Abstract
The prevalence of sepsis is increasing in subspecialty intensive care units, including the cardiac intensive care unit (CICU). The clinical characteristics and outcomes of CICU patients with sepsis are not well understood. We conducted a retrospective cohort study of sepsis patients in the CICU compared to other ICUs using the PROGRESS registry. CICU-sepsis patients were older with fewer acute organ failures (median 2 v. 3, p < 0.001), lower SOFA scores (median 7 v. 9, p < 0.001), and more comorbidities. The use of fluid resuscitation, mechanical ventilation, and renal replacement were similar. Mortality was 47.3% for CICU-sepsis patients compared to 43.6% for sepsis patients in other ICU (P = 0.37). We conclude that, in a prior cohort of septic patients, sepsis in CICU patients had outcomes that are comparably poor to sepsis in other ICUs. Septic CICU patients presented with fewer acute organ failures, but more chronic comorbidities. Contemporary data as well as novel interventions and investigations targeted specifically to cardiac patients with sepsis should be prioritized.
Keywords: Sepsis, Cardiology, Critical care, Cardiac intensive care unit, Shock
1. Introduction
The epidemiology of patients in the contemporary cardiac intensive care unit (CICU) is changing, and CICU patients present with an increasing frequency of non-cardiac critical illness syndromes including severe sepsis [1]. Cardiac patients with severe sepsis have a higher frequency of conditions that could impact sepsis management particularly heart failure, valvular disease, arrhythmias, and ischemic heart disease [2], [3], [4]. Moreover, cardiac patients with severe sepsis may have sepsis sources that differ from other populations. It is not known whether current paradigms and guidelines for sepsis management [5] apply to cardiac patients with severe sepsis. Understanding the similarities and differences of septic patients in the CICU compared to other ICU's is important to understand whether guidelines and quality metrics promulgated for sepsis patients in general should apply to septic cardiac patients5. Such knowledge is also important for CICU performance benchmarking and to design future studies of sepsis therapeutics in patients with underlying cardiac disease.
To inform future studies and hypotheses regarding septic CICU patients, we compared CICU patients with sepsis to the general population of sepsis patients using the PROGRESS registry [6]. We hypothesized that, historically, demographics, source of sepsis and management strategies would differ substantially for septic cardiac patients and that outcomes will be worse with higher rates of in-hospital mortality.
2. Methods
The Promoting Global Research Excellence in Severe Sepsis (PROGRESS) registry collected data between December 2002 and December 2005 to characterize sepsis management and outcomes internationally. All enrolled patients had clinical evidence of infection and at least one organ dysfunction treated in an ICU. The study duration was from the onset of sepsis until hospital discharge. The exposure variable of interest was admission to a CICU for severe sepsis compared to any other ICU. The primary outcome was in-hospital mortality. We compared demographics and clinical characteristics across categorical categories of the exposure variable using the Wilcoxon rank-sum test for continuous variables and the Chi Square test for categorical variables. We used logistic regression to determine the association of CICU admission with mortality adjusting for demographics and degree of critical illness. We also completed a time to event analysis using the Kaplan Meier method for the primary outcome across ICU exposure categories. Lastly, we performed a sensitivity analysis including only sepsis patients treated in medical versus cardiac ICUs (excluding surgical and mixed ICUs).
3. Results
Of 276 centers in the PROGRESS study, 16 of the ICUs (4.8%) were identified as CICUs. 49.3% of the ICUs were mixed medical and surgical units. Of the 13,785 patients identified with sepsis, 148 were cared for in a CICU. Compared to non-CICU sepsis patients, CICU-sepsis patients were older, more likely to be of white race with a lower median number of acute organ dysfunctions and lower SOFA score [Table 1]. Findings were similar in comparing CICU patients to 2840 sepsis patients admitted to medical ICUs (versus surgical or mixed ICUs).
Table 1.
Demographic and clinical characteristics and outcomes of sepsis patients in the CICU compared to other ICUs.
| Non-CICU | CICU | P | |
|---|---|---|---|
| N | 13,637 | 148 | |
| Age (years) | 63 (49–74) | 69 (57–78) | <0.0001 |
| Female sex | 5511 (40.4) | 72 (48.7) | 0.042 |
| Race-ethnicity | <0.0001 | ||
| African | 232 (1.7) | 16 (10.8) | |
| Caucasian | 5963 (43.7) | 84 (56.8) | |
| E-SE Asian | 2325 (17.1) | 13 (8.8) | |
| Hispanic | 2706 (19.8) | 6 (4.1) | |
| W Asian | 726 (5.2) | 3 (2.0) | |
| Other/unknown | 368 (2.7) | 26 (17.6) | |
| SIRS temperature criterion | 10,192 (74.4) | 113 (76.4) | 0.65 |
| SIRS heart rate criterion | 12,266 (90.0) | 133 (89.9) | 0.97 |
| SIRS respiratory rate criterion | 11,919 (87.4) | 138 (93.2) | 0.033 |
| SIRS leukocyte criterion | 11,256 (82.5) | 116 (78.4) | 0.19 |
| Number of SIRS criteria | 4 (3–4) | 4 (3–4) | 0.61 |
| Proven infection | 9253 (67.9) | 94 (63.5) | 0.26 |
| Acute organ dysfunction | |||
| Circulatory dysfunction | 10,158 (74.5) | 103 (69.6) | 0.18 |
| Respiratory dysfunction | 11,099 (81.4) | 118 (79.7) | 0.61 |
| Hematologic dysfunction | 4615 (33.8) | 39 (26.4) | 0.055 |
| Renal dysfunction | 6209 (45.5) | 55 (37.2) | 0.042 |
| Hepatic dysfunction | 2603 (19.1) | 15 (10.1) | 0.006 |
| Metabolic abnormality | 5914 (43.4) | 29 (19.6) | <0.001 |
| CNS dysfunction | 4488 (32.9) | 30 (20.3) | 0.001 |
| Total number of organ dysfunctions | 3 (2–4) | 2 (1–4) | <0.0001 |
| SOFA scorea | 9 (7–12) | 7 (5–9) | <0.0001 |
| Site of infection | <0.001 | ||
| Abdominal-pelvic | 3101 (22.7) | 14 (9.5) | |
| Bone/joint | 194 (1.4) | 1 (0.7) | |
| Hematogenous spread | 823 (6.0) | 13 (8.8) | |
| Indwelling vascular catheter | 201 (1.5) | 1 (0.7) | |
| Lung | 6227 (45.7) | 76 (51.4) | |
| CNS | 208 (1.5) | 0 (0) | |
| Skin | 697 (5.1) | 4 (2.7) | |
| Urinary tract | 1029 (7.6) | 27 (18.2) | |
| Other/unknown | 697 (5.1) | 4 (2.7) | |
| Fungal infection | 1222 (9.0) | 15 (10.1) | 0.62 |
| Gram positive infection | 4492 (32.9) | 44 (29.7) | 0.41 |
| Gram negative infection | 5721 (42.0) | 52 (35.1) | 0.095 |
| Viral infection | 182 (1.3) | 1 (0.7) | 0.49 |
| Comorbidities | |||
| Chronic lung disease | 2291 (16.8) | 39 (26.4) | 0.002 |
| Congestive heart failure | 1909 (14.0) | 41 (27.7) | <0.001 |
| CKD | 1431 (10.5) | 27 (18.2) | 0.002 |
| Chronic liver disease | 851 (6.2) | 10 (6.8) | 0.8 |
| Diabetes | 2916 (21.4) | 33 (22.3) | 0.79 |
| Active cancer | 2005 (14.7) | 13 (8.8) | 0.043 |
| Chronic steroid use | 1258 (9.2) | 12 (8.1) | 0.64 |
| ICU therapies | |||
| Albumin | 2604 (19.1) | 67 (45.3) | <0.001 |
| Fluid resuscitation | 10,733 (78.7) | 116 (78.4) | 0.92 |
| Mechanical ventilation | 11,646 (85.4) | 119 (80.4) | 0.087 |
| Renal replacement therapy | 2846 (20.9) | 39 (26.4) | 0.1 |
| Sedation | 9419 (69.07) | 104 (70.3) | 0.75 |
| Source control procedure | 4944 (36.3) | 25 (16.9) | <0.001 |
| Vasopressors | 10,712 (78.6) | 101 (68.2) | 0.002 |
| ICU length of stay | 10 (5–18) | 10 (4–20) | 0.8 |
| Hospital length of stay | 19 (10–36) | 17 (9–33) | 0.15 |
| Death in ICU | 5211 (38.2) | 57 (38.5) | 0.94 |
| Death in hospital | 5946 (43.6) | 70 (47.3) | 0.37 |
(N = 5604 for non-CCU and 84 for CCU).
CICU-sepsis patients had a higher burden of chronic comorbidities including chronic lung disease, congestive heart failure, and chronic kidney disease compared to sepsis patients in other ICUS [Table 1].
The source of sepsis was different between CICU-sepsis and non-CICU septic patients: patients in the CICU were more likely to have primary lung infections, urinary tract infections, and bloodstream infections. They were less likely to have abdominal-pelvic and skin infections [Table 1]. Treatments for CICU-sepsis patients and non-CICU patients are displayed in the Table 1; substantial fractions of both groups required fluid resuscitation, mechanical ventilation, renal replacement therapy and sedation. Fewer patients in the CICU required procedures for source control (16.9% vs. 36.4%; p < 0.001) and fewer needed treatment with vasopressors (68.2% vs. 78.6%; p = 0.002).
Hospital and ICU length of stay were long and similar in both groups. Mortality was high and similar in both groups: In-hospital mortality for septic patients in the CICU was 47.3% compared to 43.6% in other ICUs (p = 0.37; Table 1, Fig. 1). Findings were similar when comparing CICU-sepsis patients to only MICU sepsis patients (mortality 47.3% vs. 43.9% p = 0.41). There was a greater unadjusted hazard ratio for death in CICU-sepsis patients (HR 1.28, 95% CI 1.01–1.63, p = 0.045) with qualitative divergence of the Kaplan-Meier curve later in the hospital course (Fig. 1). After adjusting for age, sex, and chronic co-morbidities (chronic lung disease, chronic kidney disease and congestive heart failure history), CICU and other ICU patients with sepsis had similar outcomes (HR 1.18, 95% CI 0.92–1.50, p = −0.19). Similarly, the association of CICU admission with mortality attenuated after adjusting for age alone (HR 1.21 95% CI 0.95–1.54, p = 0.13). In comparing CICU patients to MICU-only sepsis patients, the unadjusted hazard ratio for death in CICU patients with sepsis was 1.14 (95% CI 0.89–1.46, p = 0.29).
Fig. 1.
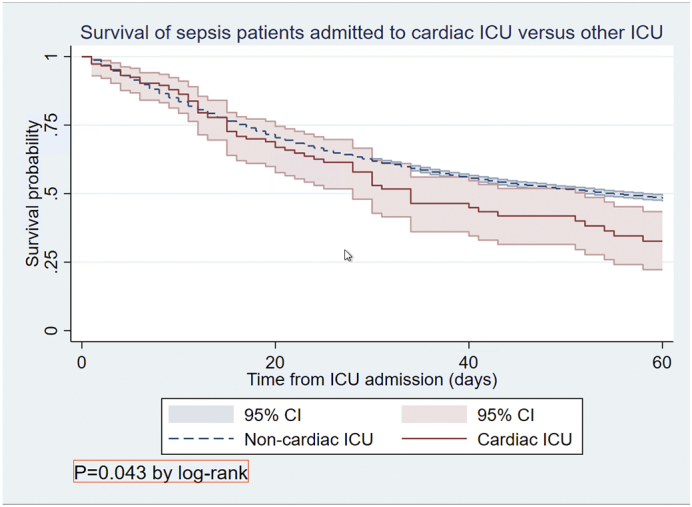
Survival of sepsis patients in the CICU compared to other ICU. There was a greater unadjusted hazard ratio for death in CICU-sepsis patients (HR 1.28, 95% CI 1.01–1.63, p = 0.045) which attenuated after adjusting for age, sex, chronic lung disease, chronic kidney disease and congestive heart failure history (HR 1.18, 95% CI 0.92–1.50, p = −0.19).
An increased number of SIRS criteria was associated with mortality in other ICU sepsis patients (HR 1.17, 95% CI 1.13–1.21, p < 0.001) but not in CICU-sepsis patients (HR 0.87, 95% CI 0.63–1.18, p = 0.37). The SOFA score was associated with mortality in other ICU sepsis patients (HR 1.10, 95% CI 1.09–1.11, P < 0.001), but not in CICU-sepsis patients (HR 1.07, 95% CI 0.97–1.19, p = 0.18).
4. Discussion
The clinical landscape in the CICU is changing [3], [4], and management of patients with acute non-cardiac critical illness in the cardiac ICU is increasingly important in CICU practice. We report the clinical characteristics, management, and outcomes of CICU patients with sepsis, in a historical international registry. We report several major findings. First, CICU patients with sepsis in this cohort had a different clinical profile than the general population of patients with sepsis, characterized by fewer acute organ failures and more chronic comorbidity. Second, CICU sepsis patients in the past required large amounts of general critical care resources and had similarly poor outcomes compared to the general sepsis population. Finally, the predictive value of scoring systems differed across septic CICU patients and non-CICU patients.
We characterize the phenotype of septic CICU patients as distinct from that present in other ICUs with greater frequency of chronic comorbidities, in a historical cohort. Other investigators have also documented the rise of chronic comorbidities in contemporary CICU populations [1], [7]. Our concurrent finding that these patients have fewer acute organ failures than non-CICU sepsis patients supports the paradigm that in patients with chronic comorbidities a lesser degree of acute illness suffices to require ICU admission for sepsis. Chronic comorbidities or older age alone could also contribute to the later divergence of survival curves that we observe. In such patients, management of the acute organ failure is necessary, yet insufficient, to improve outcomes highlighting the need to address chronic and acute-on-chronic illnesses.
Septic CICU patients required significant ICU resources. This is consistent with our results as well as with prior studies placing CICU patients on a spectrum of general critical care [2], [3]. The clinician expertise needed to care for such patients requires skill in critical care as well as cardiology. A variety of ICU staffing patterns has been recently described to meet this complex population's needs [4]. The critical care needs of the CICU-sepsis population support development of novel training pathways [8] for current trainees and collaborative care pathways in critical care for active CICU clinicians.
We report that performance of risk scores including SOFA, SIRS, and the number of acute organ failures differs across CICU sepsis and non-CICU sepsis patients. This observation is important and relevant to efforts to benchmark sepsis outcomes and compare performance across ICUs. Other authors have also described reduced performance of commonly used risk scores in critically ill CICU patients [9]. Our data support the need for development of more specific risk scoring systems for CICU patients.
There are several limitations associated with our study. A significant limitation study is that The PROGRESS registry enrolled patients in 2002–2005. Since that time there have been advancements in overall management of sepsis patients through guidelines and changes to the sepsis criteria. It is not known whether similar findings would be replicated in a contemporary cohort, but this should be explored. Our findings are hypothesis generating and should inform future study design and prompt contemporary inquiry. The interventions used in this study's population have remained the tenets of sepsis care including resuscitation, identifying the site of infection, antibiotic therapy, and source control, suggesting that these data provide relevant information for ICU practice. An additional limitation is that a minority of centers included in the database identified as CICU's leading to a small sample size. Finally, the study was observational and retrospective in design, and thus is not reflective of causal mechanism.
In conclusion, in an international sepsis registry, sepsis patients admitted to the CICU had a phenotype reflecting a high burden of chronic comorbidities and fewer acute organ failures compared to the general sepsis population. CICU-sepsis patients had a high burden of critical care needs with poor outcomes. Our results support sepsis in the CICU as a high-risk phenotype and points to the need for contemporary dedicated research in this specific patient population.
Sources of funding
Dr. Metkus is supported the National Institutes of Health-funded Institutional Career Development Core at Johns Hopkins (project number 5KL2TR003099-02).
CRediT authorship contribution statement
Elizabeth Willa Feldman: Investigation, Formal analysis, Writing – original draft, Writing – review & editing. Eunice Dugan: Investigation, Data curation, Formal analysis, Writing – review & editing. Robert Scott Stephens: Writing – review & editing, Supervision. Steven Schulman: Writing – review & editing, Supervision. Sammy Zakaria: Writing – review & editing, Supervision. Thomas Metkus: Conceptualization, Methodology, Supervision, Writing – review & editing, Funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This publication is based on research using data from data contributor Lilly that has been made available through Vivli, Inc. Vivli has not contributed to or approved, and is not in any way responsible for, the contents of this publication.
References
- 1.Jentzer J.C., van Diepen S., Barsness G.W., et al. Changes in comorbidities, diagnoses, therapies and outcomes in a contemporary cardiac intensive care unit population. Am. Heart J. 2019;215:12–19. doi: 10.1016/j.ahj.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 2.Bohula E.A., Katz J.N., van Diepen S., et al. Demographics, care patterns, and outcomes of patients admitted to cardiac intensive care units: the critical care cardiology trials network prospective north american multicenter registry of cardiac critical illness. JAMA Cardiol. 2019;4(9):928–935. doi: 10.1001/jamacardio.2019.2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morrow D.A., Fang J.C., Fintel D.J., et al. Evolution of critical care cardiology: transformation of the cardiovascular intensive care unit and the emerging need for new medical staffing and training models: a scientific statement from the American Heart Association. Circulation. 2012;126(11):1408–1428. doi: 10.1161/CIR.0b013e31826890b0. [DOI] [PubMed] [Google Scholar]
- 4.Katz J.N., Minder M., Olenchock B., et al. The genesis, maturation, and future of critical care cardiology. J. Am. Coll. Cardiol. 2016;68(1):67–79. doi: 10.1016/j.jacc.2016.04.036. [DOI] [PubMed] [Google Scholar]
- 5.Levy M.M., Evans L.E., Rhodes A. The surviving sepsis campaign bundle: 2018 update. Intensive Care Med. 2018;44(6):925–928. doi: 10.1007/s00134-018-5085-0. [DOI] [PubMed] [Google Scholar]
- 6.Beale R., Reinhart K., Brunkhorst F.M., et al. Promoting global research excellence in severe sepsis (PROGRESS): lessons from an international sepsis registry. Infection. 2009;37(3):222–232. doi: 10.1007/s15010-008-8203-z. [DOI] [PubMed] [Google Scholar]
- 7.Sinha S.S., Sjoding M.W., Sukul D., et al. Changes in primary noncardiac diagnoses over time among elderly cardiac intensive care unit patients in the United States. Circ. Cardiovasc. Qual. Outcomes. 2017;10(8) doi: 10.1161/CIRCOUTCOMES.117.003616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Gara P.T., Adams J.E., 3rd, Drazner M.H., et al. COCATS 4 task force 13: training in critical care cardiology. J. Am. Coll. Cardiol. 2015;65(17):1877–1886. doi: 10.1016/j.jacc.2015.03.027. [DOI] [PubMed] [Google Scholar]
- 9.Jentzer J.C., van Diepen S., Murphree D.H., et al. Admission diagnosis and mortality risk prediction in a contemporary cardiac intensive care unit population. Am. Heart J. 2020;224:57–64. doi: 10.1016/j.ahj.2020.02.018. [DOI] [PubMed] [Google Scholar]


