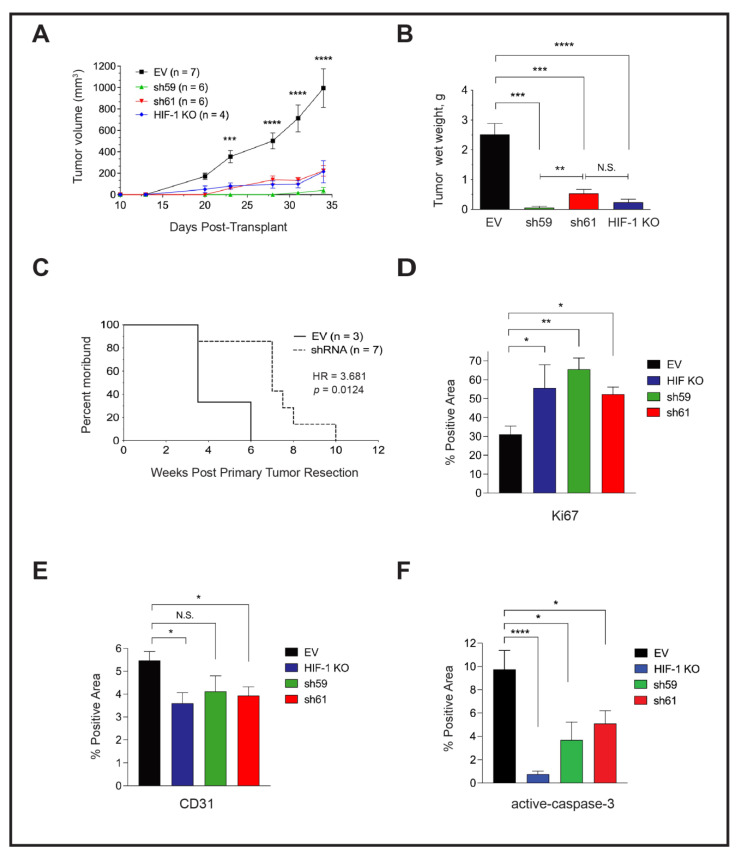
Figure 5.
Tumor-cell-intrinsic CKB promotes PyMT primary tumor growth and lung metastasis in vivo, and the deletion of CKB in the tumor epithelium improves overall survival. (A) Growth rate over time after transplantation of PyMT EV, HIF-1 KO, sh59 KD, and sh61 KD cells into the inguinal mammary fat pad of female FVB/Nj recipients. Mean tumor volume ± SEM is shown. (B) All tumors harvested at day 34 from panel (A) were weighed to determine the mean wet weight (g) ± SEM at the experiment endpoint. Data in (A,B) are representative of two independent experiments. (C) The impact of CKB expression in the PyMT tumor epithelium on the survival of recipients following tumor resection. Mice implanted with PyMT cells (EV or either shRNA KD construct) were subjected to primary tumor resection after tumors grew to similar volumes (~500 mm3), and mice were allowed to survive post-resection until moribund due to lung metastasis. Mice were removed from the study when panting due to lung metastasis, or if bodyweight decreased by >15%. The morbidity hazard ratio (HR) was 3.68-fold higher when FVB/Nj recipients bore Ckb WT tumors (n = 3 mice for EV and n = 7 total mice for Ckb shRNA knockdown, representing either sh59 KD or sh61 KD tumors). (D–F) Immunostaining of PyMT EV (n = 5 tumors), HIF-1 KO (n = 4 tumors), sh59 KD (n = 4 tumors) or sh61 KD (n = 5 tumors) sections to enumerate Ki67 (D), CD31 (E) or activated-caspase 3. (F) The mean ± SEM of the percentage (%) of the positive area of whole tumor sections is reported for each genotype.