Abstract
Osteoarthritis, as a degenerative disease, is a common problem and results in high socioeconomic costs and rates of disability. The most commonly affected joint is the knee and characterized by progressive destruction of articular cartilage, loss of extracellular matrix, and progressive inflammation. Mesenchymal stromal cell (MSC)-based therapy has been explored as a new regenerative treatment for knee osteoarthritis in recent years. However, the detailed functions of MSC-based therapy and related mechanism, especially of cartilage regeneration, have not been explained. Hence, this review summarized how to choose, authenticate, and culture different origins of MSCs and derived exosomes. Moreover, clinical application and the latest mechanistical findings of MSC-based therapy in cartilage regeneration were also demonstrated.
Keywords: Mesenchymal stromal cell, Osteoarthritis, Exosome, Regeneration, Cartilage
Background
Osteoarthritis is a common and disabling condition that represents substantial health and socioeconomic costs with notable implications for the individuals affected and healthcare systems [1, 2]. Global percentage change of years lived with disability in counts between 2006 and 2016 was 31.5% [3]. Knee osteoarthritis (KOA) is the most prevalent subtype of osteoarthritis [4] that shows symptoms with pain, swell, stiffness, and loss of mobility mainly in the aging and obese populations [5]. The pathogenesis of KOA is complicated, not only associated with the “wear and tear,” which is called mechanical stress [6]. Microenvironmental and genetic factors interact during deterioration that ultimately leads to degeneration of articular cartilage, intraarticular inflammation with synovitis, and changes in subchondral bone [7, 8]. Extracellular matrix (ECM) produced and secreted by chondrocytes and synovial fluid secreted by fibroblast-like synoviocytes are the two main important substances to maintain the microenvironment [9, 10]. Nonetheless, chondrocytes constitute only 2% of cartilage volume [11, 12] and may the first be activated by inflammatory signals originating from synovium or subchondral bone [13], which alter the balance between synthesis and degradation of ECM and cause the limited potential for self-regeneration of articular cartilage. Recommended treatment options range from non-care currently limited to pain control and merely improve the regeneration of articular cartilage in KOA.
Cell-based therapy and novel approaches using mesenchymal stromal cells (MSCs) or exosomes secreted by MSCs are presented as alternative cell-based sources to chondrocytes, which show potential for cartilage regeneration in KOA [14, 15]. The International Society for Cell & Gene Therapy refers MSCs as a bulk population with notable secretory, immunomodulatory, and homing properties. The minimal criteria include being plastic adherent, expressing specific surface markers, and capable of in vitro differentiation into adipocyte, chondrocyte, and osteoblast lineages [16]. MSCs and secreted exosomes (Exos) maintain therapeutical potentials for cartilage regeneration, including balancing metabolic activity of cartilage and the chondrogenic differentiation, which has been reported in animal studies and gaining positive outcomes in the clinic [17–19]. However, a common standard for cell selection and preparation for studies and applications of MSCs is not yet available. Moreover, the mechanism of MSCs and MSC-Exos for KOA is not demonstrated clearly yet. This paper briefly describes situations associated with currently used methods for cell selection and preparation, followed by a review of the existing literature on MSC-based cell therapy for cartilage regeneration in KOA.
MSCs and MSCs-exosomes: cell selection and preparation
Cell selection
Stromal cells having multipotent differentiation potentials with regenerative capacity can be generally classified into two groups: embryonic stromal cells and adult stromal cells [20]. Embryonic stromal cells contain cells from the term placenta, amniotic fluid, and umbilical cord. Adult stromal cells have been identified within most of the tissues or organs, and the following sources have been applied for treating KOA, such as bone marrow (BM) [21, 22], trabecular bone [23], adipose tissue (AT) [19], synovial fluid [24], synovium [25], and peripheral blood [26]. Stromal cells from different sources have different differentiation capacities, different clinical benefits, and cultural characteristics [27]. Hence, cell source is an important consideration for successful outcomes in mesenchymal stromal cell therapies and the common sources include bone marrow, adipose, synovial fluid, and synovium. According to the number of studies, bone marrow-derived MSCs (BM-MSCs) could be the predominant cell source, followed by adipose tissue-derived MSCs (AT-MSCs).
Exosome is a specific extracellular vesicle ranged from 30 to 150 nm diameter [28] with a density of between 1.1 and 1.2 g/mL [29], found in multiple types of cell [30] and extracellular fluids, such as plasma [31], synovial fluid [32], urine [33], amniotic fluid [34], saliva [35], cerebrospinal fluid [36], breast milk [37], and tears [38]. MSC-Exos transfer bioactive lipids, nucleic acids (DNA, mRNAs, and non-coding RNAs) [39], and proteins between cells to elicit biological responses (gene-regulation [40], proliferation, apoptosis [41], immunomodulation [42], and so on) in recipient cells [43]. Different MSC-Exos have heterogeneity, even extracellular RNA extracted from exosomes and non-vesicles derived by the same cell have heterogeneity [44].
Phenotypic analysis
Phenotypic analysis confirms the expression of various MSCs-related surface markers. Most MSCs are positive for cluster of differentiation (CD)73 (5'nucleotidase) [45–51], CD90 (Thy1 membrane glycoprotein) [48–54], CD105 (endoglin) [32, 50, 51, 55–57], CD44 (hyaluronan receptor) [48, 49, 58, 59], and lack expressions for CD34 (hematopoietic progenitor cell antigen) [32, 55, 56, 60, 61], CD14 (myeloid cell-specific leucine-rich glycoprotein) [60–63], CD45 (protein tyrosine-phosphatase) [64–68], and HLA-DR (human leukocyte antigens class II DR) [62, 68, 69]. Individual markers include CD146 (S-endo1, melanoma cell adhesion molecule, Muc18, or glycerin) [65–67, 70], CD29 (integrin β1) [45–47, 52, 53, 64–66], CD49e (integrin α5), CD54 (intercellular adhesion molecule 1), CD106 (vascular cell adhesion molecule) [63], CD146 (melanoma cell adhesion molecule) [32, 55, 56, 67, 70], CD166 (activated leukocyte cell adhesion molecule) [63, 67], CD271 (low-affinity nerve growth factor receptor) [32, 46, 47, 55, 56, 65–67], SSEA-4 (stage-specific embryonic antigen-4) [45], Notch 1 (neurogenic locus notch homologue protein 1), HLA-ABC (human leukocyte antigens, histocompatibility complex class I molecules) [71, 72], and Stro1 (stromal antigen 1) [68].
Besides CD44, CD73, CD90, CD105, some protein markers have the potentials to be new and specific markers [73]. Stro-1 and CD271 are cell membrane single-pass type I proteins that translocate from the endoplasmic reticulum to the cell membrane in response to the depletion of intracellular calcium. However, it is unclear whether Stro-1 expression correlates with multipotency [46]. SSEA-4 is an embryonic stem cell marker, and CD146 is detected on perivascular cells around venules [69]. Erdogan et al. reported that AT-MSCs in New Zealand rabbits did not express CD73 and CD90 [58], while Chen et al. detected the expression of CD90 [59]. Some markers appeared already at the optic vesicle stage but did not remain highly expressed in the later differentiation stage [74].
As for Exos, they are characterized by the expression of endosomal markers, including tetraspanins (CD9, CD63, CD81, and CD82) due to endosomal origin [32, 64, 68, 75–77], whereas TSG101 (tumor suppressor gene 101), an endosomal sorting complex required for transport-related protein specific for micro-vesicle body formation, is not specifically expressed in exosomes [32]. The common surface marker profile of MSCs and MSC-exosomes is shown in Table 1.
Table 1.
Surface markers on mesenchymal stromal cells and exosomes
| Species | Source | Positive antigens | Negative antigens | References |
|---|---|---|---|---|
| Human | Bone marrow | CD13, CD29, CD44, CD71, CD90, CD106, CD120a, CD124, CD271, CD146, Stro-1, SSEA-4 | CD14, CD34, CD45 | [65, 66] |
| Rabbit | Bone marrow | CD29, CD73, CD105, CD146 | CD34, CD45 | [45] |
| Rat | Bone marrow | CD29, CD44, CD90 | CD34, CD11, CD45 | [52, 53] |
| Mice | Bone marrow | Sca-1, CD29 | CD45, CD11b | [64, 65] |
| Human | Adipose | CD13, CD29, CD44, CD73, CD90, CD105, CD271, CD146 | CD31, CD34, CD45, Stro-1, SSEA-4 | [46, 47] |
| Rabbit | Adipose | CD29, CD44, α-SMA, CD90 | CD34, CD45 | [58, 59] |
| Rat | Adipose | CD44, CD73, CD90 | CD34, CD45, CD11b | [48, 49] |
| Mice | Adipose | CD29, CD105 | CD34, CD45 | [57] |
| Human | Synovial fluid/synovium | CD13, CD73, CD90, CD105, Stro-1, SSEA-4, CD146 | CD11b, CD14, CD19, CD34, CD45, CD79b, CD271, HLA-DR | [32, 55, 56] |
| Human | Blood | CD29, CD73, CD90, CD105, CD146, CD166 | CD45, Stro-1, SSEA-4, CD271 | [67] |
| Horse | Blood | CD73, CD90, CD105, CD146 | [70] | |
| Human | Term placenta | CD29, CD44, CD73, CD90, CD105, SSEA-4 | CD11b, CD14, CD19 CD31, CD34, CD45, Stro-1, HLA‐DR, CD271 | [60, 61] |
| Human | Amniotic fluid | CD73, CD90, CD105 | CD31, CD34, CD45 | [54] |
| Human | Umbilical cord | CD73, CD90, CD105 | CD11b, CD14, CD19, CD34, CD45, HLA-DR, CD271, SSEA-4 | [62] |
| Human | Trabecular bone | CD90, CD73, CD105, CD166, CD106, CD146 | CD14, CD19, CD34, CD45 | [63] |
| Human | BM-MSC-Exos | CD9, CD81, TSG101 | Calnexin | [68] |
| Rabbit | BM-MSC-Exos | CD9, HSP70 | [75] | |
| Rat | BM-MSC-Exos | CD63, CD81, TSG101 | Calnexin | [76] |
| Mice | BM-MSC-Exos | CD63, CD81, syntenin 1, TSG101 | [64, 77] | |
| Human | AT-MSC-Exos | CD9, CD63, CD73, CD81, CD90, CD146, TSG 101, HLA-ABC | Calnexin, CD45, HLA-DR | [68] |
| Human | SF-MSC-Exos | CD9, CD63, CD81, TSG101 | [32] | |
| Human | UC-MSC- Exos | CD63 | Calnexin | [62] |
MSCs Mesenchymal stromal cells, BM bone marrow, AT adipose tissue, UC umbilical cord, SF synovial fluid, Exos exosomes, CD cluster of differentiation, SSEA-4 stage-specific embryonic antigen-4, α-SMΑ α-smooth muscle actin, HLA human leukocyte antigen, TSG101 Recombinant Tumor Susceptibility Gene 101, HSP70 heat-shock protein 70
Culture
MSCs are spindle-shaped and adherent cells, capable of proliferation, self-renewal, and differentiating into cells of multi-lineage. One of the characteristic features of MSCs is adhering to tissue culture plastic and generating colonies when plated at low densities [78]. MSCs growing from individual foci, or colonies from the microscopic view, and these colonies generated from progenitor cells have been called the colony-forming unit fibroblast [79]. The ability of MSCs to undergo chondrogenic, osteogenic, and adipogenic differentiation has been reported in vitro and in vivo.
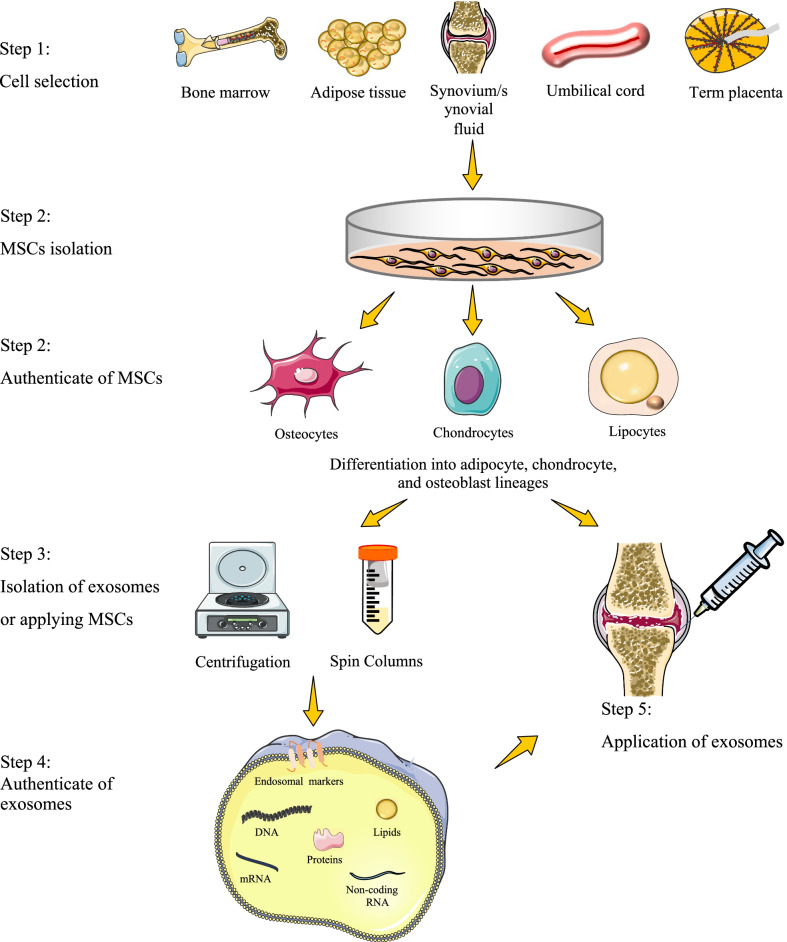
Chondrogenic differentiation largely depends on the culture conditions. Mediators capable of promoting chondrogenesis, such as transforming growth factor-beta (TGF-β), have been elucidated using simplified in vitro models [80]. Recently, Yin et al. indicated that MSCs differentiated into mature chondrocytes after 21 days of co-culture with ECM-derived particles in a microgravity environment without exogenous TGF-β3 [81]. Chondrogenesis can be achieved either in 2-dimensional or 3-dimensional culture systems in vitro. The 3-dimensional culture system facilitates greater cell contacts and interactions of cells with the ECM, allowing cells to adapt to their native morphology [82]. Moreover, the efficiency of chondrogenesis tends to be lower in the 2-dimensional culture system. The scaffold-free 3-dimensional cultures provide a high-density cell culture environment and are commonly classified as pellet or micromass culture systems [83]. In general, the induced cartilage was more similar to hyaline cartilage in the micromass culture technique, while the pellet culture is more useful for clinical applications [84]. Moreover, platelet-rich plasma (PRP), MSCs, and chondrocytes co-culture would favor chondrogenesis without hypertrophic and pathologic responses [85]. Chondrocytes cultured with MSC-Exos enhanced proliferation and chondrogenesis [86]. The flow diagram of applying MSC-based therapy is presented in Fig. 1.
Fig. 1.
The flow diagram of applying MSC-based therapy. Firstly, choose the appropriate origin of MSCs, then isolate MSCs from other cells, and authenticate them. Inject the MSCs or isolate MSCs-derived exosomes by centrifugation or other methods, and then inject the exosomes after authentication. MSCs: mesenchymal stromal cells
Functions of MSC-based therapy for cartilage regeneration in KOA
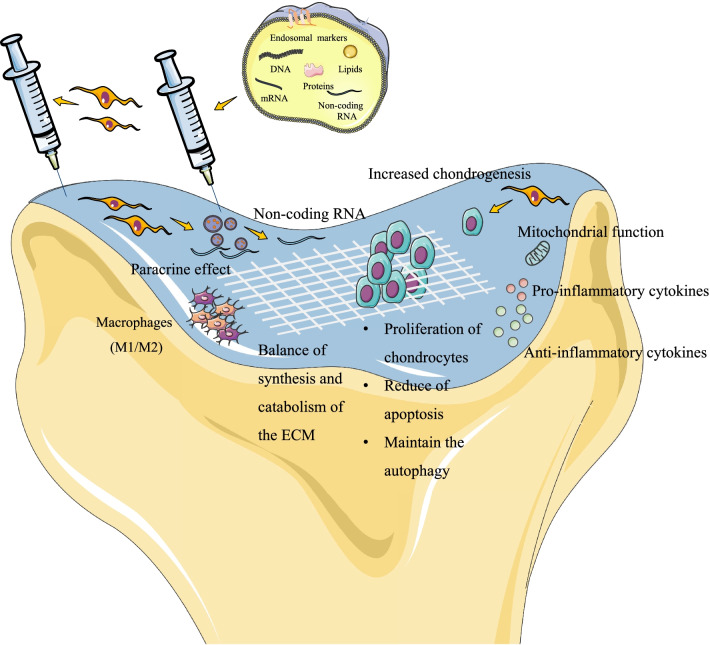
Impact on chondrocyte
Increased chondrogenesis, improved proliferation, reduced apoptosis, and maintenance of autophagy of chondrocytes are the main functions of MSC-based therapy on KOA. The chondrogenesis is primarily due to chondrogenic differentiation of MSCs triggered by some growth factors or enhanced activity of chondroprogenitors and chondrocytes stimulated by MSCs [87]. Moreover, human AT-MSCs showed a high chondrogenic potential supported by the increased expression of sex-determining region of Y chromosome-box transcription factor 9 (SOX9), as a chondrocyte precursor marker [88]. One study reported a reduced matrix synthesis and low proliferation rate of chondrocytes in the injured cartilage, while the restored proliferation ki67 enhanced after injecting human umbilical cord-derived MSCs [89]. Additionally, the proliferation rate of chondrocytes was increased while co-culturing with BM-MSCs [90]. In addition, synovial MSC-Exos have the potential to improve proliferation and migration of chondrocytes in vitro and in vivo [91]. TGF-β1-stimulated MSC-Exos increased the cell viability of the chondrocyte-restricted rat cell line [92]. Rat BM-MSC-Exos under hypoxic pretreatment promoted the proliferation and migration of chondrocytes [93].
Apoptosis of chondrocytes is another characteristic of the progression of OA. Chen et al. reported a notable decrease of the proportion of dUTP nick end labeling positive cells that indicated apoptosis in cartilage after injection with MSCs compared with the phosphate-buffered saline [94]. Apoptosis could be a potential therapeutic pathway for KOA [95]. Moreover, the apoptosis of chondrocytes was remarkably inhibited by coculturing with BM-MSCs under hypoxia [90]. Exos also have a positive effect on preventing cartilage damage. Interleukin (IL)-1β treatment inhibited cell viability and DNA synthesis activity, and enhanced apoptosis of chondrocytes. However, BM-MSC-Exos treatment promoted cell viability and DNA synthesis activity with a lower apoptosis rate [96]. Wu et al. also reported AT-MSC-Exos inhibited cell apoptosis and enhanced autophagy [97]. Autophagy can be detected combined with apoptosis in KOA. Autophagy serves as an adaptive response under environmental changes that maintain the survival of chondrocytes by preserving energy metabolism in cells. The levels of Beclin‐1 and microtubule‐associated protein light chain 3, as two vital proteins in the autophagic process, were detected to manifest a reduced autophagic activity in KOA animal model that treated with phosphate-buffered saline, whereas MSCs therapy maintained almost the same level as that of the normal group [94].
Impact on the ECM
Regulating the balance of synthesis and catabolism of the ECM is essential to treat degenerative diseases, such as KOA. Matrix metalloproteinases (MMPs) refer to a family of zinc-dependent ECM remodeling endopeptidases that degrade the ECM. On the other hand, the tissue inhibitors of MMPs (TIMPs) are important regulators of ECM turnover, tissue remodeling, and cellular behavior that inhibit the proteolytic activity of MMPs within the ECM. BM-MSCs balanced the ratio of MMP‐13 to TIMP‐1 in cartilage and reduced the expression of cartilage hypertrophic markers such as collagen (Col)-X, fibroblast growth factor receptors 1–3, parathyroid hormone-related protein, and MMP-13 [98]. Several studies reported the higher expression of gene Col 2α1 in KOA cartilage, which encoded the α-1 chain of Col II, after MSC-based therapy [24, 99]. Moreover, the expressions of a disintegrin and metalloproteinase with thrombospondin motifs-5 and MMP13 in cartilage were significantly downregulated after treating with human umbilical cord-derived MSCs [89]. Hyaluronan synthase-1 mRNA expression was upregulated in BM-MSCs after co-culture with chondrocytes from the KOA model, whereas hyaluronidase-1 was downregulated [100]. Chen et al. revealed that BM-MSC-Exos could promote the expression of Col II, SOX9, and aggrecan while negatively regulating the expression of chondrocyte hypertrophy markers MMP-13 in mouse models of post-traumatic KOA [101].
Impact on the inflammatory cytokines
Inflammatory response plays an important role in the pathogenesis of KOA. The most important groups controlling the disease seem to be pro-inflammatory cytokines and anti-inflammatory cytokines, which have an antagonistic effect. The former mainly includes IL-1β, tumor necrosis factor‐α (TNF‐α), IL-6, IL-15, IL-17, and IL-18. Another is formed by TNF-stimulated gene 6, IL-4, IL-10, IL-13, IL-37, and others. IL-37 partly rescued IL-1β and impaired cartilage formation of MSCs. This effect contributed to a lower MMP3 expression and an increased ratio of Col-II/ Col-I without increasing hypertrophy markers [102]. Pro-inflammatory (M1) macrophages are associated with a high production of pro-inflammatory mediators such as TNF-α, IL-6, IL-1β, and IL-12, and are required for T cell activation. These cytokines induce destructive processes in chondrocytes manifesting a lower expression of Col-II and aggrecan synthesis [103].
Some researchers found decreased expressions of inflammatory and catabolic markers including IL-1β, TNF-α, and MMP13, after AT-MSCs injection [104], BM-MSCs injection [105], or induced pluripotent stromal cell-chondrocytes transplant in KOA model. However, no difference in Col-II and Col-I expression was found between transplanted cartilage and other groups [106]. One study determined that both IL-1β and TNF-α immunostaining in chondrocytes in the cartilage were significantly enhanced after human umbilical cord-derived MSCs treatment and reserved almost back to normal tissue. Additionally, umbilical cord-derived MSCs therapy also led to increased expression of anti-inflammatory factors, TNF-stimulated gene 6, and IL-1 receptor antagonist, in the articular chondrocytes [89]. Human AT-MSCs seem to adapt and respond better to both inflammatory stimuli and autologous protein solution than BM-MSCs in vitro [107]. Co-culture with AT-MSCs counteracted the IL-1β-induced mRNA upregulation of the MMP-3, MMP-13, TNF- α, and IL-6 in chondrocytes. Importantly, AT-MSCs increased the expression of the anti-inflammatory cytokine IL-10 in chondrocytes [108, 109].
As for treatment with Exos, injection of miR-9-5p-contained Exos alleviated the inflammation in KOA, which was evidenced by downregulated levels of inflammatory factors and reduced oxidative stress injury [110]. Lu et al. reported synovial MSC-Exos enhanced IL-1β-induced cell proliferation, whereas inhibited apoptosis and inflammation and the target relationship of miR-26a-5p and phosphatase and tensin homologue were predicted and confirmed [111]. Moreover, Zhe et al. investigated miR-26a-5p in human BM-MSCs exerted an alleviatory effect on the damage of the synovial fibroblasts [112].
Impact on the immunity
Macrophages could play a crucial role in modulating inflammation during the pathogenesis of KOA via various secreted mediators. These cells can polarize to pro-inflammatory and anti-inflammatory (M2) phenotypes. One study exposed AT-MSCs to osteoarthritic synovial fluid for two days for determining the effect of their secretome on differentiation of monocytes into pro-inflammatory M1-like macrophages and mature dendritic cells, and the effect on T cell proliferation and expansion of T regulatory cells. The results suggest that the exposure of AT-MSCs upregulated the immunosuppressive factors that induce monocytes into the M2-like phenotype and inhibit differentiation of monocytes into mature dendritic cells. Only the secretome of exposed AT-MSCs was detected to inhibit proliferation of T cells and promote T regulatory cells expansion [113].
More than 240 micro-RNAs were found in AT-MSCs and accounted for most of the genetic message that protected chondrocytes and M2 macrophage polarizing. Ragni et al. [114] have confirmed an increased M2 phenotype marker CD163 and reduced the chondrocyte inflammation marker vascular cell adhesion molecule-1 on inflamed macrophages and chondrocytes. BM-MSCs-Exos and AT-MSCs-Exos have reported relieving KOA by promoting the phenotypic transformation of synovial macrophages from M1 to M2 [115, 116]. Moreover, TGF-β1-stimulated BM-MSC-Exos reduced pro-inflammatory factors by promoting M2 polarization of synovial macrophages [117].
Impact on the mitochondrial function
Aging and exposure to stress would determine the chondrocyte phenotype in osteoarthritis and age-related mitochondrial dysfunction and associated oxidative stress might induce senescence in chondrocytes [118]. The mitochondrial transfer was found from BM-MSCs to osteoarthritis chondrocytes. One study showed an increased mitochondrial membrane potential when co-cultured with mitochondria from MSCs compared with chondrocytes without mitochondria transfer. The activity of mitochondrial respiratory chain enzymes and the content of adenosine-triphosphates were significantly improved [119].
Impact on the paracrine effect
Some researchers thought the paracrine effect of MSCs was mediated or performed by MSC-derived extracellular vesicles, while others support the induction of paracrine effect was independent of extracellular vesicles [120]. In general, the paracrine effect and Exos both represent cell-to-cell contact and biological information delivery. Extracellular vesicles have been traditionally classified into four subtypes, mainly based on their origins and sizes. MSC-Exos, as the smallest extracellular vesicles, have recently been suggested as a mechanism for their therapeutic potentials [121]. Figure 2 shows the functions of MSC-based therapy.
Fig. 2.
The functions of injections of MSCs or MSCs-derived exosomes. MSCs can protect cartilage by differentiation into chondrocyte lineages, affecting the chondrocytes, mediating mitochondrial function, regulating cytokines, balancing the synthesis and catabolism of the extracellular matrix (ECM), modifying immune reactions, and paracrine activity that might be involved with the secreted exosomes. Exosomes are small extracellular vesicles that include lipids, nucleic acids, and proteins. MSCs: mesenchymal stromal cells, ECM: extracellular matrix
Mechanisms in cartilage regeneration by MSC-based cell therapy
Pathways or axis
Regulations of inflammation, immunoregulatory, and metabolic pathways and the expression of key molecules by the MSCs-based therapy have been revealed in recent research. The nuclear factor-kappaB (NF-κB) family plays crucial roles in various biological processes including mechanical processes, immunity, inflammation, and oxidative stress response, which could be activated by chemokines, pro-inflammatory cytokines, and degradation factors. NF-κB comprises five members: RelA (p65), c-Rel, RelB, NF-κB1 (p50), and NF-κB2 (p52) [122]. Yu et al. reported that the deletion of RelA in culturing BM-MSCs could increase the chondrogenic differentiation [123]. Treatment with human AT-MSCs significantly reduced the content of signal transducer and activator of transcription 3, which is a DNA-binding molecule that regulates the levels of many cytokines. Activation of signal transducer and activator of transcription 3 leads to increased pro-inflammatory cytokine production and immune responses [124]. BM-MSC-Exos inhibited mitochondrial-induced apoptosis in response to IL-1β, involving p38 mitogen-activated protein kinase (MAPK), extracellular regulated protein kinases (ERK), and protein kinase B pathways (AKT) [125].
Chronic inflammation may contribute to stress‐induced senescence of chondrocytes and cartilage degeneration during the progression. Treatment of chondrocytes with MSCs down‐regulated senescence markers induced by IL‐1β including senescence‐associated β‐galactosidase activity, accumulation of γH2AX foci, and morphological changes with enhanced formation of actin stress fibers. Additionally, the treatment reduced the activation of MAPK, ERK1/2, and p38 and to a lower extent the phosphorylation of c-jun N-terminal kinase 1/2 [126], which represents a classical inflammatory pathway. Besides this, inflammation is a prerequisite for the protective effect of AT-MSCs. Van Dalen et al. proved that local application of AT-MSCs in KOA joints led to rapid clustering of polymorphonuclear cells around AT-MSCs, while IL-1β stimulated this clustering which reduces the pro-inflammatory activity of the polymorphonuclear cells in vitro [127].
In human chondrocytes, oxidative stress may lead to DNA damage and senescence. In addition, reactive oxygen species (ROS) production is important in signaling pathways activated by IL-1β in chondrocytes. As oxidative stress is a key process in the induction and maintenance of senescence, Platas et al. investigated the effects of AT-MSCs on protein modification by ROS. In chondrocytes from the KOA model, IL-1β quickly induced the production of ROS and enhanced levels of 4-hydroxy-2-nominal-modified proteins, whereas AT-MSCs reduced the level of them [126]. In addition, human AT-MEC-Exos reduced the production of oxidative stress in OA chondrocytes stimulated with IL-1β and resulted in an upregulation of peroxiredoxin 6 [128].
Cell proliferation activated by AT-MSCs in KOA rabbits may be specifically regulating the glycogen synthase kinase-3β (GSK-3β)/cyclin D1/cyclin-dependent kinase (CDK)4/CDK6 pathway. It reduced the elevated serum level of cartilage oligomeric matrix protein, blocked increases in the mRNA, and protein expression of GSK3β while decreasing the mRNA and protein expression of cyclin D1/CDK4 and cyclin D1/CDK6 in cartilage [129]. Wu et al. demonstrated BM-MSCs increased the levels of the ECM proteins Col-II and SOX9 and decreased chondrocyte apoptosis and inflammation by upregulating the mediators of the autophagy phosphatidylinositol 3 kinase/AKT/mammalian target of rapamycin (mTOR) pathway [130].
Key transcription factors
Key factors included TGFBI/BIGH3 (TGF-β-induced gene product-h3), bone morphogenetic proteins (BMPs), Nanog, and Oct4, which have important functions in cell adhesion, migration, proliferation, and apoptosis. TGFBI is a chondroprotective factor, released by MSCs and an anabolic regulator of cartilage homeostasis. Priming with TGFβ3 upregulated TGFBI transcription in murine MSCs and human MSCs and increased TGFBI secretion in human MSCs. Moreover, incubation of osteoarthritis-like mouse chondrocytes with TGFβ3-primed murine MSC-conditioned media significantly upregulated the expression of chondrocyte anabolic markers but did not change the expression of catabolic and inflammatory factors [131]. BMPs are a subfamily of the TGF-β superfamily that participate in the induction of bone and cartilage formation. BMP6 enhanced chondrogenesis of MSCs [132]. As key transcription factors for pluripotency and self-renewal, the overexpression of Nanog and Oct4 also enhanced chondrogenic reported that cell therapy by using MSCs after neurogenic differentiation and maintained MSCs properties in various culture conditions [133]. Stromal cell-derived factor-1α has been detected to promote stem cell migration and homing [134].
Non-coding RNAs
Non-coding RNAs are functionally complex and are implicated in many crucial biochemical and cellular processes such as cell communication, inflammation, exosome biogenesis, tissue repair, regeneration, and metabolism. This wide distribution of biological activities confers on MSC-Exos the potential to elicit diverse cellular responses and interact with many cell types. MiR-410 is a key regulator of MSC chondrogenic differentiation and directly targets Wnt3a triggering the Wnt signaling pathway [135]. Moreover, miR-127-3p from BM-MSCs inhibited cadherin-11 in chondrocytes, thereby blocking the Wnt/β-catenin pathway [96]. The miR-155-5p in synovial fluid-derived MSC-Exos promoted proliferation and migration, suppressed apoptosis, and enhanced ECM secretion of osteoarthritic chondrocytes. Further, overexpression of Runt-related transcription factor 2 partially reversed the effect of the synovium-derived MSC-155-5p-Exos on osteoarthritic chondrocytes [136]. MiR-135b promoted M2 polarization of synovial macrophages through targeting MAPK6 [117]. Additionally, miR-361-5p was verified to inhibit the NF-κB signaling pathway [137]. Synovium-derived MSC-extracellular vesicle-encapsulated miR-31 ameliorates KOA via the lysine-specific demethylase 2A/E2F transcription factor 1/pituitary tumor transforming gene 1 axis [91]. The upregulation of miR-143 and miR-124 in cellular and mouse OA models treated with Exos remarkably restored the normal expression of NF-κB and Rho Kinase 1 pathways [138]. Human AT-MSCs-Exos inhibited cell apoptosis, enhanced matrix synthesis, and reduced the expression of catabolic factors via the mTOR signaling pathway. MiR-100-5p decreased the luciferase activity of the mTOR 3′-untranslated region [97]. Hu et al. revealed that miR-365 expression was activated by chondrogenic induction in both MSCs from the osteoarthritis model and BM-MSCs [139]. Additionally, some micro-RNAs protect the cartilage, such as miR-26a-5p targeting phosphatase and tensin homolog, miR-26a-5p targeting prostaglandin-endoperoxide synthase 2 [111, 112], miR-136-5p targeting E74-like factor 3 [101], and miR-520d-5p targeting histone deacetylase 4 [140]. Most reported non-coding RNAs were detected in the Exos, and detailed mechanisms are presented in Table 2.
Table 2.
Mechanisms of non-coding RNA in mesenchymal stromal cell-based therapy for knee osteoarthritis
| Source | Target | Amount | Axis/signaling pathway | Function | References |
|---|---|---|---|---|---|
| Human AT-MSCs | In vitro | 400 µg/mL | miR-145 and miR-221 | Downregulated the expression of pro-inflammatory markers IL-6, NF-κB, and TNF-α, while upregulated the expression of the anti‐inflammatory cytokine IL‐10 | [109] |
| Human OA cartilage-derived MSCs and BM-MSCs | Mice | NR | miR-365 | Activation of aggrecan and collagen type 2a1 gene expression. MiR-365 expression was activated by chondrogenic induction in both OA-MSCs and BM-MSCs | [139] |
| Human BM-MSCs-Exos | In vitro | NR | miR-520d-5p/HDAC1 | MiR-520d-5p promoted MSCs chondrogenesis and regulates chondrocyte metabolism through targeting HDAC1 | [140] |
| Human BM-MSCs | In vitro | NR | miR-410/Wnt3a | MiR-410 was elevated during TGF-β3-induced chondrogenic differentiation of MSCs, and regulated the Wnt signaling pathway | [135] |
| Rat BM-MSCs-Exos | Rat | NR | miR-9-5p/syndecan 1 | Anti-inflammatory and chondroprotective effects of BM-MSC-derived exosomal miR-9-5p on KOA via regulation of syndecan 1 | [110] |
| Human BM-MSCs-Exos | Rat | 250 ng/5 µL | miR-26a-5p/Cox2 | Human BM-MSC-Exos overexpressing miR-26a-5p serve as a repressor for damage of synovial fibroblasts via Cox2 in KOA | [112] |
| Human SMSCs-Exos | Rat | 30 µL, 1011 particles/mL | miR-26a-5p/PTEN/IL-1β | SMSC-exos enhanced IL-1β-induced cell proliferation, whereas inhibited apoptosis and inflammation. MiR-26a-5p targeted PTEN, for which overexpression spoiled the protection of exosomes against IL-1β-induced cell damage | [111] |
| SMSCs-Exos | Mice | 5 µL | miR-31/KDM2A/E2F1/PTTG1 | SMSC-Exos and Exos from miR-31-overexpressed SMSCs alleviated cartilage damage and inflammation in KOA in vivo | [91] |
| Human AT-MSCs-Exos | Mice | 10 µL, 1010 particles/mL | miR-100-5p/mTOR | The level of miR-100-5p decreased the luciferase activity of mTOR 3′UTR, while inhibition of miR-100-5p could reverse the MSC-Exos-decreased mTOR signaling pathway | [97] |
| Rat BM-MSCs-Exos | Nude mice | 20 µg | miR-127-3p/ CDH11/Wnt/β-catenin | MiR-127-3p targeted CDH11 and over-expressed CDH11 in chondrocytes weakened the therapeutic effect of exosomes. IL-1β treatment resulted in the activation of the Wnt/β-catenin pathway in chondrocytes | [96] |
| Rat BM-MSCs-Exos | Rat | 100 µL, 1011 particles/mL | miR-135b/MAPK6 | MiR-135b promoted M2 polarization of synovial macrophages through targeting MAPK6 | [117] |
| Rat MSCs-Exos | Rat | 100 µL, 1011 particles/mL | miR-135b/Sp1/TGF-β1 | TGF-β1 stimulation enhanced miR-135b expression in MSC-exosomes, and MSC-exosomes-derived miR-135b increased the cell viability of C5.18 cells via downregulated Sp1 expression | [92] |
| Human BM-MSCs-Exos | Mice | 100 µL, 1011 particles/mL | miRNA-136-5p/ELF3 | An increased ELF3 expression and reduced miR-136-5p expression were detected in the clinical samples of traumatic OA cartilage tissues. BM-MSC-derived exosomal miR-136-5p could promote chondrocyte migration in vitro and inhibit cartilage degeneration in vivo | [101] |
| Human AT-MSCs-Exos | Mice | NR | miR-124/NF-κB and miR-143/ ROCK1/TLR9 | MiR-143 and miR-124 inhibited the expression of NF-κB and ROCK1 in OA cells. In addition, the 3’ UTRs of NF-κB and ROCK1 were proven to contain the binding sites for miR-143 and miR-124, respectively | [138] |
| Rat BM-MSCs-Exos | Rat | 200 µg | miR-216a-5p/JAK2/STAT3 | Hypoxic-Exos promoted the proliferation and migration of chondrocytes and inhibited their apoptosis by targeting functional miR-216a-5p to chondrocytes and then downregulating JAK2. In addition, HIF-1α induces hypoxic BM-MSCs to release Exos | [93] |
| Human BM-MSCs-Exos | Rat | 2 µg | miR-361-5p/DDX20/NF-κB | MiR-361-5p was verified to directly target DDX20. Additionally, human BM-MSC-Exos-transferred miR-361-5p alleviates chondrocyte damage and inhibits the NF-κB signaling pathway | [137] |
| Human SMSCs-Exos | BALB/C mouse | 30 µL, 1011 particles/mL | miR-155-5p/Runx2 | The SMSC-155-5p-Exos prevented KOA. Overexpression of Runx2 partially reversed the effect of the SMSC-155-5p-Exos | [136] |
| MSCs-Exos | In vitro, co-culture with mouse chondrocytes | NR | circRNA_HIPK3/miR-124-3p/MYH9 | MSCs-Exos overexpressing circHIPK3 improved IL-1β-induced chondrocyte injury. Mechanistically, circHIPK3 could directly bind to miR-124-3p and subsequently elevate the expression of the target gene MYH9 | [143] |
| Human MSCs | In vitro | NR | lncRNA HOTAIRM1-1/miR-125b/ BMPR2; JNK/MAPK/ERK pathway | HOTAIRM1-1 was downregulated in KOA cartilages and may inhibit MSCs viability, induce apoptosis, and suppress differentiation via regulating miR-125b/BMPR2 axis JNK/MAPK/ERK pathway may be a possible downstream mechanism to mediate the role of HOTAIRM1-1 in OA development | [146] |
| Human BM-MSCs-Exos | In vitro | NR | lncRNA HOTTIP/miR-455-3p/CCL3 | HOTTIP negatively regulated miR-455-3p and increased CCL3 levels in human chondrocytes | [147] |
| Human AT-MSCs | In vitro | NR | circRNA_ATRNL1/miR‐145‐5p/SOX9 | Circ_ATRNL1 regulated the promotion of SOX9 expression to promote chondrogenic differentiation of human AT-MSCs mediated by miR‐145‐5p | [141] |
| Human BM-MSCs-Exos | Mice | 10 µL, 500 µg/mL | circRNA_0001236/miR-3677-3p/Sox9 | Exosomal circRNA_0001236 enhanced the expression of Col2α1 and SOX9, but inhibited MMP13 in chondrogenesis via targeting miR-3677-3p and Sox9 | [142] |
| Human BM-MSCs | In vitro | NR | lncRNA GRASLND | Silencing of lncRNA GRASLND resulted in lower accumulation of cartilage-like extracellular matrix, while GRASLND overexpression significantly enhanced cartilage matrix production | [144] |
| Human SMSCs | In vitro | NR | lncRNA MEG3/EZH2-mediated H3K27me3/TRIB2 | LncRNA MEG3 regulated chondrogenic differentiation by inhibiting TRIB2 expression through EZH2-mediated H3K27me3 | [145] |
| Human and mouse MSCs | In vitro | NR | lncRNA EPB41L4A‐AS1 and lncRNA SNHG7/miR‐146a | MiR‐146a significantly inhibited BM-MSCs proliferation partly interacting with lncRNA EPB41L4A‐AS1 and lncRNA SNHG7 | [148] |
| Human BM-MSCs-Exos | In vitro | NR | lncRNA LYRM4-AS1/GRPR/miR-6515-5p | IL-1β significantly decreased cell viability, promoted apoptosis, and upregulated the expression of MMP3, AKT, and GRPR, while Exos reversed the changes | [149] |
OA Osteoarthritis, KOA knee osteoarthritis, MSCs mesenchymal stromal cells, BM bone marrow, AT adipose tissue, Exos exosomes, NR not reported, IL interleukin, NF-κB nuclear factor-kappaB, TNF-α tumor necrosis factor-α, TGF-β transforming growth factor-β, UTR untranslated regions of mRNA, CDH11 cadherin-11, SMSCs synovial-derived mesenchymal stromal cells, Runx2 Runt-related transcription factor 2, MAPK mitogen-activated protein kinases, DDX20 Asp-Glu-Ala-Asp (DEAD)-box polypeptide 20, ROCK1 Rho-associated kinase 1, TLR9 Toll-like receptor 9, mTOR mechanistic target of rapamycin, JAK2 Janus kinase 2, STAT3 signal transducer and activator of transcription 3, PTEN phosphatase and tensin homolog, HDAC1 histone deacetylase 1, Cox2 cyclooxygenase-2, ELF3 E74-like factor 3, SOX9 sex-determining region of Y chromosome-box transcription factor 9, Col2α1 α-1 chain of procollagen type 2, MMP matrix metalloproteinase, MYH9 myosin heavy chain 9, TRIB2 tribbles homolog 2, BMPR2 bone morphogenetic protein receptor 2, JNK p38 and c-jun N-terminal kinase, ERK extracellular signal-regulated kinase, CCL3 macrophage inflammatory protein 1-α, AKT protein kinase B, GRPR gastrin-releasing peptide receptor
Moreover, circle-RNAs and long non-coding RNAs play vital roles in micro-RNAs interaction and show abnormal expression in osteoarthritis, which may be an important target for regulating osteoarthritis and for drug treatment. These RNAs regulate the progress of KOA by completing with micro-RNAs or other non-coding RNAs, that is called the ceRNA regulatory network, such as circRNA_ATRNL1 targeting miR‐145‐5p [141], circRNA_0001236 targeting miR-3677-3p [142], circRNA_HIPK3 targeting miR-124-3p [143], lncRNA GRASLND [144], lncRNA MEG3 targeting EZH2-mediated H3K27me3 [145], lncRNA HOTAIRM1-1 targeting miR-125b [146], lncRNA HOTTIP targeting miR-455-3p [147], lncRNA EPB41L4A‐AS1 and lncRNA SNHG7 targeting miR‐146a [148], and lncRNA LYRM4-AS1 targeting miR-6515-5p [149].
The physical situation on MSC-based cells
The external physical situation could affect the cartilage and MSCs phenotype, such as conditions with hypoxia, hydrostatic pressure, compression, or magnetic fields. Nonetheless, the standard culture systems of the external physical situation have not been well-established yet and mechanisms are unclear.
Several studies have determined the application of low oxygen tension or hypoxia in MSC chondrogenesis and culture. In the presence of IL-1β, a significant in glycosaminoglycan, as a measure of proteoglycan levels, collagen, and water content, was observed under hypoxic condition (2% O2, 5% CO2, 93% N2) [150]. Moreover, the mRNA expression of Col-II and aggrecan was upregulated in chondrocytes co-cultured with BM-MSCs under hypoxia (5% CO2 and 95% N2), and DNA methylation of the SOX9 promoter was significantly decreased under hypoxia [90]. Low oxygen tension (5%) was observed to promote ECM production by chondrocytes and enhanced the chondrogenesis of AT-MSCs compared to that cultured in normal condition [151]. Grayson and colleagues showed that under a 2% O2 hypoxia, the expression of stromal cell genes Oct-4 and Rex-1 was upregulated [152].
Magnetic fields have been reported to enhance the chondrogenic differentiation of MSCs. Pulsed electromagnetic fields drastically promoted chondrogenesis by a specific hydrogel with high expressions of Col-II, aggrecan, and SOX9 genes [153]. Besides pulsed electromagnetic fields, a static magnetic field with 0.4 T was demonstrated to produce a strong chondrogenic differentiation response after 14 days of culturing through the TGF-β pathway [154]. Further, the presence of electromagnetic fields could partly replace the addition of TGF-β3, while the efficacy of chondrogenesis was statistically increased in the culture system. In TGF-β3-treated pellets, a further significant increase of 72.7% in aggrecan gene expression was induced by electromagnetic fields at 5 weeks [155].
Ultrasound-targeted microbubble destruction has been confirmed to increase the homing of transplanted MSCs to targeted organs. Stromal cell-derived factor-1α, as an important role in BM-MSCs migration, was loaded in microbubble. The number of migrated cells was higher when loaded microbubble under the guidance of ultrasound that the ultrasonic irradiation conditions of duty ratio 10%, intensity 1 W/cm2, time 30 s [134].
Clinical application
The initial injection of MSC-based therapy was in 2008 [156], and a total of 23 non-case report studies are reported to apply MSC-based therapy for KOA since then. Thirteen of them were designed as randomized controlled studies, although with heterogeneity in sources cell, preparation methods, and dosage of MSCs. No study using MSC-Exos in KOA has been revealed yet. BM was the most frequently used source of MSCs (13/23 studies; 57%) [157–169], AT was used in 7 trials (30%) [18, 19, 170–174], and umbilical cord was used in two in two trial (9%) [15, 175], and one study used MSCs from placenta (4%) [176]. In 12 trials in phase I, the different dosages were compared. The control interventions in the rest trials were hyaluronic acid injection in five trials [15, 157, 160, 163, 175], PRP injection in four trials [161, 167, 168, 172], saline injection in four trials [19, 163, 164, 176], total knee arthroplasty in one study [162], and conservational treatment [18]. Combined therapy included total knee arthroplasty [162], PRP [161], PRP with arthroscopic debridement [172], and hyaluronic acid [160]. Most included individuals had grade II–III of Kellgren-Lawrence. Table 3 summarizes the study characteristics.
Table 3.
Characteristics of clinical trials about mesenchymal stromal cell-based therapy for cartilage regeneration in knee osteoarthritis
| Design | Sample size | Source | Dosage (cells) | Control intervention | Phase of trial | K-L grade | Outcomes | Follow-up | References |
|---|---|---|---|---|---|---|---|---|---|
| RCT | 30 | BM-MSCs | 4 × 107 | HA | II | II-IV | MRI, WOMAC, VAS, Lequesne index | 12 months | [157] |
| RCT and observational study | 18 | AT-MSCs | 1, 2, 5 × 107 | None | I/IIa | > II | AE, WOMAC, NRS, SF- 36, MRI | 24 months | [170] |
| Observational study | 15 | BM-MSCs | 4 × 107 | None | I/II | II-III | AE, WOMAC, VAS, Lequesne index SF- 36, MRI | 12 months | [158] |
| Observational study | 18 | AT-MSCs | 2, 10, 50 × 106 | None | I | III-IV | AE, WOMAC, VAS, KOOS | 6 months | [171] |
| Observational study | 12 | BM-MSCs | 4 × 107 | None | II | II-IV | MRI, WOMAC, VAS, SF-36 | 12 months | [159] |
| RCT | 26 | UC-MSCs | 2 × 107 | HA | I/II | I-III | MRI, WOMAC | 12 months | [15] |
| RCT | 24 | AT-MSCs | 1 × 108 | Saline | IIb | II-IV | MRI, WOMAC, KOOS | 6 months | [19] |
| RCT | 30 | BM-MSCs | 1, 10 × 107 | HA | I/II | > II | MRI, WOMAC, VAS | 12 months | [160] |
| RCT | 60 | BM-MSCs | 1 × 108 | PRP | II | > II | MRI, WOMAC, VAS | 12 months | [161] |
| Observational study | 25 | AT-MSCs | 1.89 × 106 | PRP, arthroscopic debridement | II | I-III | Lysholm, Tegner activity scale, VAS | 16 months | [172] |
| RCT | 20 | Placenta-derived MSCs | 5–6 × 107 | Saline | II | II-IV | VAS, KOOS, ROM, MRI | 6 months | [176] |
| Observational study | 18 | AT-MSCs | 1, 5, 10 × 107 | None | I/II | > II | WOMAC, MRI, arthroscopy | 6 months | [173] |
| RCT | 140 | BM-MSCs | 1.56 × 104 | TKA | III | II-IV | Radiographs, MRI | 15 years | [162] |
| RCT | 60 | BM-MSCs | 25, 50, 75, 150 × 106 | HA | I/II | II-III | WOMAC, VAS | 12 months | [163] |
| RCT | 30 | AT-MSCs | 1 × 108 | Conservative management | II | II-III | AE, MRI, KOOS, WOMAC, NRS | 12 months | [18] |
| RCT | 43 | BM-MSCs | 4 × 107 | Saline | I/II | II-IV | VAS, WOMAC | 6 months | [164] |
| Observational study | 29 | UC-MSCs | 1 × 107 | HA | II | I-II | WOMAC | 6 months | [175] |
| Observational study | 4 | BM-MSCs | 8–9 × 106 | None | I | NR | VAS, X-ray, activities | 12 months | [165] |
| Observational study | 12 | AT-MSCs | 5 × 107 | None | I | NR | AE, MRI | 12 months | [174] |
| Observational study | 12 | BM-MSCs | 1, 10, 50 × 106 | None | I/IIa | III-IV | ROM, KOOS, WOMAC, MRI | 12 months | [166] |
| RCT | 18 | BM-MSCs | NR | PRP | II | II-IV | KOOS, ROM | 12 months | [167] |
| RCT | 57 | BM-MSCs | NR | PRP | II | II-IV | KOOS, ROM | 12 months | [168] |
| Observational study | 12 | BM-MSCs | 6 × 107 | None | I | II-III | AE, KOOS, MRI | 24 months | [169] |
RCT Randomized controlled trial, MSCs mesenchymal stromal cells, BM bone marrow, AT adipose tissue, NR not reported, AE adverse event, NRS numerical pain rating scale, VAS visual analog scale, WOMAC Western Ontario and McMaster Universities Osteoarthritis Index, SF-36 short-form 36 health survey questionnaire, KOOS Knee Injury and Osteoarthritis Outcome Score, MRI magnetic resonance imaging, TKA total knee arthroplasty, HA hyaluronic acid, PRP platelet-rich plasma, K-L Kellgren-Lawrence
Dosage of MSCs
The single injection dosage ranged from 1.56 × 104 to 1 × 108 cells, and the most wildly proved dosage was 5 × 107 cells. Repeated injections or high dosage showed superiority than single injection or low dosage. Matas et al. clarified that repeated umbilical cord-derived MSCs (2 × 107 cells, every half year) treatment showed better improvements in pain and function than receiving injection only once at 1-year follow-up for individuals with KOA [15]. Moreover, Lamo-Espinosa et al. reported a high dosage with 1 × 108 BM-MSCs together with hyaluronic acid resulted in a larger clinical and functional improvement [160]. In addition, Chahal et al. found lower cartilage catabolic biomarkers and MRI synovitis in participants with higher doses [166] and the effects were maintained until 2-year follow-up [177].
Safety of MSC-based therapy
In general, MSC-based therapy is safe with mild adverse events. The most common adverse events were transient arthralgia, swelling of joints after local injection [171], and low back pain [158], which were mild to moderate and were usually spontaneously relieved within 7 days without special treatment or controlled with ibuprofen [159]. Song et al. reported one patient experienced mild edema and cramps of bilateral lower extremities that were relieved in 21 days without treatment [170]. Pers et al. demonstrated one severe adverse event that one patient with hypertension and hyperlipidemia experienced unstable angina pectoris without creased cardiac markers 3 months after AT-MSCs injection [171]. Adverse events were predominant in the high doses (> 5 × 107 cells) [163].
Effects on structure, pain, activities, and quality of living
Intra-articular injections of MSCs improved structure, pain, the function of the knee joint, rendering them a promising novel treatment for KOA. Besides these, this therapy had potential in activities, such as climbing the stairs and walking, and inflammatory factors. These benefits may last for several years, even be more apparent after months. Orozco et al. demonstrated an average 27% decrease of poor cartilage areas in severe KOA [159]. For MSCs-treated patients, Vega et al. [157] and Dilogo et al. [175] reported cartilage quality improvements that were quantified by T2 relaxation measurements. Although Lee et al. thought there was no improvement of cartilage at 6 months in the MSCs group, whereas the defect in the control group was increased [19]. Radiological, arthroscopic, and histological measures consistently demonstrated decreased deterioration by regeneration of hyaline-like articular cartilage [173]. For pain and function, Soler et al. [158] revealed a relevant pain relief since day 8 and maintained after one year. Khalifeh et al. clarified improvement in range of motion of the knee joint after MSCs injection was significant between the 2-week and 24-week follow-up [176]. The walking time without pain improved [165]. Although knees deteriorate gradually, they were still better than at baseline at 5 years [178]. Pro-inflammatory monocytes/macrophages [166] and IL-10/12 levels [168] decreased in the synovial fluid after MSCs injection.
Compared with ongoing conventional conservative management, AT-MSCs showed clinically significant pain and functional improvement after one year [18]. Moreover, greater improvements in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) total score, WOMAC pain, and physical function were recorded than saline [164]. There were greater improvements in the pain, function, daily living activities, and sports and recreational activities subscales in people receiving MSCs therapy than PRP, although less than the combination of two therapies [167].
Future directions
Based on the current application states, different cell sources have been clarified in the clinic by phase I/II studies, while no MSC-Exos are used. Therefore, a standard for MSCs therapy in KOA is required, which includes cell selection, authentication (phenotypic analysis and multipotent differentiation potential, especially distinguish with progenitor cells), culture or expansion methods, dosages, and rehabilitation program after injection. Second, Exos are good cargo and have potential in clinic application. The contained specific non-coding RNAs are important and may have an essential influence on the therapeutic effects. LncRNAs and circRNAs in Exos and the safety and doses of Exos need large research, which will be the aim of future clinical trials. Third, previous researchers have focused on the influence of physical situations on MSCs, while the mechanisms are still unclear. In addition, no study reported the changes of MSCs-Exos, RNA, or DNA sequence after physical exposure, which might be an unexpected trend. Although we merely discuss biological materials in MSC-based therapy, scaffold-assisted grafts or complex 3D hybrid tissues of MSCs or Exos with or without electromagnetic fields are interesting trends for severe KOA. At last, besides cartilage regeneration, functional subchondral bone regeneration also has a significant impact on KOA treatment.
Conclusions
MSCs and MSC-exosomes, as new therapeutic methods for KOA, showed unique advantages. The selection of different origins of MSCs may be inconsistent based on the research goal and the phenotype exhibits various characteristics. MSCs and the derived exosomes carried out various functions in the treatment of KOA which include of increase of chondrogenesis, proliferation of chondrocyte, reduction of apoptosis, maintenance of autophagy, regulation synthesis and catabolism of the ECM, regulation of immune response, inhibition of inflammation, monitoring the mitochondrial dysfunction, and the paracrine effect. These functions were partly demonstrated through several biological pathways or axis, such as NF-κB, MAPK, ROS, and mTOR pathways. Exosomes are primary mediators of intercellular communications especially by transferring non-coding RNAs to adjacent cells or remote cells. Different physical conditions (hypoxia, magnetic fields, and ultrasound) have been studied to enhance the functions in MSC-based therapy experiments. This review has presented the evidence for MSC-based therapy as a new approach to the cell-free treatment of KOA. However, a standard for MSC-based therapy in KOA is required.
Acknowledgements
Not applicable.
Abbreviations
- KOA
Knee osteoarthritis
- ECM
Extracellular matrix
- MSCs
Mesenchymal stromal cells
- Exos
Exosomes
- BM
Bone marrow
- AT
Adipose tissue
- CD
Cluster of differentiation
- TGF-β
Transforming growth factor-beta
- SOX9
Sex-determining region of Y chromosome-box transcription factor 9
- TLR
Toll‐like receptor
- TNF‐α
Tumor necrosis factor‐α
- MMPs
Matrix metalloproteinases
- TIMPs
Tissue inhibitors of MMPs
- Col
Collagen
- IL
Interleukin
- NF-κB
Nuclear factor-kappaB
- MAPK
Mitogen-activated protein kinase
- ERK
Extracellular regulated protein kinases
- AKT
Protein kinase B pathways
- ROS
Reactive oxygen species
- GSK-3β
Glycogen synthase kinase-3β
- CDK
Cyclin-dependent kinase
- TGFBI/BIGH3
TGF-β-induced gene product-h3
- BMPs
Bone morphogenetic proteins
- WOMAC
Western Ontario and McMaster Universities Osteoarthritis Index
- PRP
Platelet-rich plasma
Authors' contributions
All authors contributed to the conception and the main idea of the work. XNX drafted the main text, figures, and tables. SYZ revised the manuscript and drafted the figures. HCH, XY, and YX reviewed and revised the text. CQH supervised the work and provided comments and additional scientific information. All authors read and approved the final version of the work to be published.
Funding
This research study was supported by the National Natural Science Foundation (81972146, 82002393), the Department of Science and Technology of Sichuan Province (21YFS0004, 2021YJ0424), China Postdoctoral Science Foundation (2020M673251), Health Commission of Sichuan Province (20PJ034), West China Hospital of Sichuan University (ZYGD18018, 2019HXBH058).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declared that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiao-Na Xiang and Si-Yi Zhu contributed equally to this work
References
- 1.Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–1759. doi: 10.1016/S0140-6736(19)30417-9. [DOI] [PubMed] [Google Scholar]
- 2.Safiri S, Kolahi AA, Smith E, Hill C, Bettampadi D, Mansournia MA, Hoy D, Ashrafi-Asgarabad A, Sepidarkish M, Almasi-Hashiani A, et al. Global, regional and national burden of osteoarthritis 1990–2017: a systematic analysis of the global burden of disease study 2017. Ann Rheum Dis. 2020;79(6):819–828. doi: 10.1136/annrheumdis-2019-216515. [DOI] [PubMed] [Google Scholar]
- 3.Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulkader RS, Abdulle AM, Abebo TA, Abera SF, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, Callahan L, Copenhaver C, Dodge C, Felson D, et al. 2019 American college of rheumatology/arthritis foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2020;72(2):149–162. doi: 10.1002/acr.24131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Musumeci G, Aiello FC, Szychlinska MA, Di Rosa M, Castrogiovanni P, Mobasheri A. Osteoarthritis in the XXIst century: risk factors and behaviours that influence disease onset and progression. Int J Mol Sci. 2015;16(3):6093–6112. doi: 10.3390/ijms16036093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobson GP, Letson HL, Grant A, McEwen P, Hazratwala K, Wilkinson M, Morris JL. Defining the osteoarthritis patient: back to the future. Osteoarthr Cartil. 2018;26(8):1003–1007. doi: 10.1016/j.joca.2018.04.018. [DOI] [PubMed] [Google Scholar]
- 7.Murphy C, Withrow J, Hunter M, Liu Y, Tang YL, Fulzele S, Hamrick MW. Emerging role of extracellular vesicles in musculoskeletal diseases. Mol Aspects Med. 2018;60:123–128. doi: 10.1016/j.mam.2017.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li J, Pei M. Cell senescence: a challenge in cartilage engineering and regeneration. Tissue Eng Part B Rev. 2012;18(4):270–287. doi: 10.1089/ten.TEB.2011.0583. [DOI] [PubMed] [Google Scholar]
- 9.Guilak F, Nims RJ, Dicks A, Wu CL, Meulenbelt I. Osteoarthritis as a disease of the cartilage pericellular matrix. Matrix Biol. 2018;71–72:40–50. doi: 10.1016/j.matbio.2018.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tu J, Huang W, Zhang W, Mei J, Yu Z, Zhu C. TWIST1-MicroRNA-10a-MAP3K7 axis ameliorates synovitis of osteoarthritis in fibroblast-like synoviocytes. Mol Ther Nucleic Acids. 2020;22:1107–1120. doi: 10.1016/j.omtn.2020.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rahmati M, Nalesso G, Mobasheri A, Mozafari M. Aging and osteoarthritis: Central role of the extracellular matrix. Ageing Res Rev. 2017;40:20–30. doi: 10.1016/j.arr.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Hunziker EB, Quinn TM, Hauselmann HJ. Quantitative structural organization of normal adult human articular cartilage. Osteoarthr Cartil. 2002;10(7):564–572. doi: 10.1053/joca.2002.0814. [DOI] [PubMed] [Google Scholar]
- 13.Glyn-Jones S, Palmer AJ, Agricola R, Price AJ, Vincent TL, Weinans H, Carr AJ. Osteoarthritis. Lancet. 2015;386(9991):376–387. doi: 10.1016/S0140-6736(14)60802-3. [DOI] [PubMed] [Google Scholar]
- 14.Tao SC, Yuan T, Zhang YL, Yin WJ, Guo SC, Zhang CQ. Exosomes derived from miR-140-5p-overexpressing human synovial mesenchymal stem cells enhance cartilage tissue regeneration and prevent osteoarthritis of the knee in a rat model. Theranostics. 2017;7(1):180–195. doi: 10.7150/thno.17133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matas J, Orrego M, Amenabar D, Infante C, Tapia-Limonchi R, Cadiz MI, Alcayaga-Miranda F, González PL, Muse E, Khoury M, et al. Umbilical cord-derived mesenchymal stromal cells (MSCs) for knee osteoarthritis: repeated MSC dosing is superior to a single MSC dose and to hyaluronic acid in a controlled randomized phase I/II trial. Stem Cells Transl Med. 2019;8(3):215–224. doi: 10.1002/sctm.18-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Viswanathan S, Shi Y, Galipeau J, Krampera M, Leblanc K, Martin I, Nolta J, Phinney DG, Sensebe L. Mesenchymal stem versus stromal cells: international society for cell & gene therapy (ISCT®) mesenchymal stromal cell committee position statement on nomenclature. Cytotherapy. 2019;21(10):1019–1024. doi: 10.1016/j.jcyt.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Yu D, Liu Z, Zhou F, Dai J, Wu B, Zhou J, Heng BC, Zou XH, Ouyang H, et al. Exosomes from embryonic mesenchymal stem cells alleviate osteoarthritis through balancing synthesis and degradation of cartilage extracellular matrix. Stem Cell Res Ther. 2017;8(1):189. doi: 10.1186/s13287-017-0632-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freitag J, Bates D, Wickham J, Shah K, Huguenin L, Tenen A, Paterson K, Boyd R. Adipose-derived mesenchymal stem cell therapy in the treatment of knee osteoarthritis: a randomized controlled trial. Regen Med. 2019;14(3):213–230. doi: 10.2217/rme-2018-0161. [DOI] [PubMed] [Google Scholar]
- 19.Lee WS, Kim HJ, Kim KI, Kim GB, Jin W. Intra-articular injection of autologous adipose tissue-derived mesenchymal stem cells for the treatment of knee osteoarthritis: a phase IIb, randomized, placebo-controlled clinical trial. Stem Cells Transl Med. 2019;8(6):504–511. doi: 10.1002/sctm.18-0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carstairs A, Genever P. Stem cell treatment for musculoskeletal disease. Curr Opin Pharmacol. 2014;16:1–6. doi: 10.1016/j.coph.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 21.Ilas DC, Churchman SM, Baboolal T, Giannoudis PV, Aderinto J, McGonagle D, Jones E. The simultaneous analysis of mesenchymal stem cells and early osteocytes accumulation in osteoarthritic femoral head sclerotic bone. Rheumatology (Oxford) 2019;58(10):1777–1783. doi: 10.1093/rheumatology/kez130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson K, Zhu S, Tremblay MS, Payette JN, Wang J, Bouchez LC, Meeusen S, Althage A, Cho CY, Wu X, et al. A stem cell-based approach to cartilage repair. Science. 2012;336(6082):717–721. doi: 10.1126/science.1215157. [DOI] [PubMed] [Google Scholar]
- 23.Wu X, Wang W, Meng C, Yang S, Duan D, Xu W, Liu X, Tang M, Wang H. Regulation of differentiation in trabecular bone-derived mesenchymal stem cells by T cell activation and inflammation. Oncol Rep. 2013;30(5):2211–2219. doi: 10.3892/or.2013.2687. [DOI] [PubMed] [Google Scholar]
- 24.Neybecker P, Henrionnet C, Pape E, Mainard D, Galois L, Loeuille D, Gillet P, Pinzano A. In vitro and in vivo potentialities for cartilage repair from human advanced knee osteoarthritis synovial fluid-derived mesenchymal stem cells. Stem Cell Res Ther. 2018;9(1):329. doi: 10.1186/s13287-018-1071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greif DN, Kouroupis D, Murdock CJ, Griswold AJ, Kaplan LD, Best TM, Correa D. Infrapatellar fat pad/synovium complex in early-stage knee osteoarthritis: potential new target and source of therapeutic mesenchymal stem/stromal cells. Front Bioeng Biotechnol. 2020;8:860. doi: 10.3389/fbioe.2020.00860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Turajane T, Chaveewanakorn U, Fongsarun W, Aojanepong J, Papadopoulos KI. Avoidance of total knee arthroplasty in early osteoarthritis of the knee with intra-articular implantation of autologous activated peripheral blood stem cells versus hyaluronic acid: a randomized controlled trial with differential effects of growth factor addition. Stem Cells Int. 2017;2017:8925132. doi: 10.1155/2017/8925132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jacob G, Shimomura K, Krych AJ, Nakamura N. The meniscus tear: a review of stem cell therapies. Cells. 2019;9(1):92. doi: 10.3390/cells9010092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wortzel I, Dror S, Kenific CM, Lyden D. Exosome-mediated metastasis: communication from a distance. Dev Cell. 2019;49(3):347–360. doi: 10.1016/j.devcel.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 29.Doyle LM, Wang MZ. Overview of extracellular vesicles, their origin, composition, purpose, and methods for exosome isolation and analysis. Cells. 2019;8(7):727. doi: 10.3390/cells8070727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun Z, Yang S, Zhou Q, Wang G, Song J, Li Z, Zhang Z, Xu J, Xia K, Chang Y, et al. Emerging role of exosome-derived long non-coding RNAs in tumor microenvironment. Mol Cancer. 2018;17(1):82. doi: 10.1186/s12943-018-0831-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lobb RJ, Becker M, Wen SW, Wong CS, Wiegmans AP, Leimgruber A, Möller A. Optimized exosome isolation protocol for cell culture supernatant and human plasma. J Extracell Vesicles. 2015;4:27031. doi: 10.3402/jev.v4.27031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xu X, Liang Y, Li X, Ouyang K, Wang M, Cao T, Li W, Liu J, Xiong J, Li B, et al. Exosome-mediated delivery of kartogenin for chondrogenesis of synovial fluid-derived mesenchymal stem cells and cartilage regeneration. Biomaterials. 2021;269:120539. doi: 10.1016/j.biomaterials.2020.120539. [DOI] [PubMed] [Google Scholar]
- 33.McKiernan J, Donovan MJ, O'Neill V, Bentink S, Noerholm M, Belzer S, Skog J, Kattan MW, Partin A, Andriole G, et al. A novel urine exosome gene expression assay to predict high-grade prostate cancer at initial biopsy. JAMA Oncol. 2016;2(7):882–889. doi: 10.1001/jamaoncol.2016.0097. [DOI] [PubMed] [Google Scholar]
- 34.Dixon CL, Sheller-Miller S, Saade GR, Fortunato SJ, Lai A, Palma C, Guanzon D, Salomon C, Menon R. Amniotic fluid exosome proteomic profile exhibits unique pathways of term and preterm labor. Endocrinology. 2018;159(5):2229–2240. doi: 10.1210/en.2018-00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lässer C, Alikhani VS, Ekström K, Eldh M, Paredes PT, Bossios A, Sjöstrand M, Gabrielsson S, Lötvall J, Valadi H. Human saliva, plasma and breast milk exosomes contain RNA: uptake by macrophages. J Transl Med. 2011;9:9. doi: 10.1186/1479-5876-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jia L, Qiu Q, Zhang H, Chu L, Du Y, Zhang J, Zhou C, Liang F, Shi S, Wang S, et al. Concordance between the assessment of Aβ42, T-tau, and P-T181-tau in peripheral blood neuronal-derived exosomes and cerebrospinal fluid. Alzheimers Dement. 2019;15(8):1071–1080. doi: 10.1016/j.jalz.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 37.Nik Mohamed Kamal NNS, Awang RAR, Mohamad S, Shahidan WNS. Plasma- and saliva exosome profile reveals a distinct microrna signature in chronic periodontitis. Front Physiol. 2020;11:587381. doi: 10.3389/fphys.2020.587381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Inubushi S, Kawaguchi H, Mizumoto S, Kunihisa T, Baba M, Kitayama Y, Takeuchi T, Hoffman RM, Tanino H, Sasaki R. Oncogenic miRNAs identified in tear exosomes from metastatic breast cancer patients. Anticancer Res. 2020;40(6):3091–3096. doi: 10.21873/anticanres.14290. [DOI] [PubMed] [Google Scholar]
- 39.Cao Q, Guo Z, Yan Y, Wu J, Song C. Exosomal long noncoding RNAs in aging and age-related diseases. IUBMB Life. 2019;71(12):1846–1856. doi: 10.1002/iub.2141. [DOI] [PubMed] [Google Scholar]
- 40.Whiteside TL. Exosome and mesenchymal stem cell cross-talk in the tumor microenvironment. Semin Immunol. 2018;35:69–79. doi: 10.1016/j.smim.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu Y, Lin L, Zou R, Wen C, Wang Z, Lin F. MSC-derived exosomes promote proliferation and inhibit apoptosis of chondrocytes via lncRNA-KLF3-AS1/miR-206/GIT1 axis in osteoarthritis. Cell Cycle. 2018;17(21–22):2411–2422. doi: 10.1080/15384101.2018.1526603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ha DH, Kim HK, Lee J, Kwon HH, Park GH, Yang SH, Jung JY, Choi H, Lee JH, Sung S, et al. Mesenchymal stem/stromal cell-derived exosomes for immunomodulatory therapeutics and skin regeneration. Cells. 2020;9(5):1157. doi: 10.3390/cells9051157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang S, Chuah SJ, Lai RC, Hui JHP, Lim SK, Toh WS. MSC exosomes mediate cartilage repair by enhancing proliferation, attenuating apoptosis and modulating immune reactivity. Biomaterials. 2018;156:16–27. doi: 10.1016/j.biomaterials.2017.11.028. [DOI] [PubMed] [Google Scholar]
- 44.Jeppesen DK, Fenix AM, Franklin JL, Higginbotham JN, Zhang Q, Zimmerman LJ, Liebler DC, Ping J, Liu Q, Evans R, et al. Reassessment of exosome composition. Cell. 2019;177(2):428–445.e418. doi: 10.1016/j.cell.2019.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee Y-C, Chan Y-H, Hsieh S-C, Lew W-Z, Feng S-W. Comparing the osteogenic potentials and bone regeneration capacities of bone marrow and dental pulp mesenchymal stem cells in a rabbit calvarial bone defect model. Int J Mol Sci. 2019;20(20):5015. doi: 10.3390/ijms20205015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lv FJ, Tuan RS, Cheung KM, Leung VY. Concise review: the surface markers and identity of human mesenchymal stem cells. Stem Cells. 2014;32(6):1408–1419. doi: 10.1002/stem.1681. [DOI] [PubMed] [Google Scholar]
- 47.Han S-M, Han S-H, Coh Y-R, Jang G, Chan Ra J, Kang S-K, Lee H-W, Youn H-Y. Enhanced proliferation and differentiation of Oct4- and Sox2-overexpressing human adipose tissue mesenchymal stem cells. Exp Mol Med. 2014;46:e101. doi: 10.1038/emm.2014.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akhondzadeh F, Kadkhodaee M, Seifi B, Ashabi G, Kianian F, Abdolmohammadi K, Izad M, Adelipour M, Ranjbaran M. Adipose-derived mesenchymal stem cells and conditioned medium attenuate the memory retrieval impairment during sepsis in rats. Mol Neurobiol. 2020;57(9):3633–3645. doi: 10.1007/s12035-020-01991-6. [DOI] [PubMed] [Google Scholar]
- 49.Chen S, Cui G, Peng C, Lavin MF, Sun X, Zhang E, Yang Y, Guan Y, Du Z, Shao H. Transplantation of adipose-derived mesenchymal stem cells attenuates pulmonary fibrosis of silicosis via anti-inflammatory and anti-apoptosis effects in rats. Stem Cell Res Ther. 2018;9(1):110. doi: 10.1186/s13287-018-0846-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bagher Z, Kamrava SK, Alizadeh R, Farhadi M, Absalan M, Falah M, Faghihi F, Zare-Sadeghi A, Komeili A. Differentiation of neural crest stem cells from nasal mucosa into motor neuron-like cells. J Chem Neuroanat. 2018;92:35–40. doi: 10.1016/j.jchemneu.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 51.Wagenbrenner M, Heinz T, Horas K, Jakuscheit A, Arnholdt J, Herrmann M, Rudert M, Holzapfel BM, Steinert AF, Weißenberger M. The human arthritic hip joint is a source of mesenchymal stromal cells (MSCs) with extensive multipotent differentiation potential. BMC Musculoskelet Disord. 2020;21(1):297. doi: 10.1186/s12891-020-03340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.He L, He T, Xing J, Zhou Q, Fan L, Liu C, Chen Y, Wu D, Tian Z, Liu B, et al. Bone marrow mesenchymal stem cell-derived exosomes protect cartilage damage and relieve knee osteoarthritis pain in a rat model of osteoarthritis. Stem Cell Res Ther. 2020;11(1):276. doi: 10.1186/s13287-020-01781-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ramezani M, Komaki A, Hashemi-Firouzi N, Mortezaee K, Faraji N, Golipoor Z. Therapeutic effects of melatonin-treated bone marrow mesenchymal stem cells (BMSC) in a rat model of Alzheimer's disease. J Chem Neuroanat. 2020;108:101804. doi: 10.1016/j.jchemneu.2020.101804. [DOI] [PubMed] [Google Scholar]
- 54.Moraghebi R, Kirkeby A, Chaves P, Rönn RE, Sitnicka E, Parmar M, Larsson M, Herbst A, Woods N-B. Term amniotic fluid: an unexploited reserve of mesenchymal stromal cells for reprogramming and potential cell therapy applications. Stem Cell Res Ther. 2017;8(1):190. doi: 10.1186/s13287-017-0582-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dickhut A, Pelttari K, Janicki P, Wagner W, Eckstein V, Egermann M, Richter W. Calcification or dedifferentiation: requirement to lock mesenchymal stem cells in a desired differentiation stage. J Cell Physiol. 2009;219(1):219–226. doi: 10.1002/jcp.21673. [DOI] [PubMed] [Google Scholar]
- 56.Amemiya M, Tsuji K, Katagiri H, Miyatake K, Nakagawa Y, Sekiya I, Muneta T, Koga H. Synovial fluid-derived mesenchymal cells have non-inferior chondrogenic potential and can be utilized for regenerative therapy as substitute for synovium-derived cells. Biochem Biophys Res Commun. 2020;523(2):465–472. doi: 10.1016/j.bbrc.2019.12.068. [DOI] [PubMed] [Google Scholar]
- 57.Wang M, Song L, Strange C, Dong X, Wang H. Therapeutic effects of adipose stem cells from diabetic mice for the treatment of type 2 diabetes. Mol Ther. 2018;26(8):1921–1930. doi: 10.1016/j.ymthe.2018.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Erdogan Ö, Supachawaroj N, Soontornvipart K, Kheolamai P. Treatment of peri-implant defects in the rabbit's tibia with adipose or bone marrow-derived mesenchymal stems cells. Clin Implant Dent Relat Res. 2016;18(5):1003–1014. doi: 10.1111/cid.12378. [DOI] [PubMed] [Google Scholar]
- 59.Chen G, Zhang W, Zhang K, Wang S, Gao Y, Gu J, He L, Li W, Zhang C, Zhang W, et al. Hypoxia-induced mesenchymal stem cells exhibit stronger tenogenic differentiation capacities and promote patellar tendon repair in rabbits. Stem Cells Int. 2020;2020:8822609. doi: 10.1155/2020/8822609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Patel J, Shafiee A, Wang W, Fisk NM, Khosrotehrani K. Novel isolation strategy to deliver pure fetal-origin and maternal-origin mesenchymal stem cell (MSC) populations from human term placenta. Placenta. 2014;35(11):969–971. doi: 10.1016/j.placenta.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 61.Sardesai VS, Shafiee A, Fisk NM, Pelekanos RA. Avoidance of maternal cell contamination and overgrowth in isolating fetal chorionic villi mesenchymal stem cells from human term placenta. Stem Cells Transl Med. 2017;6(4):1070–1084. doi: 10.1002/sctm.15-0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dong L, Pu Y, Zhang L, Qi Q, Xu L, Li W, Wei C, Wang X, Zhou S, Zhu J, et al. Human umbilical cord mesenchymal stem cell-derived extracellular vesicles promote lung adenocarcinoma growth by transferring miR-410. Cell Death Dis. 2018;9(2):218. doi: 10.1038/s41419-018-0323-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sanchez-Guijo FM, Blanco JF, Cruz G, Muntion S, Gomez M, Carrancio S, Lopez-Villar O, Barbado M-V, Sanchez-Abarca L-I, Blanco B, et al. Multiparametric comparison of mesenchymal stromal cells obtained from trabecular bone by using a novel isolation method with those obtained by iliac crest aspiration from the same subjects. Cell Tissue Res. 2009;336(3):501–507. doi: 10.1007/s00441-009-0778-x. [DOI] [PubMed] [Google Scholar]
- 64.Lu G-D, Cheng P, Liu T, Wang Z. BMSC-derived exosomal miR-29a promotes angiogenesis and osteogenesis. Front Cell Dev Biol. 2020;8:608521. doi: 10.3389/fcell.2020.608521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lin Z, He H, Wang M, Liang J. MicroRNA-130a controls bone marrow mesenchymal stem cell differentiation towards the osteoblastic and adipogenic fate. Cell Prolif. 2019;52(6):e12688. doi: 10.1111/cpr.12688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284(5411):143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 67.Wiegner R, Rudhart NE, Barth E, Gebhard F, Lampl L, Huber-Lang MS, Brenner RE. Mesenchymal stem cells in peripheral blood of severely injured patients. Eur J Trauma Emerg Surg. 2018;44(4):627–636. doi: 10.1007/s00068-017-0849-8. [DOI] [PubMed] [Google Scholar]
- 68.Wang Z-G, He Z-Y, Liang S, Yang Q, Cheng P, Chen A-M. Comprehensive proteomic analysis of exosomes derived from human bone marrow, adipose tissue, and umbilical cord mesenchymal stem cells. Stem Cell Res Ther. 2020;11(1):511. doi: 10.1186/s13287-020-02032-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Samsonraj RM, Raghunath M, Nurcombe V, Hui JH, van Wijnen AJ, Cool SM. Concise review: multifaceted characterization of human mesenchymal stem cells for use in regenerative medicine. Stem Cells Transl Med. 2017;6(12):2173–2185. doi: 10.1002/sctm.17-0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Longhini ALF, Salazar TE, Vieira C, Trinh T, Duan Y, Pay LM, Li Calzi S, Losh M, Johnston NA, Xie H, et al. Peripheral blood-derived mesenchymal stem cells demonstrate immunomodulatory potential for therapeutic use in horses. PLoS ONE. 2019;14(3):e0212642. doi: 10.1371/journal.pone.0212642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jiang Y, Tuan RS. Origin and function of cartilage stem/progenitor cells in osteoarthritis. Nat Rev Rheumatol. 2015;11(4):206–212. doi: 10.1038/nrrheum.2014.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chaganty BK, Lu Y, Qiu S, Somanchi SS, Lee DA, Fan Z. Trastuzumab upregulates expression of HLA-ABC and T cell costimulatory molecules through engagement of natural killer cells and stimulation of IFNγ secretion. Oncoimmunology. 2016;5(4):e1100790. doi: 10.1080/2162402X.2015.1100790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Soundararajan M, Kannan S. Fibroblasts and mesenchymal stem cells: two sides of the same coin? J Cell Physiol. 2018;233(12):9099–9109. doi: 10.1002/jcp.26860. [DOI] [PubMed] [Google Scholar]
- 74.Plaza Reyes A, Petrus-Reurer S, Padrell Sánchez S, Kumar P, Douagi I, Bartuma H, Aronsson M, Westman S, Lardner E, André H, et al. Identification of cell surface markers and establishment of monolayer differentiation to retinal pigment epithelial cells. Nat Commun. 2020;11(1):1609. doi: 10.1038/s41467-020-15326-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yao Y, Chen R, Wang G, Zhang Y, Liu F. Exosomes derived from mesenchymal stem cells reverse EMT via TGF-β1/Smad pathway and promote repair of damaged endometrium. Stem Cell Res Ther. 2019;10(1):225. doi: 10.1186/s13287-019-1332-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zuo R, Liu M, Wang Y, Li J, Wang W, Wu J, Sun C, Li B, Wang Z, Lan W, et al. BM-MSC-derived exosomes alleviate radiation-induced bone loss by restoring the function of recipient BM-MSCs and activating Wnt/β-catenin signaling. Stem Cell Res Ther. 2019;10(1):30. doi: 10.1186/s13287-018-1121-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Roccaro AM, Sacco A, Maiso P, Azab AK, Tai Y-T, Reagan M, Azab F, Flores LM, Campigotto F, Weller E, et al. BM mesenchymal stromal cell-derived exosomes facilitate multiple myeloma progression. J Clin Investig. 2013;123(4):1542–1555. doi: 10.1172/JCI66517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Berger DR, Aune ET, Centeno CJ, Steinmetz NJ. Cryopreserved bone marrow aspirate concentrate as a cell source for the colony-forming unit fibroblast assay. Cytotherapy. 2020;22(9):486–493. doi: 10.1016/j.jcyt.2020.04.091. [DOI] [PubMed] [Google Scholar]
- 79.Baustian C, Hanley S, Ceredig R. Isolation, selection and culture methods to enhance clonogenicity of mouse bone marrow derived mesenchymal stromal cell precursors. Stem Cell Res Ther. 2015;6(1):151. doi: 10.1186/s13287-015-0139-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bornes TD, Adesida AB, Jomha NM. Mesenchymal stem cells in the treatment of traumatic articular cartilage defects: a comprehensive review. Arthritis Res Ther. 2014;16(5):432. doi: 10.1186/s13075-014-0432-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yin H, Wang Y, Sun Z, Sun X, Xu Y, Li P, Meng H, Yu X, Xiao B, Fan T, et al. Induction of mesenchymal stem cell chondrogenic differentiation and functional cartilage microtissue formation for in vivo cartilage regeneration by cartilage extracellular matrix-derived particles. Acta Biomater. 2016;33:96–109. doi: 10.1016/j.actbio.2016.01.024. [DOI] [PubMed] [Google Scholar]
- 82.Frith JE, Thomson B, Genever PG. Dynamic three-dimensional culture methods enhance mesenchymal stem cell properties and increase therapeutic potential. Tissue Eng Part C Methods. 2010;16(4):735–749. doi: 10.1089/ten.TEC.2009.0432. [DOI] [PubMed] [Google Scholar]
- 83.Gegg C, Yang F. The effects of ROCK inhibition on mesenchymal stem cell chondrogenesis are culture model dependent. Tissue Eng Part A. 2020;26(3–4):130–139. doi: 10.1089/ten.tea.2019.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang L, Su P, Xu C, Yang J, Yu W, Huang D. Chondrogenic differentiation of human mesenchymal stem cells: a comparison between micromass and pellet culture systems. Biotech Lett. 2010;32(9):1339–1346. doi: 10.1007/s10529-010-0293-x. [DOI] [PubMed] [Google Scholar]
- 85.Ramezanifard R, Kabiri M, Hanaee Ahvaz H. Effects of platelet rich plasma and chondrocyte co-culture on MSC chondrogenesis, hypertrophy and pathological responses. Excli J. 2017;16:1031–1045. doi: 10.17179/excli2017-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mao G, Zhang Z, Hu S, Zhang Z, Chang Z, Huang Z, Liao W, Kang Y. Exosomes derived from miR-92a-3p-overexpressing human mesenchymal stem cells enhance chondrogenesis and suppress cartilage degradation via targeting WNT5A. Stem Cell Res Ther. 2018;9(1):247. doi: 10.1186/s13287-018-1004-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Dickinson SC, Sutton CA, Brady K, Salerno A, Katopodi T, Williams RL, West CC, Evseenko D, Wu L, Pang S, et al. The Wnt5a receptor, receptor tyrosine kinase-like orphan receptor 2, is a predictive cell surface marker of human mesenchymal stem cells with an enhanced capacity for chondrogenic differentiation. Stem Cells. 2017;35(11):2280–2291. doi: 10.1002/stem.2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Muñoz-Criado I, Meseguer-Ripolles J, Mellado-López M, Alastrue-Agudo A, Griffeth RJ, Forteza-Vila J, Cugat R, García M, Moreno-Manzano V. Human suprapatellar fat pad-derived mesenchymal stem cells induce chondrogenesis and cartilage repair in a model of severe osteoarthritis. Stem Cells Int. 2017;2017:4758930. doi: 10.1155/2017/4758930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhang Q, Xiang E, Rao W, Zhang YQ, Xiao CH, Li CY, Han B, Wu D. Intra-articular injection of human umbilical cord mesenchymal stem cells ameliorates monosodium iodoacetate-induced osteoarthritis in rats by inhibiting cartilage degradation and inflammation. Bone Joint Res. 2021;10(3):226–236. doi: 10.1302/2046-3758.103.BJR-2020-0206.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhi Z, Zhang C, Kang J, Wang Y, Liu J, Wu F, Xu G. The therapeutic effect of bone marrow-derived mesenchymal stem cells on osteoarthritis is improved by the activation of the KDM6A/SOX9 signaling pathway caused by exposure to hypoxia. J Cell Physiol. 2020;235(10):7173–7182. doi: 10.1002/jcp.29615. [DOI] [PubMed] [Google Scholar]
- 91.Wang K, Li F, Yuan Y, Shan L, Cui Y, Qu J, Lian F. Synovial mesenchymal stem cell-derived EV-Packaged miR-31 downregulates histone demethylase KDM2A to prevent knee osteoarthritis. Mol Ther Nucleic Acids. 2020;22:1078–1091. doi: 10.1016/j.omtn.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang R, Xu B, Xu H. TGF-β1 promoted chondrocyte proliferation by regulating Sp1 through MSC-exosomes derived miR-135b. Cell Cycle. 2018;17(24):2756–2765. doi: 10.1080/15384101.2018.1556063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rong Y, Zhang J, Jiang D, Ji C, Liu W, Wang J, Ge X, Tang P, Yu S, Cui W, et al. Hypoxic pretreatment of small extracellular vesicles mediates cartilage repair in osteoarthritis by delivering miR-216a-5p. Acta Biomater. 2021;122:325–342. doi: 10.1016/j.actbio.2020.12.034. [DOI] [PubMed] [Google Scholar]
- 94.Chen W, Sun Y, Gu X, Hao Y, Liu X, Lin J, Chen J, Chen S. Conditioned medium of mesenchymal stem cells delays osteoarthritis progression in a rat model by protecting subchondral bone, maintaining matrix homeostasis, and enhancing autophagy. J Tissue Eng Regen Med. 2019;13(9):1618–1628. doi: 10.1002/term.2916. [DOI] [PubMed] [Google Scholar]
- 95.Zhou J, Wang Y, Liu Y, Zeng H, Xu H, Lian F. Adipose derived mesenchymal stem cells alleviated osteoarthritis and chondrocyte apoptosis through autophagy inducing. J Cell Biochem. 2018;120:2198–2212. doi: 10.1002/jcb.27530. [DOI] [PubMed] [Google Scholar]
- 96.Dong J, Li L, Fang X, Zang M. Exosome-encapsulated microRNA-127-3p released from bone marrow-derived mesenchymal stem cells alleviates osteoarthritis through regulating CDH11-mediated Wnt/β-catenin pathway. J Pain Res. 2021;14:297–310. doi: 10.2147/JPR.S291472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wu J, Kuang L, Chen C, Yang J, Zeng WN, Li T, Chen H, Huang S, Fu Z, Li J, et al. miR-100-5p-abundant exosomes derived from infrapatellar fat pad MSCs protect articular cartilage and ameliorate gait abnormalities via inhibition of mTOR in osteoarthritis. Biomaterials. 2019;206:87–100. doi: 10.1016/j.biomaterials.2019.03.022. [DOI] [PubMed] [Google Scholar]
- 98.Prasadam I, Akuien A, Friis TE, Fang W, Mao X, Crawford RW, Xiao Y. Mixed cell therapy of bone marrow-derived mesenchymal stem cells and articular cartilage chondrocytes ameliorates osteoarthritis development. Lab Invest. 2018;98(1):106–116. doi: 10.1038/labinvest.2017.117. [DOI] [PubMed] [Google Scholar]
- 99.Wang AT, Zhang QF, Wang NX, Yu CY, Liu RM, Luo Y, Zhao YJ, Xiao JH. Cocktail of hyaluronic acid and human amniotic mesenchymal cells effectively repairs cartilage injuries in sodium iodoacetate-induced osteoarthritis rats. Front Bioeng Biotechnol. 2020;8:87. doi: 10.3389/fbioe.2020.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Antonioli E, Piccinato CA, Nader HB, Cohen M, Goldberg AC, Ferretti M. Modulation of Hyaluronan Synthesis by the Interaction between Mesenchymal Stem Cells and Osteoarthritic Chondrocytes. Stem Cells Int. 2015;2015:640218. doi: 10.1155/2015/640218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chen X, Shi Y, Xue P, Ma X, Li J, Zhang J. Mesenchymal stem cell-derived exosomal microRNA-136-5p inhibits chondrocyte degeneration in traumatic osteoarthritis by targeting ELF3. Arthritis Res Ther. 2020;22(1):256. doi: 10.1186/s13075-020-02325-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.van Geffen EW, van Caam APM, Vitters EL, van Beuningen HM, van de Loo FA, van Lent P, Koenders MI, van der Kraan PM. Interleukin-37 protects stem cell-based cartilage formation in an inflammatory osteoarthritis-like microenvironment. Tissue Eng Part A. 2019;25(15–16):1155–1166. doi: 10.1089/ten.TEA.2018.0267. [DOI] [PubMed] [Google Scholar]
- 103.Fahy N, de Vries-van Melle ML, Lehmann J, Wei W, Grotenhuis N, Farrell E, van der Kraan PM, Murphy JM, Bastiaansen-Jenniskens YM, van Osch GJ. Human osteoarthritic synovium impacts chondrogenic differentiation of mesenchymal stem cells via macrophage polarisation state. Osteoarthritis Cartilage. 2014;22(8):1167–1175. doi: 10.1016/j.joca.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 104.Huang S, Song X, Li T, Xiao J, Chen Y, Gong X, Zeng W, Yang L, Chen C. Pellet coculture of osteoarthritic chondrocytes and infrapatellar fat pad-derived mesenchymal stem cells with chitosan/hyaluronic acid nanoparticles promotes chondrogenic differentiation. Stem Cell Res Ther. 2017;8(1):264. doi: 10.1186/s13287-017-0719-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.van Buul GM, Villafuertes E, Bos PK, Waarsing JH, Kops N, Narcisi R, Weinans H, Verhaar JA, Bernsen MR, van Osch GJ. Mesenchymal stem cells secrete factors that inhibit inflammatory processes in short-term osteoarthritic synovium and cartilage explant culture. Osteoarthr Cartil. 2012;20(10):1186–1196. doi: 10.1016/j.joca.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 106.Chang YH, Wu KC, Ding DC. Induced pluripotent stem cell-differentiated chondrocytes repair cartilage defect in a rabbit osteoarthritis model. Stem Cells Int. 2020;2020:8867349. doi: 10.1155/2020/8867349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Pagani S, Veronesi F, Giavaresi G, Filardo G, Papio T, Romandini I, Fini M: Autologous protein solution effect on chondrogenic differentiation of mesenchymal stem cells from adipose tissue and bone marrow in an osteoarthritic environment. Cartilage. 2021; 1947603521993217. [DOI] [PMC free article] [PubMed]
- 108.Mei L, Shen B, Ling P, Liu S, Xue J, Liu F, Shao H, Chen J, Ma A, Liu X. Culture-expanded allogenic adipose tissue-derived stem cells attenuate cartilage degeneration in an experimental rat osteoarthritis model. PLoS ONE. 2017;12(4):e0176107. doi: 10.1371/journal.pone.0176107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhao C, Chen JY, Peng WM, Yuan B, Bi Q, Xu YJ. Exosomes from adipose-derived stem cells promote chondrogenesis and suppress inflammation by upregulating miR-145 and miR-221. Mol Med Rep. 2020;21(4):1881–1889. doi: 10.3892/mmr.2020.10982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jin Z, Ren J, Qi S. Exosomal miR-9-5p secreted by bone marrow-derived mesenchymal stem cells alleviates osteoarthritis by inhibiting syndecan-1. Cell Tissue Res. 2020;381(1):99–114. doi: 10.1007/s00441-020-03193-x. [DOI] [PubMed] [Google Scholar]
- 111.Lu L, Wang J, Fan A, Wang P, Chen R, Lu L, Yin F. Synovial mesenchymal stem cell-derived extracellular vesicles containing microRN555A-26a-5p ameliorate cartilage damage of osteoarthritis. J Gene Med. 2021;23:e3379. doi: 10.1002/jgm.3379. [DOI] [PubMed] [Google Scholar]
- 112.Jin Z, Ren J, Qi S. Human bone mesenchymal stem cells-derived exosomes overexpressing microRNA-26a-5p alleviate osteoarthritis via down-regulation of PTGS2. Int Immunopharmacol. 2020;78:105946. doi: 10.1016/j.intimp.2019.105946. [DOI] [PubMed] [Google Scholar]
- 113.Cifù A, Domenis R, Pozzi-Mucelli M, Di Benedetto P, Causero A, Moretti M, Stevanato M, Pistis C, Parodi PC, Fabris M, et al. The Exposure to osteoarthritic synovial fluid enhances the immunomodulatory profile of adipose mesenchymal stem cell secretome. Stem Cells Int. 2020;2020:4058760. doi: 10.1155/2020/4058760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ragni E, Perucca Orfei C, De Luca P, Mondadori C, Viganò M, Colombini A, de Girolamo L. Inflammatory priming enhances mesenchymal stromal cell secretome potential as a clinical product for regenerative medicine approaches through secreted factors and EV-miRNAs: the example of joint disease. Stem Cell Res Ther. 2020;11(1):165. doi: 10.1186/s13287-020-01677-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhang J, Rong Y, Luo C, Cui W. Bone marrow mesenchymal stem cell-derived exosomes prevent osteoarthritis by regulating synovial macrophage polarization. Aging. 2020;12(24):25138–25152. doi: 10.18632/aging.104110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Woo CH, Kim HK, Jung GY, Jung YJ, Lee KS, Yun YE, Han J, Lee J, Kim WS, Choi JS, et al. Small extracellular vesicles from human adipose-derived stem cells attenuate cartilage degeneration. J Extracell Vesicles. 2020;9(1):1735249. doi: 10.1080/20013078.2020.1735249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wang R, Xu B. TGF-β1-modified MSC-derived exosomal miR-135b attenuates cartilage injury via promoting M2 synovial macrophage polarization by targeting MAPK6. Cell Tissue Res. 2021;384(1):113–127. doi: 10.1007/s00441-020-03319-1. [DOI] [PubMed] [Google Scholar]
- 118.Coryell PR, Diekman BO, Loeser RF. Mechanisms and therapeutic implications of cellular senescence in osteoarthritis. Nat Rev Rheumatol. 2021;17(1):47–57. doi: 10.1038/s41584-020-00533-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wang R, Maimaitijuma T, Ma YY, Jiao Y, Cao YP. Mitochondrial transfer from bone-marrow-derived mesenchymal stromal cells to chondrocytes protects against cartilage degenerative mitochondrial dysfunction in rats chondrocytes. Chin Med J (Engl) 2020;134(2):212–218. doi: 10.1097/CM9.0000000000001057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hassanzadeh A, Rahman HS, Markov A, Endjun JJ, Zekiy AO, Chartrand MS, Beheshtkhoo N, Kouhbanani MAJ, Marofi F, Nikoo M, et al. Mesenchymal stem/stromal cell-derived exosomes in regenerative medicine and cancer; overview of development, challenges, and opportunities. Stem Cell Res Ther. 2021;12(1):297. doi: 10.1186/s13287-021-02378-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Vonk LA, van Dooremalen SFJ, Liv N, Klumperman J, Coffer PJ, Saris DBF, Lorenowicz MJ. Mesenchymal stromal/stem cell-derived extracellular vesicles promote human cartilage regeneration in vitro. Theranostics. 2018;8(4):906–920. doi: 10.7150/thno.20746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang Q, Lenardo MJ, Baltimore D. 30 Years of NF-kappaB: a blossoming of relevance to human pathobiology. Cell. 2017;168(1–2):37–57. doi: 10.1016/j.cell.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yu S, Li P, Li B, Miao D, Deng Q. RelA promotes proliferation but inhibits osteogenic and chondrogenic differentiation of mesenchymal stem cells. FEBS Lett. 2020;594(9):1368–1378. doi: 10.1002/1873-3468.13739. [DOI] [PubMed] [Google Scholar]
- 124.Lee SY, Lee SH, Na HS, Kwon JY, Kim GY, Jung K, Cho KH, Kim SA, Go EJ, Park MJ, et al. The therapeutic effect of STAT3 signaling-suppressed MSC on pain and articular cartilage damage in a rat model of monosodium iodoacetate-induced osteoarthritis. Front Immunol. 2018;9:2881. doi: 10.3389/fimmu.2018.02881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Qi H, Liu DP, Xiao DW, Tian DC, Su YW, Jin SF. Exosomes derived from mesenchymal stem cells inhibit mitochondrial dysfunction-induced apoptosis of chondrocytes via p38, ERK, and Akt pathways. In Vitro Cell Dev Biol Anim. 2019;55(3):203–210. doi: 10.1007/s11626-019-00330-x. [DOI] [PubMed] [Google Scholar]
- 126.Platas J, Guillén MI, Pérez Del Caz MD, Gomar F, Castejón MA, Mirabet V, Alcaraz MJ. Paracrine effects of human adipose-derived mesenchymal stem cells in inflammatory stress-induced senescence features of osteoarthritic chondrocytes. Aging. 2016;8(8):1703–1717. doi: 10.18632/aging.101007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.van Dalen SCM, Blom AB, Walgreen B, Slöetjes AW, Helsen MMA, Geven EJW, Ter Huurne M, Vogl T, Roth J, van de Loo FAJ, et al. IL-1β-mediated activation of adipose-derived mesenchymal stromal cells results in PMN reallocation and enhanced phagocytosis: a possible mechanism for the reduction of osteoarthritis pathology. Front Immunol. 2019;10:1075. doi: 10.3389/fimmu.2019.01075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Guillen MI, Tofino-Vian M, Silvestre A, Castejon MA, Alcaraz MJ. Role of peroxiredoxin 6 in the chondroprotective effects of microvesicles from human adipose tissue-derived mesenchymal stem cells. J Orthop Translat. 2021;30:61–69. doi: 10.1016/j.jot.2021.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.An X, Wang T, Zhang W, Yu H, Chunhua Zhao R, Guo Y, Wang C, Qin L, Guo C. Chondroprotective effects of combination therapy of acupotomy and human adipose mesenchymal stem cells in knee osteoarthritis rabbits via the GSK3β-cyclin D1-CDK4/CDK6 signaling pathway. Aging Dis. 2020;11(5):1116–1132. doi: 10.14336/AD.2019.1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wu Z, Lu H, Yao J, Zhang X, Huang Y, Ma S, Zou K, Wei Y, Yang Z, Li J, et al. GABARAP promotes bone marrow mesenchymal stem cells-based the osteoarthritis cartilage regeneration through the inhibition of PI3K/AKT/mTOR signaling pathway. J Cell Physiol. 2019;234(11):21014–21026. doi: 10.1002/jcp.28705. [DOI] [PubMed] [Google Scholar]
- 131.Ruiz M, Toupet K, Maumus M, Rozier P, Jorgensen C, Noël D. TGFBI secreted by mesenchymal stromal cells ameliorates osteoarthritis and is detected in extracellular vesicles. Biomaterials. 2020;226:119544. doi: 10.1016/j.biomaterials.2019.119544. [DOI] [PubMed] [Google Scholar]
- 132.Jeon HJ, Yoon KA, An ES, Kang TW, Sim YB, Ahn J, Choi EK, Lee S, Seo KW, Kim YB, et al. Therapeutic effects of human umbilical cord blood-derived mesenchymal stem cells combined with cartilage acellular matrix mediated via bone morphogenic protein 6 in a rabbit model of articular cruciate ligament transection. Stem Cell Rev Rep. 2020;16(3):596–611. doi: 10.1007/s12015-020-09958-9. [DOI] [PubMed] [Google Scholar]
- 133.Lin S, Lee WYW, Xu L, Wang Y, Chen Y, Ho KKW, Qin L, Jiang X, Cui L, Li G. Stepwise preconditioning enhances mesenchymal stem cell-based cartilage regeneration through epigenetic modification. Osteoarthritis Cartilage. 2017;25(9):1541–1550. doi: 10.1016/j.joca.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 134.Xiang X, Liu H, Wang L, Zhu B, Ma L, Du F, Li L, Qiu L. Ultrasound combined with SDF-1α chemotactic microbubbles promotes stem cell homing in an osteoarthritis model. J Cell Mol Med. 2020;24(18):10816–10829. doi: 10.1111/jcmm.15706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zhang Y, Huang X, Yuan Y. MicroRNA-410 promotes chondrogenic differentiation of human bone marrow mesenchymal stem cells through down-regulating Wnt3a. Am J Transl Res. 2017;9(1):136–145. [PMC free article] [PubMed] [Google Scholar]
- 136.Wang Z, Yan K, Ge G, Zhang D, Bai J, Guo X, Zhou J, Xu T, Xu M, Long X, et al. Exosomes derived from miR-155-5p-overexpressing synovial mesenchymal stem cells prevent osteoarthritis via enhancing proliferation and migration, attenuating apoptosis, and modulating extracellular matrix secretion in chondrocytes. Cell Biol Toxicol. 2021;37(1):85–96. doi: 10.1007/s10565-020-09559-9. [DOI] [PubMed] [Google Scholar]
- 137.Tao Y, Zhou J, Wang Z, Tao H, Bai J, Ge G, Li W, Zhang W, Hao Y, Yang X, et al. Human bone mesenchymal stem cells-derived exosomal miRNA-361-5p alleviates osteoarthritis by downregulating DDX20 and inactivating the NF-κB signaling pathway. Bioorg Chem. 2021;113:104978. doi: 10.1016/j.bioorg.2021.104978. [DOI] [PubMed] [Google Scholar]
- 138.Qiu B, Xu X, Yi P, Hao Y. Curcumin reinforces MSC-derived exosomes in attenuating osteoarthritis via modulating the miR-124/NF-kB and miR-143/ROCK1/TLR9 signalling pathways. J Cell Mol Med. 2020;24(18):10855–10865. doi: 10.1111/jcmm.15714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hu N, Gao Y, Jayasuriya CT, Liu W, Du H, Ding J, Feng M, Chen Q. Chondrogenic induction of human osteoarthritic cartilage-derived mesenchymal stem cells activates mineralization and hypertrophic and osteogenic gene expression through a mechanomiR. Arthritis Res Ther. 2019;21(1):167. doi: 10.1186/s13075-019-1949-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lu J, Zhou Z, Sun B, Han B, Fu Q, Han Y, Yuan W, Xu Z, Chen A. MiR-520d-5p modulates chondrogenesis and chondrocyte metabolism through targeting HDAC1. Aging. 2020;12(18):18545–18560. doi: 10.18632/aging.103831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zhu J, Fu Q, Shao J, Jinhui P, Qian Q, Zhou Y, Yi C. Regulating effect of Circ_ATRNL1 on the promotion of SOX9 expression to promote chondrogenic differentiation of hAMSCs mediated by MiR-145-5p. J Tissue Eng Regen Med. 2021;15(5):487–502. doi: 10.1002/term.3189. [DOI] [PubMed] [Google Scholar]
- 142.Mao G, Xu Y, Long D, Sun H, Li H, Xin R, Zhang Z, Li Z, Yang Z, Kang Y. Exosome-transported circRNA_0001236 enhances chondrogenesis and suppress cartilage degradation via the miR-3677-3p/Sox9 axis. Stem Cell Res Ther. 2021;12(1):389. doi: 10.1186/s13287-021-02431-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Li S, Liu J, Liu S, Jiao W, Wang X. Mesenchymal stem cell-derived extracellular vesicles prevent the development of osteoarthritis via the circHIPK3/miR-124-3p/MYH9 axis. J Nanobiotechnology. 2021;19(1):194. doi: 10.1186/s12951-021-00940-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Huynh NP, Gloss CC, Lorentz J, Tang R, Brunger JM, McAlinden A, Zhang B, Guilak F. Long non-coding RNA GRASLND enhances chondrogenesis via suppression of the interferon type II signaling pathway. Elife. 2020;9:e49558. doi: 10.7554/eLife.49558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.You D, Yang C, Huang J, Gong H, Yan M, Ni J. Long non-coding RNA MEG3 inhibits chondrogenic differentiation of synovium-derived mesenchymal stem cells by epigenetically inhibiting TRIB2 via methyltransferase EZH2. Cell Signal. 2019;63:109379. doi: 10.1016/j.cellsig.2019.109379. [DOI] [PubMed] [Google Scholar]
- 146.Xiao Y, Yan X, Yang Y, Ma X. Downregulation of long noncoding RNA HOTAIRM1 variant 1 contributes to osteoarthritis via regulating miR-125b/BMPR2 axis and activating JNK/MAPK/ERK pathway. Biomed Pharmacother. 2019;109:1569–1577. doi: 10.1016/j.biopha.2018.10.181. [DOI] [PubMed] [Google Scholar]
- 147.Mao G, Kang Y, Lin R, Hu S, Zhang Z, Li H, Liao W, Zhang Z. Long non-coding RNA HOTTIP promotes CCL3 expression and induces cartilage degradation by sponging miR-455-3p. Front Cell Dev Biol. 2019;7:161. doi: 10.3389/fcell.2019.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Cui P, Zhao X, Liu J, Chen X, Gao Y, Tao K, Wang C, Zhang X. miR-146a interacting with lncRNA EPB41L4A-AS1 and lncRNA SNHG7 inhibits proliferation of bone marrow-derived mesenchymal stem cells. J Cell Physiol. 2020;235(4):3292–3308. doi: 10.1002/jcp.29217. [DOI] [PubMed] [Google Scholar]
- 149.Wang X, Li Z, Cui Y, Cui X, Chen C, Wang Z. Exosomes isolated from bone marrow mesenchymal stem cells exert a protective effect on osteoarthritis via lncRNA LYRM4-AS1-GRPR-miR-6515-5p. Front Cell Dev Biol. 2021;9:644380. doi: 10.3389/fcell.2021.644380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Pattappa G, Krueckel J, Schewior R, Franke D, Mench A, Koch M, Weber J, Lang S, Pfeifer CG, Johnstone B, et al. Physioxia expanded bone marrow derived mesenchymal stem cells have improved cartilage repair in an early osteoarthritic focal defect model. Biology. 2020;9(8):230. doi: 10.3390/biology9080230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Buckley CT, Vinardell T, Kelly DJ. Oxygen tension differentially regulates the functional properties of cartilaginous tissues engineered from infrapatellar fat pad derived MSCs and articular chondrocytes. Osteoarthr Cartil. 2010;18(10):1345–1354. doi: 10.1016/j.joca.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 152.Dos Santos F, Andrade PZ, Boura JS, Abecasis MM, da Silva CL, Cabral JM. Ex vivo expansion of human mesenchymal stem cells: a more effective cell proliferation kinetics and metabolism under hypoxia. J Cell Physiol. 2010;223(1):27–35. doi: 10.1002/jcp.21987. [DOI] [PubMed] [Google Scholar]
- 153.Huang J, Liang Y, Huang Z, Zhao P, Liang Q, Liu Y, Duan L, Liu W, Zhu F, Bian L, et al. Magnetic enhancement of chondrogenic differentiation of mesenchymal stem cells. ACS Biomater Sci Eng. 2019;5(5):2200–2207. doi: 10.1021/acsbiomaterials.9b00025. [DOI] [PubMed] [Google Scholar]
- 154.Amin HD, Brady MA, St-Pierre JP, Stevens MM, Overby DR, Ethier CR. Stimulation of chondrogenic differentiation of adult human bone marrow-derived stromal cells by a moderate-strength static magnetic field. Tissue Eng Part A. 2014;20(11–12):1612–1620. doi: 10.1089/ten.tea.2013.0307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ongaro A, Pellati A, Setti S, Masieri FF, Aquila G, Fini M, Caruso A, De Mattei M. Electromagnetic fields counteract IL-1β activity during chondrogenesis of bovine mesenchymal stem cells. J Tissue Eng Regen Med. 2015;9(12):E229–238. doi: 10.1002/term.1671. [DOI] [PubMed] [Google Scholar]
- 156.Centeno CJ, Busse D, Kisiday J, Keohan C, Freeman M, Karli D. Increased knee cartilage volume in degenerative joint disease using percutaneously implanted, autologous mesenchymal stem cells. Pain Physician. 2008;11(3):343–353. [PubMed] [Google Scholar]
- 157.Vega A, Martín-Ferrero MA, Del Canto F, Alberca M, García V, Munar A, Orozco L, Soler R, Fuertes JJ, Huguet M, et al. Treatment of knee osteoarthritis with allogeneic bone marrow mesenchymal stem cells: a randomized controlled trial. Transplantation. 2015;99(8):1681–1690. doi: 10.1097/TP.0000000000000678. [DOI] [PubMed] [Google Scholar]
- 158.Soler R, Orozco L, Munar A, Huguet M, López R, Vives J, Coll R, Codinach M, Garcia-Lopez J. Final results of a phase I-II trial using ex vivo expanded autologous Mesenchymal Stromal Cells for the treatment of osteoarthritis of the knee confirming safety and suggesting cartilage regeneration. Knee. 2016;23(4):647–654. doi: 10.1016/j.knee.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 159.Orozco L, Munar A, Soler R, Alberca M, Soler F, Huguet M, Sentís J, Sánchez A, García-Sancho J. Treatment of knee osteoarthritis with autologous mesenchymal stem cells: a pilot study. Transplantation. 2013;95(12):1535–1541. doi: 10.1097/TP.0b013e318291a2da. [DOI] [PubMed] [Google Scholar]
- 160.Lamo-Espinosa JM, Mora G, Blanco JF, Granero-Moltó F, Nuñez-Córdoba JM, Sánchez-Echenique C, Bondía JM, Aquerreta JD, Andreu EJ, Ornilla E, et al. Intra-articular injection of two different doses of autologous bone marrow mesenchymal stem cells versus hyaluronic acid in the treatment of knee osteoarthritis: multicenter randomized controlled clinical trial (phase I/II) J Transl Med. 2016;14(1):246. doi: 10.1186/s12967-016-0998-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lamo-Espinosa JM, Blanco JF, Sánchez M, Moreno V, Granero-Moltó F, Sánchez-Guijo F, Crespo-Cullel Í, Mora G, San Vicente DD, Pompei-Fernández O, et al. Phase II multicenter randomized controlled clinical trial on the efficacy of intra-articular injection of autologous bone marrow mesenchymal stem cells with platelet rich plasma for the treatment of knee osteoarthritis. J Transl Med. 2020;18(1):356. doi: 10.1186/s12967-020-02530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hernigou P, Delambre J, Quiennec S, Poignard A. Human bone marrow mesenchymal stem cell injection in subchondral lesions of knee osteoarthritis: a prospective randomized study versus contralateral arthroplasty at a mean fifteen year follow-up. Int Orthop. 2021;45(2):365–373. doi: 10.1007/s00264-020-04571-4. [DOI] [PubMed] [Google Scholar]
- 163.Gupta PK, Chullikana A, Rengasamy M, Shetty N, Pandey V, Agarwal V, Wagh SY, Vellotare PK, Damodaran D, Viswanathan P, et al. Efficacy and safety of adult human bone marrow-derived, cultured, pooled, allogeneic mesenchymal stromal cells (Stempeucel®): preclinical and clinical trial in osteoarthritis of the knee joint. Arthritis Res Ther. 2016;18(1):301. doi: 10.1186/s13075-016-1195-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Emadedin M, Labibzadeh N, Liastani MG, Karimi A, Jaroughi N, Bolurieh T, Hosseini SE, Baharvand H, Aghdami N. Intra-articular implantation of autologous bone marrow-derived mesenchymal stromal cells to treat knee osteoarthritis: a randomized, triple-blind, placebo-controlled phase 1/2 clinical trial. Cytotherapy. 2018;20(10):1238–1246. doi: 10.1016/j.jcyt.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 165.Davatchi F, Abdollahi BS, Mohyeddin M, Shahram F, Nikbin B. Mesenchymal stem cell therapy for knee osteoarthritis. Preliminary report of four patients. Int J Rheum Dis. 2011;14(2):211–215. doi: 10.1111/j.1756-185X.2011.01599.x. [DOI] [PubMed] [Google Scholar]
- 166.Chahal J, Gómez-Aristizábal A, Shestopaloff K, Bhatt S, Chaboureau A, Fazio A, Chisholm J, Weston A, Chiovitti J, Keating A, et al. Bone marrow mesenchymal stromal cell treatment in patients with osteoarthritis results in overall improvement in pain and symptoms and reduces synovial inflammation. Stem Cells Transl Med. 2019;8(8):746–757. doi: 10.1002/sctm.18-0183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Bastos R, Mathias M, Andrade R, Bastos R, Balduino A, Schott V, Rodeo S, Espregueira-Mendes J. Intra-articular injections of expanded mesenchymal stem cells with and without addition of platelet-rich plasma are safe and effective for knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2018;26(11):3342–3350. doi: 10.1007/s00167-018-4883-9. [DOI] [PubMed] [Google Scholar]
- 168.Bastos R, Mathias M, Andrade R, Amaral R, Schott V, Balduino A, Bastos R, Miguel Oliveira J, Reis RL, Rodeo S, et al. Intra-articular injection of culture-expanded mesenchymal stem cells with or without addition of platelet-rich plasma is effective in decreasing pain and symptoms in knee osteoarthritis: a controlled, double-blind clinical trial. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1989–1999. doi: 10.1007/s00167-019-05732-8. [DOI] [PubMed] [Google Scholar]
- 169.Al-Najar M, Khalil H, Al-Ajlouni J, Al-Antary E, Hamdan M, Rahmeh R, Alhattab D, Samara O, Yasin M, Abdullah AA, et al. Intra-articular injection of expanded autologous bone marrow mesenchymal cells in moderate and severe knee osteoarthritis is safe: a phase I/II study. J Orthop Surg Res. 2017;12(1):190. doi: 10.1186/s13018-017-0689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Song Y, Du H, Dai C, Zhang L, Li S, Hunter DJ, Lu L, Bao C. Human adipose-derived mesenchymal stem cells for osteoarthritis: a pilot study with long-term follow-up and repeated injections. Regen Med. 2018;13(3):295–307. doi: 10.2217/rme-2017-0152. [DOI] [PubMed] [Google Scholar]
- 171.Pers YM, Rackwitz L, Ferreira R, Pullig O, Delfour C, Barry F, Sensebe L, Casteilla L, Fleury S, Bourin P, et al. Adipose mesenchymal stromal cell-based therapy for severe osteoarthritis of the knee: a phase I dose-escalation trial. Stem Cells Transl Med. 2016;5(7):847–856. doi: 10.5966/sctm.2015-0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Koh YG, Choi YJ. Infrapatellar fat pad-derived mesenchymal stem cell therapy for knee osteoarthritis. Knee. 2012;19(6):902–907. doi: 10.1016/j.knee.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 173.Jo CH, Lee YG, Shin WH, Kim H, Chai JW, Jeong EC, Kim JE, Shim H, Shin JS, Shin IS, et al. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells. 2014;32(5):1254–1266. doi: 10.1002/stem.1634. [DOI] [PubMed] [Google Scholar]
- 174.Chen HH, Chen YC, Yu SN, Lai WL, Shen YS, Shen PC, Lin SH, Chang CH, Lee SM. Infrapatellar fat pad-derived mesenchymal stromal cell product for treatment of knee osteoarthritis: a first-in-human study with evaluation of the potency marker. Cytotherapy. 2021;24:72–85. doi: 10.1016/j.jcyt.2021.08.006. [DOI] [PubMed] [Google Scholar]
- 175.Dilogo IH, Canintika AF, Hanitya AL, Pawitan JA, Liem IK, Pandelaki J. Umbilical cord-derived mesenchymal stem cells for treating osteoarthritis of the knee: a single-arm, open-label study. Eur J Orthop Surg Traumatol. 2020;30(5):799–807. doi: 10.1007/s00590-020-02630-5. [DOI] [PubMed] [Google Scholar]
- 176.Khalifeh Soltani S, Forogh B, Ahmadbeigi N, Hadizadeh Kharazi H, Fallahzadeh K, Kashani L, Karami M, Kheyrollah Y, Vasei M. Safety and efficacy of allogenic placental mesenchymal stem cells for treating knee osteoarthritis: a pilot study. Cytotherapy. 2019;21(1):54–63. doi: 10.1016/j.jcyt.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 177.Jo CH, Chai JW, Jeong EC, Oh S, Shin JS, Shim H, Yoon KS. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a 2-year follow-up study. Am J Sports Med. 2017;45(12):2774–2783. doi: 10.1177/0363546517716641. [DOI] [PubMed] [Google Scholar]
- 178.Davatchi F, Sadeghi Abdollahi B, Mohyeddin M, Nikbin B. Mesenchymal stem cell therapy for knee osteoarthritis: 5 years follow-up of three patients. Int J Rheum Dis. 2016;19(3):219–225. doi: 10.1111/1756-185X.12670. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.