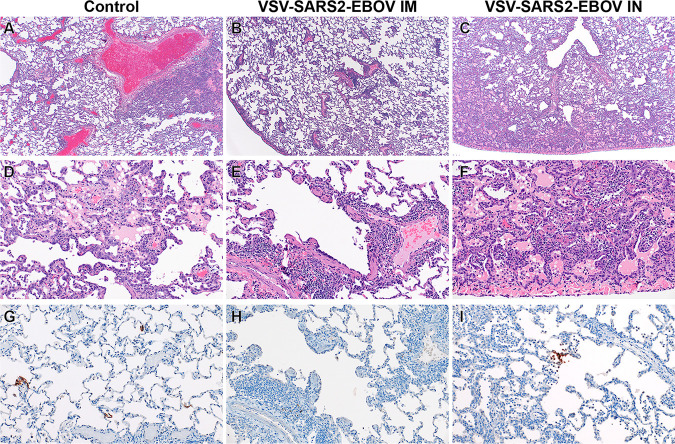
FIG 2.
Histopathology and immunohistochemistry of NHP lungs. (A) Pulmonary lesions depicting typical coronavirus respiratory pathologies, including locally extensive regions of bronchointerstitial pneumonia and proteinaceous fluid accumulation in adjacent alveoli (magnification, ×40; H&E). (B) Disseminated immunopathology with prominent perivascular lymphocytic cuffing and multifocal involvement at terminal airways (magnification, ×40; H&E). (C) i.n. vaccination shows pulmonary pathology characterized by a combination of interstitial pneumonia and immunopathology (magnification, ×40; H&E). (D) Foci of interstitial pneumonia are characterized by prominent type II pneumocyte hyperplasia, leukocyte infiltration, expansion of alveolar septa, and accumulation of low numbers of macrophages, neutrophils, and proteinaceous fluid in alveolar spaces (magnification, ×200; H&E). (E) Terminal airways and medium- to small-caliber blood vessels are cuffed by moderate numbers of lymphocytes with scattered eosinophils (magnification, ×200; H&E). (F) Foci of interstitial pneumonia show pronounced type II pneumocyte hyperplasia, thickening of alveolar septa by an infiltration of leukocytes, and leukocyte spillover into adjacent alveolar spaces, with moderate numbers of alveolar eosinophils noted and multifocal fibrin mats filling alveolar spaces (magnification, ×200; H&E). (G) Low numbers of type I pneumocytes in regions lacking pathology are immunoreactive for SARS-CoV-2 antibody (magnification, ×200; immunohistochemistry [IHC]). (H) SARS-CoV-2-specific immunoreactivity was not observed in evaluated sections of the i.m. vaccinated group (magnification, ×200; IHC). (I) Low numbers of type I pneumocytes and alveolar macrophages are immunoreactive for SARS-CoV-2 in select foci of interstitial pneumonia (magnification, ×200; IHC).