the time between bedtime and wake-up time is actually the time spent in bed, and whether it also includes sleep onset and wake after sleep onset. Thirdly, sleep quality as a disturbing factor in the various stages, which might reflect different sleep habits of adolescents across age groups, was not examined in this study due to absence of available data. Another important limitation of this study is that in the baseline wave of the survey, mental health status of students was measured using a Chinese version of Children's Depression Inventory (Wu et al., 2010) but due to unreliable quality of responses based on students’ reflection against the questions in the inventory, we used an easier to understand tool DASS-21 during the pandemic instead, thus in the present study we only used mental health outcomes measured during the pandemic. It might lose the opportunity to examine the causal association between sleep patterns and mental health outcomes with leveraging the prospective observational design advantage of this study.
Considering that the lockdown is likely to continue in many countries and a second wave of COVID-19 is a real risk (Adebowale et al., 2020), there is a pressing need to monitor children and adolescents’ health behavior and mental health and develop timely evidence‐based strategies and interventions to mitigate adverse behavioral and psychological impacts caused by these unprecedented challenges. Particularly, for children and adolescents who are living in lower-income and middle-income countries, due to the already fragile and fragmented health care systems, health care services access might be disrupted or limited during the COVID-19 pandemic. Efforts to respond to these challenges such as adoption of digital health intervention alongside conventional therapies are recommended.
CRediT authorship contribution statement
Jian Zhao: Formal analysis, Writing – original draft, Writing – review & editing. Jiawei Xu: Formal analysis, Writing – original draft, Writing – review & editing. Yaping He: Conceptualization, Funding acquisition, Writing – review & editing. Mi Xiang: Conceptualization, Funding acquisition, Writing – review & editing.
Declaration of Competing Interest
None.
Acknowledgments
This research was funded by the National Natural Science Foundation of China (Grant No. 71804110), Shanghai Science and Technology Development Funds (Grant No. 21QA1405300), Science Foundation for new teachers of Shanghai Jiao Tong University School of Medicine (Grant No. 20×100040012), and Shanghai Municipal Health Commission (GW-10.1-XK07) for Mi Xiang and supported by Global Public Health strand of the Elizabeth Blackwell Institute for Health Research funded under the University of Bristol's QR GCRF strategy.
References
- Adebowale V., Alderson D., Burn W., Dixon J., Godlee F., Goddard A., Taylor J. COVID-19: call for a rapid forward looking review of the UK's preparedness for a second wave-an open letter to the leaders of all UK political parties. BMJ. 2020;369:m2514. doi: 10.1136/bmj.m2514. [DOI] [PubMed] [Google Scholar]
- Altena E., Baglioni C., Espie C.A., Ellis J., Gavriloff D., Holzinger B., Riemann D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J. Sleep. Res. 2020:e13052. doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- Alvaro P.K., Roberts R.M., Harris J.K. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059–1068. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barclay N.L., Gregory A.M. Quantitative genetic research on sleep: a review of normal sleep, sleep disturbances and associated emotional, behavioural, and health-related difficulties. Sleep Med. Rev. 2013;17(1):29–40. doi: 10.1016/j.smrv.2012.01.008. [DOI] [PubMed] [Google Scholar]
- Becker S.P., Gregory A.M. Editorial Perspective: perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. J. Child Psychol. Psychiatry. 2020 doi: 10.1111/jcpp.13278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunney B.G., Li J.Z., Walsh D.M., Stein R., Vawter M.P., Cartagena P., Bunney W.E. Circadian dysregulation of clock genes: clues to rapid treatments in major depressive disorder. Mol. Psychiatry. 2015;20(1):48–55. doi: 10.1038/mp.2014.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020:e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Chou K.R., Huang Y.J., Wang T.S., Liu S.Y., Ho L.Y. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. Int. J. Nurs. Stud. 2006;43(2):215–225. doi: 10.1016/j.ijnurstu.2005.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T., Wu Z., Shen Z., Zhang J., Shen X., Li S. Sleep duration in Chinese adolescents: biological, environmental, and behavioral predictors. Sleep Med. 2014;15(11):1345–1353. doi: 10.1016/j.sleep.2014.05.018. [DOI] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health. 2020;14 doi: 10.1186/s13034-020-00329-3. 20-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman D., Sheaves B., Goodwin G.M., Yu L.M., Nickless A., Harrison P.J., Espie C.A. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. 2017;4(10):749–758. doi: 10.1016/S2215-0366(17)30328-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Gregory A.M., Sadeh A. Annual research review: sleep problems in childhood psychiatric disorders–a review of the latest science. J. Child Psychol. Psychiatry. 2016;57(3):296–317. doi: 10.1111/jcpp.12469. [DOI] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung, S., Kneer, J., & Krueger, T. (2020). The German COVID-19 survey on mental health: primary results. medRxiv, doi: 10.1101/2020.05.06.20090340. [DOI]
- Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Health. 2020 doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J.Z., Bunney B.G., Meng F., Hagenauer M.H., Walsh D.M., Vawter M.P., Bunney W.E. Circadian patterns of gene expression in the human brain and disruption in major depressive disorder. Proc. Natl. Acad. Sci. U.S.A. 2013;110(24):9950–9955. doi: 10.1073/pnas.1305814110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Buysse D.J. Sleep and youth suicidal behavior: a neglected field. Curr. Opin. Psychiatry. 2006;19(3):288–293. doi: 10.1097/01.yco.0000218600.40593.18. [DOI] [PubMed] [Google Scholar]
- Liu X., Buysse D.J., Gentzler A.L., Kiss E., Mayer L., Kapornai K., Kovacs M. Insomnia and hypersomnia associated with depressive phenomenology and comorbidity in childhood depression. Sleep. 2007;30(1):83–90. doi: 10.1093/sleep/30.1.83. [DOI] [PubMed] [Google Scholar]
- Lovato N., Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med. Rev. 2014;18(6):521–529. doi: 10.1016/j.smrv.2014.03.006. [DOI] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques de Miranda D., da Silva Athanasio B., Sena Oliveira A.C., Simoes-E-Silva A.C. How is COVID-19 pandemic impacting mental health of children and adolescents? Int. J. Disaster Risk Reduct. IJDRR. 2020;51 doi: 10.1016/j.ijdrr.2020.101845. -101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellor D., Vinet E.V., Xu X., Mamat N.H.B., Richardson B., Román F. Factorial invariance of the DASS-21 among adolescents in four countries. Eur. J. Psychol. Assess. 2015;31(2):138–142. doi: 10.1027/1015-5759/a000218. [DOI] [Google Scholar]
- Orgilés, M., Morales, A., Delveccio, E., Mazzeschi, C., & Espada, J.P. (2020). Immediate psychological effects of COVID-19 quarantine in youth from Italy and Spain. Available at SSRN 3588552. [DOI] [PMC free article] [PubMed]
- Shanahan L., Copeland W.E., Angold A., Bondy C.L., Costello E.J. Sleep problems predict and are predicted by generalized anxiety/depression and oppositional defiant disorder. J. Am. Acad. Child Adolesc. Psychiatry. 2014;53(5):550–558. doi: 10.1016/j.jaac.2013.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Tsai K.M., Dahl R.E., Irwin M.R., Bower J.E., McCreath H., Seeman T.E., Fuligni A.J. The Roles of Parental Support and Family Stress in Adolescent Sleep. Child Dev. 2018;89(5):1577–1588. doi: 10.1111/cdev.12917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S., Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J. Stat. Softw. 2011;45(3):67. doi: 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- Van den Oord E., Boomsma D.I., Verhulst F.C. A study of genetic and environmental effects on the co-occurrence of problem behaviors in three-year-old twins. J. Abnorm. Psychol. 2000;109(3):360–372. doi: 10.1037/0021-843X.109.3.360. [DOI] [PubMed] [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395(10228):945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Xie L., Xu Y., Yu S., Yao B., Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup. Med. 2020 doi: 10.1093/occmed/kqaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu W.F., Lu Y.B., Tan F.R., Yao S.Q. Reliability and validity of the Chinese version of children's depression inventory. Chin. Ment. Health J. 2010;24(10):775–779. [Google Scholar]
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu D.D., Rao W.W., Cao X.L., Wen S.Y., An F.R., Che W.I., Xiang Y.T. Prevalence of depressive symptoms in primary school students in China: a systematic review and meta-analysis. J. Affect. Disord. 2020;268:20–27. doi: 10.1016/j.jad.2020.02.034. [DOI] [PubMed] [Google Scholar]
- Zhang F., Liu Z., Zhujiang M., Hou Q. Application of the short version of depression-anxiety-stress scale to stress assessment on students after earthquake. Chin. J. Behav. Med. Brain Sci. 2016;25(1):82–85. [Google Scholar]