Figure 5. Example of how thiopurine treatment and MMR deficiency cooperate to induce a TP53 driver mutation.
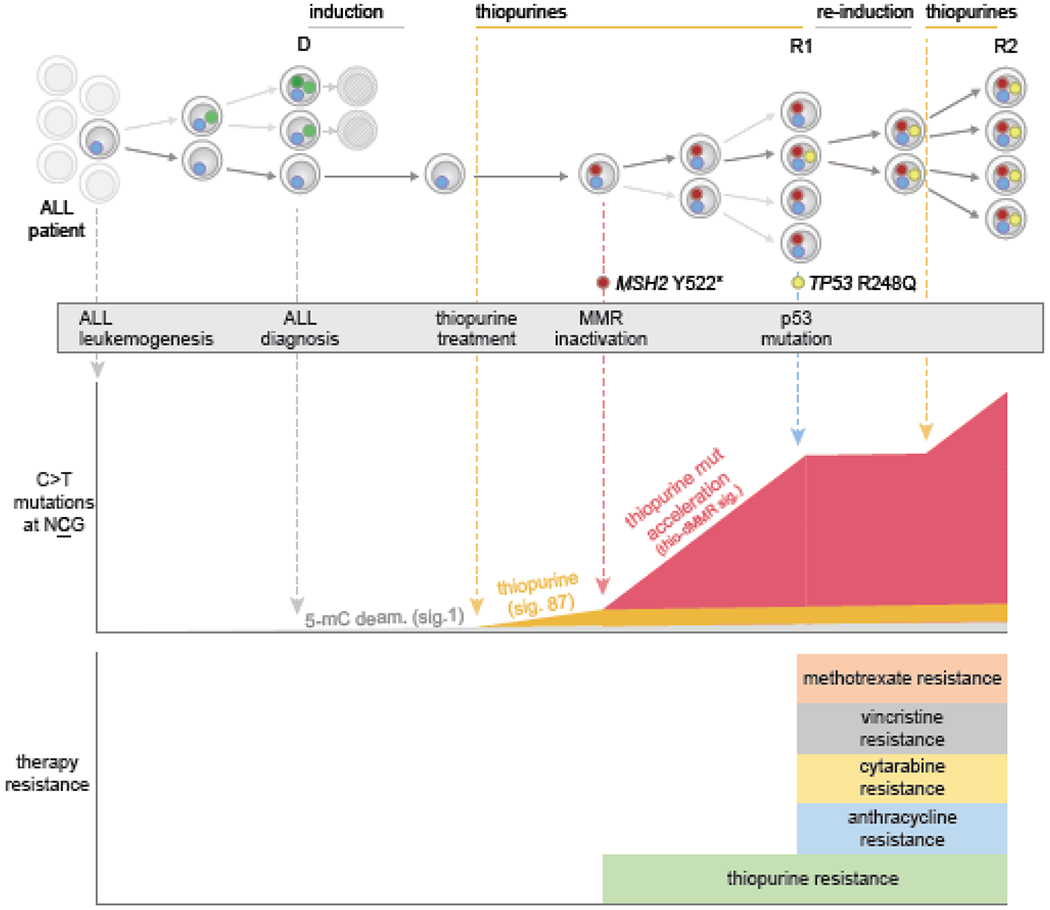
This shows a specific ALL patient analyzed by WGS at diagnosis and through multiple relapses, from a previous study [69]. Individual ALL clones are shown as cells harboring specific mutations (small colored circles), and time goes from left (ALL initiation) to right (through to second relapse). Initial therapy eliminated multiple clones, but the first relapse (R1) acquired MSH2 mutation leading to MMR deficiency. The resulting MMR deficiency enhanced the rate of mutation by thiopurine treatment approximately 10-fold (orange signature originally, in middle panel, to red signature with enhanced rate). Thiopurines induce C>T mutations at NCG contexts, increasing the probability of a TP53 R248Q mutation, which is of this C>T at NCG mutation class. Indeed, a subclonal TP53 R248Q mutation was present at a low level at R1, which was likely induced by thiopurines after the MSH2 mutation occurred (based on experimental and patient analysis). TP53 mutations cause resistance to induction and re-induction therapies, including resistance to anthracyclines, vincristine, and other drugs (see bottom), resulting in a multi-drug resistant clone which became dominant at second relapse (R2). Thus, thiopurine treatment can induce important drug resistance mutations that lead to more aggressive disease, and this process is more likely in MMR-deficient clones which are unable to repair thiopurine mismatches incorporated into DNA.
