Abstract
Objectives
Fairness is a core concept meant to grapple with different forms of discrimination and bias that emerge with advances in Artificial Intelligence (eg, machine learning, ML). Yet, claims to fairness in ML discourses are often vague and contradictory. The response to these issues within the scientific community has been technocratic. Studies either measure (mathematically) competing definitions of fairness, and/or recommend a range of governance tools (eg, fairness checklists or guiding principles). To advance efforts to operationalise fairness in medicine, we synthesised a broad range of literature.
Methods
We conducted an environmental scan of English language literature on fairness from 1960-July 31, 2021. Electronic databases Medline, PubMed and Google Scholar were searched, supplemented by additional hand searches. Data from 213 selected publications were analysed using rapid framework analysis. Search and analysis were completed in two rounds: to explore previously identified issues (a priori), as well as those emerging from the analysis (de novo).
Results
Our synthesis identified ‘Three Pillars for Fairness’: transparency, impartiality and inclusion. We draw on these insights to propose a multidimensional conceptual framework to guide empirical research on the operationalisation of fairness in healthcare.
Discussion
We apply the conceptual framework generated by our synthesis to risk assessment in psychiatry as a case study. We argue that any claim to fairness must reflect critical assessment and ongoing social and political deliberation around these three pillars with a range of stakeholders, including patients.
Conclusion
We conclude by outlining areas for further research that would bolster ongoing commitments to fairness and health equity in healthcare.
Keywords: artificial intelligence, machine learning, health equity, health services research, patient-centered care
Introduction
Automated-decision-making systems in medicine (often machine-learning or ML-based) represent an emergent medical and technological innovation we call ‘Predictive Care’. Predictive care combines Big Data (on whole populations) and Small Data (on single people) to facilitate proactive, precise, and personalised health interventions. It is widely viewed as the ML tool with the most promise to solve some of the most complex and intractable problems in healthcare.1 However, according to recent scholarship on algorithmic injustice, there is growing evidence to suggest that ML tools amplify existing inequities, such as racial bias, often because they are trained on biased datasets.2–5 Therefore, implementation in clinical contexts is concerning because predictive care systems have the potential to discriminate against people based on sociodemographic characteristics such as age, sex or race.6 These concerns have led to explosive growth in ‘fairness-aware ML,’ a new field that aims to design fair algorithmic systems1 by detecting and eliminating bias.7 8
In ML discourses, the notion of fairness appeared briefly in the late 1960s as a shorthand for a range of procedural and statistical methods designed to track and measure different forms of discrimination.9–11 Rediscovered recently12 most current approaches to fairness are technocratic.13 Studies either approach fairness as a set of (mathematical) techniques,14 and/or recommend a set of governance procedures that can be used to mitigate against any unintended harms (eg, fairness checklists or guiding principles).15 However, it remains unclear how exactly current approaches to fairness map onto established ethical frameworks.7 16–19 For example, the narrow definition of fairness in ML discourses does not fully engage with fairness as an idiom, or a mode of expression used to resolve public debates and emotional tensions that emerge alongside questions about what it means to build a good and just society.20–23 Nor do these techniques or procedures fully address debates about who should/will benefit the most from these advances and why.19 24–33 Finally, it remains unclear how or which notions of fairness might be used to advance health equity.34 However, without conceptual clarity, attempts to operationalise fairness will be spurious.
To advance efforts to operationalise fairness in medicine, we synthesised a broad range of literature on fairness in medical algorithms. The results of our synthesis identified three pillars of fairness: transparency, impartiality and inclusion. We draw on these insights to propose a multidimensional conceptual framework to guide empirical research on the operationalisation of fairness in healthcare. We conclude by applying these three pillars to a case use scenario, drawing on examples from psychiatry. Although predictive care systems are not yet widely employed in psychiatry,35 models to predict suicide,36 psychiatric readmission,37 and inpatient violence are in high demand.38 39 However, the performance of these models are often limited; for instance, most individuals identified with ML as being at high risk do not become violent,40 introducing a strong potential for bias in false positive predictions for certain groups. Although the future implementation of predictive care models is motivated by the provision of safer and more efficient care, biased predictions can perpetuate health inequities. Thus, predictive care in psychiatry offers a timely example for illustrating the value of our three pillars in advancing the operationalisation of fairness in healthcare. Our overall aim is to invite discussion and spur innovative solutions.
Methodology: what’s fair?
The planning phase of this research included a medical anthropologist (LS) and a computational neuroscientist (SLH). We noted that there are few scholarly works devoted exclusively to understanding what it means to be fair or unfair (for exceptions41–43). We hypothesised that this may be because fairness is what sociolinguists call a ‘strategically deployable shifter’.44 The meaning of any shifter depends on how the concept is used, by whom and in what context. Shifters are identifiable because they are often used by both critics and their intended targets. For example, developers of a predictive care model can claim it is “fair” because it pairs most patients with appropriate interventions. Detractors can claim it is ‘unfair’ because most patients paired with inappropriate interventions belong to protected groups, or a category of people protected by law, policy or similar authority.45 46 Therefore, our research question for this review was: how do different disciplines define and operationalise fairness in relation to ML in healthcare?
Many health systems are poised to implement the use of Big Data and ML in medicine. Yet, few studies exist that describe the outcome or impact of predictive care tools on the diagnosis, treatment and lived experience of illness. Therefore, we chose an environmental scan over a systematic review so we could survey, document and interpret commonly cited dimensions of fairness related to the use of ML in healthcare in a timely manner.47 It is particularly useful in contexts where data acquisition is necessary to identify emerging trends in a rapidly evolving research field.48 Our aim was to foster the responsible interpretation and use of knowledge derived from advances in ML and to ensure that policy uptake is relevant and beneficial for all (see online supplemental appendix 1 for more details).
bmjhci-2021-100459supp001.pdf (199.1KB, pdf)
Results
Our synthesis of the literature identified three dimensions related to fairness: transparency, impartiality, and inclusion. Each of these dimensions had intertwined attributes (see figure 1). The majority of the literature examined one or two of these pillars in relation to ML in healthcare, while few reported on all three. Rather than report raw numbers, we have indicated the degree to which each dimension of fairness is considered by a discipline (table 1). While not assessing the quality of the studies we extracted, this approach highlights current gaps in the fairness and ML literature. For example, computational scientists were preoccupied with ‘bias’ and ‘bias detection’ (eg, provenance), social scientists with transparency and accountability, whereas clinicians were most concerned with implementation (table 1).
Figure 1.
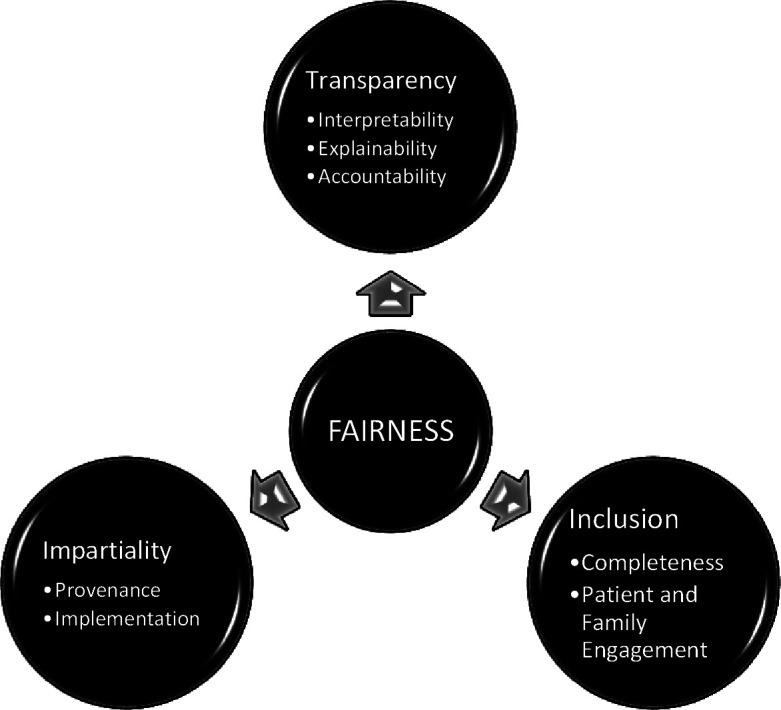
Three pillars of fairness.
Table 1.
Key dimension of fairness in the literature review by discipline (n=213)
| Research field | Fairness dimension | Specific attribute | Volume of articles by specific attributes |
| Computational sciences (n=68) |
Transparency Impartiality Inclusion |
Interpretability/explainability Accountability Provenance Implementation Completeness Patient and family engagement |
+ + + + + + + + + + + + + |
| Medicine (n=43) |
Transparency Impartiality Inclusion |
Interpretability/explainability Accountability Provenance Implementation Completeness Patient and family engagement |
+ + + + + + + + + + + + + + + |
| Social sciences (n=73) |
Transparency Impartiality Inclusion |
Interpretability/explainability Accountability Provenance Implementation Completeness Patient and family engagement |
+ + + + + + + + + + + + + + + + + + |
| Interdisciplinary research teams (n=29) |
Transparency Impartiality Inclusion |
Interpretability/explainability Accountability Provenance Implementation Completeness Patient and family engagement |
+ + + + + + + + + + + + + + |
++++The majority of the literature reviewed in this field.
+++Several peer reviewed articles (five or more).
++A small number of peer reviewed articles (less than five).
+Little or no known literature (two or less).
Three pillars for fairness and health equity
Although the literature we reviewed details a range of dimensions related to fairness, there is no single conceptual framework that integrates all of them. This article aims to address this gap through developing a conceptual framework for fairness we call ‘Three Pillars for Fairness and Health Equity’ (see table 2). Below we describe each of these pillars in turn and pay specific attention to the relationship between medical algorithms, predictive care and health equity.
Table 2.
Three pillars for fairness
| Fairness pillar | Source of unfairness | Challenge: | Attribute | Key questions |
| Transparency: A range of methods designed to see, understand and hold complex algorithmic systems accountable in a timely fashion. | ‘Like Gods, these mathematical models were opaque, their workings invisible to all but the highest priests in their domain: mathematicians and computer scientists’ (O’Neil: 3) | How can we foster democratic and sustained debate on the role of AI/ML in healthcare with a range of stakeholders, including patients experiencing complex and serious mental illness and/or addiction? | Interpretable | Are biases from predictive care models carried over across samples and settings? |
| Explainable | Which model features are contributing to bias and what kinds of assumptions do they amplify? How does an understanding of these features by stakeholders impact clinical care? | |||
| Accountable | How does predictive care impact stakeholders (patients, families, nurses, social workers)? What governance structures are in place to ensure fair development and deployment? Who is responsible for identifying and reporting potential harms? | |||
| Impartiality: Health care should be free from unfair bias and systemic discrimination. | ‘AI can help reduce bias, but it can also bake in and scale bias’ (Silberg and Manyika:2) | How are complex social realities transformed into algorithmic systems, and what kinds of normative assumptions drive these processes? |
Provenance | Do predictive care model features reflect socio-economic and political inequities? Might these features contribute to biased performance? |
| Implementation | What harms might result from the implementation of predictive care models? Do they disproportionately affect certain groups? | |||
| Inclusion: The process of improving the ability, opportunity, and dignity of people, disadvantaged on the basis of their identity, to access health services, receive compassionate care and achieve equitable treatment outcomes. | ‘Randomised trials estimate average treatment effects for a trial population, but participants in clinical trials often aren’t representative of the patient popuation that ultimately receives the treatment’ (Chen: 167). | How can we ensure that the benefits of advances in clinical AI accrue to the most structurally disadvantaged? | Completeness | Is information required to detect bias missing? Is there sufficient data to evaluate predictive care models for intersectional bias? Are marginalised groups involved in the collection and use of their data? |
| Patient and Family Engagement | Have stakeholders been involved in the development and implementation of predictive care? Do patients perceive models as being fair or positively impacting their care? |
ML, machine learning.
Transparency
Transparency was cited as a key dimension of fairness with three intertwined attributes: interpretability, explainability and accountability.49–52 Each encompasses methods designed to see, understand and hold complex algorithmic systems accountable. These attributes emerge from the fact that the inner workings of most algorithmic systems are invisible to all but the ‘highest priests in their domain: mathematicians and computer scientists,’ often making their verdicts, even when harmful, beyond dispute or appeal (O’Neil 2016:3).33 53 54 Thus, transparency requires that the actions of scientists are easy to assess,55–57 ensuring that stakeholders can decide whether they support the intentions, indications for use, and goals of any algorithmic system.58 59 However, the opacity of algorithmic systems requires that we revisit our expectations for transparency in predictive care. For example, novel approaches in ML, such as enhancing feature representations with latent embeddings or applying neural networks, can improve our ability to predict important health outcomes,60 but they also make models less transparent. Thus, there is a need to establish the degree to which we must be able to interpret and explain model results to clinicians, patients, and families. Crucially, the ability to see inside a system should not be conflated with the ability to govern it.50 61
Interpretability and explainability
In the literature we reviewed, interpretability and explainability are often used interchangeably.49 However, interpretability most often refers to procedures and statistical techniques primarily used by scientists, to test, validate, and replicate findings.62 In ML, this involves evaluation metrics (eg, accuracy, sensitivity, specificity), which can be used to compare performance across protected groups.12 34 However, a predictive care model achieving similar performance across samples or settings is interpretable but not necessarily fair. If a predictive care model is biased against a sociodemographic group, this bias may carry over or be amplified in a different setting or sample.63–66 Moreover, as described by the ‘impossibility theorem,’ not all fairness criteria can be satisfied at the same time.6 16 67 For example, a predictive care model can achieve high accuracy (and therefore be interpretable and statistically fair) but can still be discriminatory.68 69
This limitation of interpretability may be addressed by explainability, which in part involves understanding how model features contribute to prediction. Various technical tools and procedures exist to address concerns about the so-called ‘black box problem’ of algorithmic systems, such as techniques to identify how models weigh features.70 71 In the context of fairness however, explainability is only useful if highly-weighted features point to sociodemographic biases in model performance. For example, it may be possible to identify potential sources of bias in a predictive care model by examining whether the nature or availability of important features differ between sociodemographic groups. Moreover, in the literature we reviewed, explainability was also often used to draw attention to the social and communicative processes that surround predictive care tools. For example, these studies emphasised that fairness was not just about conveying accurate and unbiased information, but also about communicating the purpose, relevance and limitations of an algorithmic systems.72–74
Even if explainability is possible, it may not yield desirable outcomes.75 76 According to emerging evidence, many clinicians are susceptible to following incorrect diagnostic advice.77 This effect is more pronounced when ML-based advice is paired with explanations of features contributing to prediction,78 suggesting that explainability can adversely impact clinical decision making.79 Further, the ability to interpret and explain how a model works is not sufficient to mitigate harms. Recent studies of vaccine hesitancy and resistance to ebola campaigns emphasise that trust in public health interventions is often undermined by power differentials between patients and clinicians.5 80–83 Although little is known about how patients engage with predictive care in clinical contexts,84 sustained dialogue and shared decision-making between stakeholders that takes their concerns, desires and lived experiences seriously is critical.79 85–88 Thus, there is an urgent need to develop engaging, effective and user-friendly explanations of predictive care models for clinicians, patients, their caregivers and the general public.89 90 Explainability, therefore, must encompass both technical and social processes of translating the purpose, relevance and limitations of algorithmic systems to these various stakeholders, and providing targeted guidance on their use (eg, to complement clinical intuition, inform and negotiate care).
Accountability
Interpretability and explainability are described as prerequisites for the third transparency attribute: accountability. Accountability refers to governance structures, procedures, and tools used to evaluate and hold algorithmic systems accountable in a timely manner. Since predictive care often impacts acutely ill, marginalised or vulnerable groups, accountability cannot rest on the agency of a single person to assert their right to fair and equitable care.91 92 In other words, we cannot expect those impacted by predictive care (patients, families, nurses, social workers) to be the ones to hold it accountable. From a fairness perspective, downloading the responsibility to those primarily impacted—and potentially harmed—by the technology is also ethically worrisome as it places a disproportionate burden on these groups to mobilise change. Rather, the governance structures that measure and track algorithmic systems must operate at multiple scales and be monitored continuously.93–96 These structures should ensure that the development and implementation of predictive care is responsible and responsive to the needs and perspectives of various stakeholders.88
Impartiality
‘We shape our tools, and thereafter, our tools shape us’.97
One of the most cited dimensions of fairness is that individuals should be free from unfair bias and systemic discrimination.53 In medicine, both human and non-human actors gather, integrate and curate datasets to support care. As part of this process, (data scientists) aspire to collect unbiased data, but critics point out that data are not inherently fair, objective or impartial.19 Rather, data reflect widespread biases and historical patterns of exclusion and inequality persisting in society at large,98 99 which often extend to data on which predictive care models are trained. On the other hand, it is well documented that medical practices without algorithmic systems are far from impartial. Rather arbitrary and idiosyncratic practices in medicine frequently intersect with harmful sexist, racist and classist assumptions about patients.100 101 From this perspective, algorithmic systems may be more fair because ‘biased algorithms are easier to fix than biased people.’102–104
At first glance, it might seem like computational scientists and their critics have reached the same conclusion: that poor quality and biased data are likely to perpetuate harm. In the computational sciences, there is a growing assumption that encoding more data about a dataset’s origins (metadata) and circumstances (context) surrounding its creation will resolve these issues.1 105–111 However, as Seaver (2017:1105) and others argue, ‘context is the kind of thing that cannot be modelled’ since ‘contexts are not containers, but… relational properties occasioned through activity.’112 Rather than side with either perspective, we see this divergence as a vital opportunity for collaboration between computational and social scientists.113 114 Thus, our conceptualisation of fairness includes two crucial attributes of impartiality that warrant further attention: a dataset’s origins very broadly defined—or it’s ‘provenance’ and its end-use—or ‘implementation’.
Provenance
The view that encoding metadata will resolve issues of fairness maintains that with enough technical rigour, biases can be separated from the data, defined, contained and managed.115 Unfortunately, containing or removing bias from training data may not be possible, because biased features are often linked with other features in ways that are not apparent.105 116 Furthermore, this bias is maintained by social, technical and political systems which persist despite efforts to redress model bias with technical means.19 30 Accordingly, evidence suggests that interdisciplinary or ‘hybrid’ teams support fairness-aware ML.117 Domain experts, such as clinicians, social scientists or patient advocacy groups, have enhanced understandings of context situated bias,114 116 118 support the curation of salient axes of difference,119 and improve topic modelling and natural language processing models by aiding social bias detection.120–122 For example, ‘computational ethnography’ is an approach to fairness-aware ML that emphasises the importance of a holistic understanding of any given dataset.123 124 In sum, provenance requires more than a bias assessment that measures predictive accuracy across protected groups. In particular, far less attention has been paid to how complex social realities are transformed into algorithmic systems and the normative assumptions that drive these processes.125–127 For example, rather than define ‘fairness’ as a fixed attribute, the literature we reviewed emphasised that it is a value-laden social and political determination made by individuals or groups of people within specific contexts. A broader sociotechnical approach to provenance will further support the identification of marginalised subgroups, facilitate meaningful analysis and support fairness-aware predictive care.
Implementation
Implementation refers to integrating a predictive care model into a clinical setting. The limited evidence available suggests that it is incredibly difficult to replicate the power of a predictive algorithm in real-world settings.128–130 Significantly, potential uses of algorithmic systems in medicine are limitless. From a clinical perspective, these systems can personalise and optimise care.131 132 From a health systems perspective, they can be useful tools to support the fair allocation of limited resources.51 133 However, the integration of any algorithmic system into most clinical settings will require new workflows, which may challenge established hierarchies between doctors and nurses129 134 and redefine what makes a ‘good’ clinician.133 135–139 To fully understand the benefits or harms that could arise within algorithmic systems, it is equally important to consider at the outset of any project how it will be used, by whom, and to what end. Fair implementation foregrounds the clinical context where predictive care models are deployed.140
Inclusion
The final dimension of fairness we identified is inclusion. Among data scientists, inclusion often refers to both the representativeness of the dataset and its relative completeness (eg, how many features are filled in adequately). In other words, ‘high-quality’ data is accurate, precise, and collected from sufficiently large and representative samples.141–143 This approach is concerned with ensuring that any benefits and harms derived from advances in predictive care accrue equally/equitably across sociodemographic groups. Others argue that this approach is an ‘illusion’144 and highlight the importance of building inclusive data infrastructures that prevent the misuse and commodification of marginalised peoples’ data by supporting patient and family engagement.145–148 Combined, these attributes have the potential to hold systems accountable, prevent unintended harms, and support the design and use of robust and fair algorithmic systems that advance health equity.
Completeness
Fairness-aware ML requires access to sociodemographic data. Unfortunately, data required to measure inequities is often absent and collected inconsistently.118 149–153 Additional legal and social constraints limit access to sensitive sociodemographic data.154 In Canada, for example, the collection of race/ethnicity data in healthcare settings has been restricted due to a range of historical and socio-political forces. For example, Thompson155 illustrates how the Holocaust in the Second World War shook the foundations of the biological construction of race, which raised serious questions about the ethics of collecting this data.155 156 Significantly, limited sample sizes among marginalised groups pose a significant problem for predictive care as outputs will be biased towards the majority group.157–159 In addition, most current approaches to operationalising fairness focus only on legally protected categories, such as race or legal gender.160 Yet, sexual orientation, gender identity and disability are prototypical instances of unobserved characteristics, because they are frequently unrecorded but also fundamentally unmeasureable.161 162
Finally, these challenges are further amplified by the fact that intersectionality—overlapping systems of disadvantage related to intersecting social categories like race or gender—is critical for understanding health outcomes in relation to marginalised identities.163–167 Unfortunately, intersectional analyses are often limited by data availability; features contributing to intersectional bias may not be measured or the sizes of intersectional groups may be insufficient to generate meaningful performance metrics.168 At the same time, opacity (the ability to remain unseen by an algorithm) may have political and social value for groups under surveillance (eg, undocumented or criminalised youth).169 Therefore, while completeness entails inclusivity, inclusion should always be precipitated by dialogue and collaboration.
Patient and family engagement
As we chart the course for predictive care, we must centre the needs and lived experiences of those most likely to be impacted by ML.31 At present, there is much speculation about how predictive care might enhance or disrupt clinical care work, or the range of therapeutic procedures, processes and outcomes oriented towards ‘health and healing’ in medicine170 171 and ‘recovery’ in psychiatry.129 134 172 173 However, the research to date has minimally addressed how patients engage with predictive care. According to some studies, patients are interested in contributing to the design of these technologies and having control over the use of their data.174 Knowledge about patient engagement more broadly may be used to inform future work in this space. In particular, fair inclusion entails much more than diversifying our sampling frames. We must diversify our perspectives and ask those most impacted how predictive care (and their consequences) are experienced.
Discussion
In online supplemental appendix 2, we apply our conceptual framework to consider an urgent issue of fairness in one area of predictive care: risk assessment in inpatient psychiatric settings.38 39 Preventing and managing violence or aggression in mental healthcare is an ongoing challenge, with negative impacts on both patients and staff. Consequently, there are ongoing efforts to predict which inpatients may be at risk.38 Over the past several decades, various features have emerged as predictors of this risk.175 ML-based models trained on patient characteristics, structured assessments and clinical notes have achieved reasonable performance in predicting violence or aggression.38 40 176 While these models achieve good overall accuracy in distinguishing between individuals who may or may not become violent or aggressive, they show poor performance in identifying the small subset of individuals who will actually exhibit this behaviour. According to one study for example, only 23% of people assigned as high risk became violent,40 suggesting that many high-risk individuals are ‘false positives’. Nevertheless, no studies to date have explored whether groups defined by certain features are more likely to have this outcome, despite a strong potential for bias in this domain. In anticipation of further development and implementation of ML-based risk assessment, we demonstrate the value of employing our multidimensional framework as a heuristic tool to facilitate thoughtful and sustained dialogue on different dimensions of fairness in predictive care. In table 3, we summarise considerations related to ML-based prediction of inpatient risk for each fairness attribute. For a detailed discussion of these points, see online supplemental appendix 2.
Table 3.
The three fairness pillars, their attributes and relation to ML-based prediction of inpatient violence in psychiatric settings
| Pillar | Attribute | Relation to predictive care |
| Transparency | Interpretability | ML models achieve high accuracy in predicting violent behaviour in psychiatric settings.38 If these models achieve similar performance in new settings, they would be considered interpretable. However, if models are biased (ie, generating more false positives for inpatients defined by certain features), interpretability would be maintained even if biases carried forward to new samples.63 |
| Explainability | ML models are often trained on structured risk assessment scores.38 Scores may be biased against certain groups (eg, recent immigrants due to language barriers or cultural miscommunications), leading to biased models. Pairing predictions with feature explanations can lead clinicians to over-rely on ML models,78 which can exacerbate adverse impacts when models are biased. | |
| Accountability | ML models have been trained on actigraphy features to predict aggression in patients with dementia.178 However, patients should not be expected to advocate for themselves if models seem biased or are not generalisable, given their particularly vulnerable status. | |
| Impartiality | Provenance | Prior conviction and a diagnosis of schizophrenia are predictors of violence.38 179 Training models on these features could lead to certain groups being disproportionately classified as high-risk (eg, black men, due to residing in more policed areas,180 or being more likely misdiagnosed with schizophrenia181. Since these features are linked to other predictors, removing them does not remove model bias, nor does it address the social and political realities contributing to bias in the training data.111 182 |
| Implementation | ML modelling of violence risk is in part motivated by a desire to allocate staff resources to high-risk patients, but staff-patient interactions are known antecedents to violent behaviours.183 Most patients classified as high-risk do not become violent;40 however, pre-emptive interventions involving interactions with staff could precipitate violent behaviours. | |
| Inclusion | Completeness | A focus on legally protected categories may disregard biases related to unobserved characteristics (eg, sexual orientation or disability). Individuals with invisible or undiagnosed disabilities (eg, autism spectrum disorder) may display behaviours interpreted as precursors to violence or aggression.184–186 Additional marginalised groups might emerge when intersectional identities are taken into account. |
| Patient and family engagement | Collaboration in decision making during admission and maximising choice are important values for patients in settings where autonomy is limited.187–189 Patients may prioritise other aspects of care not captured by ML (eg, the caring relationships built with staff and peers, as compared with therapeutic interventions).190 |
ML, machine learning.
Conclusion
Our literature synthesis demonstrates that scholars and computational scientists alike must broaden their notions of fairness to examine normative assumptions about what it means to build a just society and who decides what is fair. Further, the operationalisation of fairness requires going beyond developing rigorous data processing procedures or deploying sophisticated techniques to detect, mitigate and eliminate bias in ML. Predictions can be fair (eg, accurate) and still amplify inequities.14 68 A multidimensional framework for fairness entails sustained dialogue with a range of stakeholders in the careful weighing of competing claims to fairness. It also involves proactively designing ML tools with and for marginalised and underserved communities.5 34 177 Thus, fairness is not an outcome of rigorous and thoughtful research, but the social and political process required to advance health equity.
Critically, medical algorithms are neither ‘fair’ nor ‘unfair;’ fairness is not a binary classifier. We have used our conceptual framework of fairness as a heuristic tool to surface normative values embedded into our algorithmic systems to ensure that the opportunities presented by predictive care promote health equity. Current efforts to operationalise fairness have not strengthened our ability to safeguard against the possibility that predictive care tools might ‘scale up’ health inequities, nor have they provided the means to redress these imbalances once found. Designing fairness-aware predictive care systems requires sociotechnical approaches; interdisciplinary, collaborative and patient-centred research that foregrounds power dynamics and clinical contexts will promote health equity. Further, rather than ‘de-bias’ or validate algorithms after they have been constructed, we need to pay more attention to how data are collected, what kinds of data make up larger datasets, and how data are interpreted and instrumentalised within algorithmic systems.
Footnotes
Twitter: @LauraSikstrom, @DanielZBuchman
Contributors: LS and SLH conceptualised, designed and analysed the data for this review. LS took the lead on the 'Three Pillars for Fairness' framework. MMM took the lead on the Case Scenario in Psychiatry. KH and ZF provided critical insights on the framework and the case scenario from a clinical perspective. DZB provided critical insights from bioethics on the conceptual framework and case scenario. All authors critically reviewed, edited and approved the final manuscript.
Funding: This work was supported by the Dalla Lana School of Public Health Interdisciplinary Data Science Seed Grant (DZB and SLH), AMS Fellowship in Compassion and Artificial Intelligence (DZB), Canadian Institutes of Health Research Health Systems Impact Fellowship (LS and MMM) and the Social Sciences and Humanities Research Council Insight Development Grant (LS, MMM and KH, #430-2021-01166).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Neff G. Why Big Data Won't Cure Us. Big Data 2013;1:117–23. 10.1089/big.2013.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh JP, Grann M, Fazel S. A comparative study of violence risk assessment tools: a systematic review and metaregression analysis of 68 studies involving 25,980 participants. Clin Psychol Rev 2011;31:499–513. 10.1016/j.cpr.2010.11.009 [DOI] [PubMed] [Google Scholar]
- 3.Obermeyer Z, Powers B, Vogeli C, et al. Dissecting racial bias in an algorithm used to manage the health of populations. Science 2019;366:447–53. 10.1126/science.aax2342 [DOI] [PubMed] [Google Scholar]
- 4.Chen IY, Joshi S, Ghassemi M. Treating health disparities with artificial intelligence. Nat Med 2020;26:16–17. 10.1038/s41591-019-0649-2 [DOI] [PubMed] [Google Scholar]
- 5.Benjamin R. Assessing risk, automating racism. Science 2019;366:421–2. 10.1126/science.aaz3873 [DOI] [PubMed] [Google Scholar]
- 6.Friedler SA, Scheidegger C, Venkatasubramanian S. On the (im) possibility of fairness. arXiv preprint arXiv:1609 07236, 2016. Available: https://arxiv.org/abs/1609.07236
- 7.Silberg J, Manyika J. Notes from the AI frontier: tackling bias in AI (and in humans) (June 2019), 2019. McKinsey global Institute. Available: https://www.mckinsey.com/~/media/McKinsey/Featured%20Insights/Artificial%20Intelligence/Tackling%20bias%20in%20artificial%20intelligence%20and%20in%20humans/MGI-Tackling-bias-in-AI-June-2019.pdf
- 8.Green B, Hu L. The myth in the methodology: Towards a recontextualization of fairness in machine learning. In: Proceedings of the machine learning: the debates workshop, 2018. https://econcs.seas.harvard.edu/files/econcs/files/green_icml18.pdf [Google Scholar]
- 9.Barocas S, Hardt M, Narayanan A. Fairness in machine learning. Nips tutorial 2017;1:2017. [Google Scholar]
- 10.Darlington RB. Another look at "cultural fairness"1. J Educ Meas 1971;8:71–82. 10.1111/j.1745-3984.1971.tb00908.x [DOI] [Google Scholar]
- 11.Cleary TA. Test bias: prediction of grades of Negro and white students in integrated colleges. J Educ Meas 1968;5:115–24. 10.1111/j.1745-3984.1968.tb00613.x [DOI] [Google Scholar]
- 12.Dwork C, Hardt M, Pitassi T. Fairness through awareness. Proceedings of the 3rd Innovations in Theoretical Computer Science Conference, New York, NY, USA, 2012:214–26. [Google Scholar]
- 13.TM L, Mosse D. Rendering society technical. In: Adventures in Aidland: the anthropology of professionals in international development. 6, 2011: 57. [Google Scholar]
- 14.Chouldechova A. Fair prediction with disparate impact: a study of bias in recidivism prediction instruments. Big Data 2017;5:153–63. 10.1089/big.2016.0047 [DOI] [PubMed] [Google Scholar]
- 15.Hagendorff T. The ethics of AI ethics: an evaluation of guidelines. Minds Mach 2020;30:99–120. 10.1007/s11023-020-09517-8 [DOI] [Google Scholar]
- 16.Srivastava M, Heidari H, Krause A. Human perception of fairness: a descriptive approach to fairness for machine learning. in association for computing machinery. Proceedings of the 25th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining, New York, NY, USA, 2019:2459–68. [Google Scholar]
- 17.Zou J, Schiebinger L. Design AI so that it’s fair. Nature 2018;559:324–6. [DOI] [PubMed] [Google Scholar]
- 18.Ferryman K, Pitcan M. Fairness in precision medicine. Data & Society, 2018. Available: https://kennisopenbaarbestuur.nl/media/257243/datasociety_fairness_in_precision_medicine_feb2018.pdf
- 19.boyd danah, Crawford K. Critical questions for big data. Information, Communication & Society 2012;15:662–79. 10.1080/1369118X.2012.678878 [DOI] [Google Scholar]
- 20.Rawls J. Fairness to Goodness. Philos Rev 1975;84:536–54. 10.2307/2183853 [DOI] [Google Scholar]
- 21.Powers M. Assistant Professor of Philosophy Madison Powers. In: Social justice: the moral foundations of public health and health policy. Oxford University Press, 2006. [Google Scholar]
- 22.Nuhrat Y. Fair to swear? gendered formulations of fairness in football in turkey. Journal of Middle East Women’s Studies 2017;13:25–46. [Google Scholar]
- 23.Berliner D, Lambek M, Shweder R, et al. Anthropology and the study of contradictions. HAU: Journal of Ethnographic Theory 2016;6:1–27. 10.14318/hau6.1.002 [DOI] [Google Scholar]
- 24.Meegan D. America the fair: using brain science to create a more just nation. Cornell University Press, 2019. [Google Scholar]
- 25.Wolsink M. Wind power implementation: The nature of public attitudes: Equity and fairness instead of ‘backyard motives’. Renewable and Sustainable Energy Reviews 2007;11:1188–207. 10.1016/j.rser.2005.10.005 [DOI] [Google Scholar]
- 26.Butler R. Children making sense of economic insecurity: Facework, fairness and belonging. Journal of Sociology 2017;53:94–109. 10.1177/1440783316630113 [DOI] [Google Scholar]
- 27.Deeming C. Social democracy and social policy in neoliberal times. J Sociol 2014;50:577–600. 10.1177/1440783313492240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Benjamin R. Race after technology: Abolitionist tools for the new jim code. Soc Forces 2020;98:1–3. 10.1093/sf/soz162 [DOI] [Google Scholar]
- 29.Perez CC. Invisible women: exposing data bias in a world designed for men random house, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crawford K. Atlas of AI. Yale University Press, 2021. [Google Scholar]
- 31.Kalluri P. Don't ask if artificial intelligence is good or fair, ask how it shifts power. Nature 2020;583:169. 10.1038/d41586-020-02003-2 [DOI] [PubMed] [Google Scholar]
- 32.Katell M, Young M, Dailey D. Toward situated interventions for algorithmic equity: lessons from the field. In: Association for computing machinery. New York, NY, USA, 2020: 45–55. [Google Scholar]
- 33.Eubanks V. Automating inequality: how high-tech tools profile, police, and Punish the poor. St. Martin’s Publishing Group, 2018. [Google Scholar]
- 34.Rajkomar A, Hardt M, Howell MD, et al. Ensuring fairness in machine learning to advance health equity. Ann Intern Med 2018;169:866–72. 10.7326/M18-1990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Panch T, Mattie H, Celi LA. The "inconvenient truth" about AI in healthcare. NPJ Digit Med 2019;2:77. 10.1038/s41746-019-0155-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Belsher BE, Smolenski DJ, Pruitt LD, et al. Prediction models for suicide attempts and deaths: a systematic review and simulation. JAMA Psychiatry 2019;76:642–51. 10.1001/jamapsychiatry.2019.0174 [DOI] [PubMed] [Google Scholar]
- 37.Boag W, Kovaleva O, McCoy TH, et al. Hard for humans, hard for machines: predicting readmission after psychiatric hospitalization using narrative notes. Transl Psychiatry 2021;11:32. 10.1038/s41398-020-01104-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Suchting R, Green CE, Glazier SM, et al. A data science approach to predicting patient aggressive events in a psychiatric hospital. Psychiatry Res 2018;268:217–22. 10.1016/j.psychres.2018.07.004 [DOI] [PubMed] [Google Scholar]
- 39.Viljoen JL, Cochrane DM, Jonnson MR. Do risk assessment tools help manage and reduce risk of violence and reoffending? A systematic review. Law Hum Behav 2018;42:181–214. 10.1037/lhb0000280 [DOI] [PubMed] [Google Scholar]
- 40.Connor M, Armbruster M, Hurley K, et al. Diagnostic sensitivity of the dynamic appraisal of situational aggression to predict violence and aggression by behavioral health patients in the emergency department. J Emerg Nurs 2020;46:302–9. 10.1016/j.jen.2019.12.006 [DOI] [PubMed] [Google Scholar]
- 41.Rawls J. Justice as fairness. Philos Rev 1958;67:164–94. 10.2307/2182612 [DOI] [Google Scholar]
- 42.Carr CL. On fairness. Canadian centre for diversity and inclusion (January 2018. Routledge, 2017. [Google Scholar]
- 43.Fairness sWJ. Respect and the egalitarian ethos revisited. J Ethics 2010;14:335–50. [Google Scholar]
- 44.Silverstein M. The indeterminacy of contextualization: when is enough enough. The contextualization of language 1992;22:55–76. [Google Scholar]
- 45.Barnett L, Walker J, Nicol J. An examination of the duty to accommodate in the Canadian human rights context. Library of Parliament, 2012. [Google Scholar]
- 46.Chun J, Gallagher-Louisy C. Overview of human rights codes by Province and Territory in Canada. Canadian Centre for Diversity and Inclusion, 2018. https://ccdica/media/1414/20171102-publications-overview-of-hr-codes-byprovince-final-enpdf [Google Scholar]
- 47.Rowel R, Moore ND, Nowrojee S, et al. The utility of the environmental scan for public health practice: lessons from an urban program to increase cancer screening. J Natl Med Assoc 2005;97:527–34. [PMC free article] [PubMed] [Google Scholar]
- 48.Charlton P, Kean T, Liu RH, et al. Use of environmental scans in health services delivery research: a scoping review. BMJ Open 2021;11:e050284. 10.1136/bmjopen-2021-050284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Krishnan M. Against Interpretability: a critical examination of the Interpretability problem in machine learning. Philos Technol 2020;33:487–502. 10.1007/s13347-019-00372-9 [DOI] [Google Scholar]
- 50.Ananny M, Crawford K. Seeing without knowing: limitations of the transparency ideal and its application to algorithmic accountability. New Media Soc 2018;20:973–89. 10.1177/1461444816676645 [DOI] [Google Scholar]
- 51.Zarsky T. The trouble with algorithmic decisions: an analytic road map to examine efficiency and fairness in automated and opaque decision making. Sci Technol Human Values 2016;41:118–32. [Google Scholar]
- 52.Floridi L, Cowls J, King TC, et al. How to design AI for social good: seven essential factors. Sci Eng Ethics 2020;26:1771–96. 10.1007/s11948-020-00213-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Barocas S, Selbst AD. Big data’s disparate impact. Calif Law Rev, 2016. Available: https://heinonline.org/hol-cgi-bin/get_pdf.cgi?handle=hein.journals/calr104§ion=25
- 54.O’Neil C. Weapons of math destruction: how big data increases inequality and threatens democracy. Crown, 2016. [Google Scholar]
- 55.Sandvig C, Hamilton K, Karahalios K. Auditing algorithms: research methods for detecting discrimination on Internet platforms. Data and discrimination: converting critical concerns into productive inquiry 2014;22:4349–57. [Google Scholar]
- 56.Burrell J. How the machine ‘thinks’: Understanding opacity in machine learning algorithms. Big Data Soc 2016;3:205395171562251. 10.1177/2053951715622512 [DOI] [Google Scholar]
- 57.Lepri B, Oliver N, Letouzé E, et al. Fair, transparent, and accountable algorithmic decision-making processes. Philos Technol 2018;31:611–27. 10.1007/s13347-017-0279-x [DOI] [Google Scholar]
- 58.Char DS, Abràmoff MD, Feudtner C. Identifying ethical considerations for machine learning healthcare applications. Am J Bioeth 2020;20:7–17. 10.1080/15265161.2020.1819469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brundage M, Avin S, Wang J. Toward trustworthy AI development: mechanisms for supporting verifiable claims. arXiv, 2020. Available: https://arxiv.org/abs/2004.07213
- 60.Krompaß D, Esteban C, Tresp V, et al. Exploiting latent Embeddings of nominal clinical data for predicting Hospital readmission. KI - Künstliche Intelligenz 2015;29:153–9. 10.1007/s13218-014-0344-x [DOI] [Google Scholar]
- 61.Geiger RS. Beyond opening up the black box: investigating the role of algorithmic systems in Wikipedian organizational culture. Big Data Soc 2017;4:205395171773073. 10.1177/2053951717730735 [DOI] [Google Scholar]
- 62.Bellamy RKE, Dey K, Hind M. Ai fairness 360: an EXTENSIBLE toolkit for detecting, understanding, and mitigating unwanted algorithmic bias. Available: https://github.com/ibm/aif360
- 63.et alXu Z, Liu J, Cheng D. Assessing the Fairness of Classifiers with Collider Bias. arXiv [cs.LG], 2020. Available: http://arxiv.org/abs/2010.03933
- 64.Darlow L, Jastrzębski S, Storkey A. Latent Adversarial Debiasing: Mitigating Collider Bias in Deep Neural Networks. arXiv [cs.LG], 2020. Available: http://arxiv.org/abs/2011.11486
- 65.Prosperi M, Guo Y, Sperrin M, et al. Causal inference and counterfactual prediction in machine learning for actionable healthcare. Nat Mach Intell 2020;2:369–75. 10.1038/s42256-020-0197-y [DOI] [Google Scholar]
- 66.et alChou Y-L, Moreira C, Bruza P. Counterfactuals and Causability in Explainable Artificial Intelligence: Theory, Algorithms, and Applications. arXiv [cs.AI], 2021. Available: http://arxiv.org/abs/2103.04244
- 67.Saravanakumar KK. The Impossibility Theorem of Machine Fairness - A Causal Perspective. arXiv [cs.LG], 2020. Available: http://arxiv.org/abs/2007.06024
- 68.Kleinberg J. Inherent trade-offs in algorithmic fairness. Abstracts of the 2018 ACM International Conference 2018. https://dl.acm.org/doi/abs/10.1145/3219617.3219634 [Google Scholar]
- 69.Wang C, Han B, Patel B. In Pursuit of Interpretable, Fair and Accurate Machine Learning for Criminal Recidivism Prediction. arXiv [stat.ML], 2020. Available: http://arxiv.org/abs/2005.04176
- 70.Slack D, Hilgard S, Jia E. How can we fool lime and SHAP?Adversarial Attacks on Post hoc Explanation Methods, 2019. Available: https://openreview.net/forum?id=nTHOa8__v0B [Accessed 19 Jul 2021].
- 71.Lundberg SM, Erion G, Chen H, et al. From local explanations to global understanding with Explainable AI for trees. Nat Mach Intell 2020;2:56–67. 10.1038/s42256-019-0138-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Watson DS, Floridi L. The explanation game: a formal framework for interpretable machine learning. Synthese 2021;198:9211–42. 10.1007/s11229-020-02629-9 [DOI] [Google Scholar]
- 73.Samek W, Wiegand T, Müller K-R. Explainable Artificial Intelligence: Understanding, Visualizing and Interpreting Deep Learning Models. arXiv [cs.AI], 2017. Available: http://arxiv.org/abs/1708.08296
- 74.Gunning D, Aha D. DARPA’s explainable artificial intelligence (XAI) program. AI Mag 2019;40:44–58. [Google Scholar]
- 75.Rudin C. Stop explaining black box machine learning models for high stakes decisions and use interpretable models instead. Nat Mach Intell 2019;1:206–15. 10.1038/s42256-019-0048-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Babic B, Gerke S, Evgeniou T, et al. Beware explanations from AI in health care. Science 2021;373:284–6. 10.1126/science.abg1834 [DOI] [PubMed] [Google Scholar]
- 77.Gaube S, Suresh H, Raue M, et al. Do as AI say: susceptibility in deployment of clinical decision-aids. NPJ Digit Med 2021;4:31. 10.1038/s41746-021-00385-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jacobs M, Pradier MF, McCoy TH, et al. How machine-learning recommendations influence clinician treatment selections: the example of antidepressant selection. Transl Psychiatry 2021;11:1–9. 10.1038/s41398-021-01224-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McCradden MD. When is accuracy off-target? Transl Psychiatry 2021;11:369. 10.1038/s41398-021-01479-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kaler A. Health interventions and the persistence of rumour: the circulation of sterility stories in African public health campaigns. Soc Sci Med 2009;68:1711–9. 10.1016/j.socscimed.2009.01.038 [DOI] [PubMed] [Google Scholar]
- 81.Nations MK, Monte CM. "I'm not dog, no!": cries of resistance against cholera control campaigns. Soc Sci Med 1996;43:1007–24. 10.1016/0277-9536(96)00083-4 [DOI] [PubMed] [Google Scholar]
- 82.Fairhead J. Understanding social resistance to the Ebola response in the forest region of the Republic of guinea: an anthropological perspective. Afr Stud Rev 2016;59:7–31. 10.1017/asr.2016.87 [DOI] [Google Scholar]
- 83.Chandler C, Fairhead J, Kelly A, et al. Ebola: limitations of correcting misinformation. Lancet 2015;385:1275–7. 10.1016/S0140-6736(14)62382-5 [DOI] [PubMed] [Google Scholar]
- 84.Saha D, Schumann C, Mcelfresh D. Measuring Non-Expert Comprehension of Machine Learning Fairness Metrics. In: Iii HD, Singh A, eds. Proceedings of the 37th International Conference on Machine Learning. PMLR, 2020: 8377–87. [Google Scholar]
- 85.Kelliher A, Barry B. Designing Therapeutic Care Experiences with AI in Mind. In: 2018 AAAI Spring Symposium Series. aaai.org, 2018. Available: https://www.aaai.org/ocs/index.php/SSS/SSS18/paper/viewPaper/17585
- 86.et alAnderson A, Dodge J, Sadarangani A. Explaining Reinforcement Learning to Mere Mortals: An Empirical Study. arXiv [cs.HC], 2019. Available: http://arxiv.org/abs/1903.09708
- 87.Dodge J, Liao QV, Zhang Y. Explaining models: an empirical study of how explanations impact fairness judgment. in association for computing machinery. Proceedings of the 24th International Conference on Intelligent User Interfaces, New York, NY, USA, 2019:275–85. [Google Scholar]
- 88.Ho A. Are we ready for artificial intelligence health monitoring in elder care? BMC Geriatr 2020;20:358. 10.1186/s12877-020-01764-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hengstler M, Enkel E, Duelli S. Applied artificial intelligence and trust—The case of autonomous vehicles and medical assistance devices. Technol Forecast Soc Change 2016;105:105–20. 10.1016/j.techfore.2015.12.014 [DOI] [Google Scholar]
- 90.Peck EM, Ayuso SE, El-Etr O. Data is personal: attitudes and perceptions of data visualization in rural Pennsylvania. Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems, New York, NY, USA, 2019:1–12. [Google Scholar]
- 91.Floridi L, Cowls J, Beltrametti M, et al. AI4People-An ethical framework for a good AI Society: opportunities, risks, principles, and recommendations. Minds Mach 2018;28:689–707. 10.1007/s11023-018-9482-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Carr S. 'AI gone mental': engagement and ethics in data-driven technology for mental health. J Ment Health 2020;29:125–30. 10.1080/09638237.2020.1714011 [DOI] [PubMed] [Google Scholar]
- 93.Carroll SR, Rodriguez-Lonebear D, Martinez A. Indigenous data governance: strategies from United States native nations. Data Sci J 2019;18:31. 10.5334/dsj-2019-031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Reddy S, Allan S, Coghlan S, et al. A governance model for the application of AI in health care. J Am Med Inform Assoc 2020;27:491–7. 10.1093/jamia/ocz192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Baker DB, Kaye J, Terry SF. Governance through privacy, fairness, and respect for individuals. EGEMS 2016;4:1207. 10.13063/2327-9214.1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Eaneff S, Obermeyer Z, Butte AJ. The case for algorithmic stewardship for artificial intelligence and machine learning technologies. JAMA 2020;324:1397–8. 10.1001/jama.2020.9371 [DOI] [PubMed] [Google Scholar]
- 97.Culkin JM. J S. A SCHOOLMAN’S GUIDE TO MARSHALL McLUHAN, 1967. Available: https://www.etalon-walk.com/s/JOHN_CULKIN.pdf [Accessed 27 Oct 2021].
- 98.Noble SU. Algorithms of Oppression: how search Engines reinforce racism. NYU Press, 2018. [DOI] [PubMed] [Google Scholar]
- 99.Pierson E, Cutler DM, Leskovec J, et al. An algorithmic approach to reducing unexplained pain disparities in underserved populations. Nat Med 2021;27:136–40. 10.1038/s41591-020-01192-7 [DOI] [PubMed] [Google Scholar]
- 100.Higashi RT, Tillack A, Steinman MA, et al. The 'worthy' patient: rethinking the 'hidden curriculum' in medical education. Anthropol Med 2013;20:13–23. 10.1080/13648470.2012.747595 [DOI] [PubMed] [Google Scholar]
- 101.Oldani MJ. Uncanny scripts: understanding pharmaceutical emplotment in the Aboriginal context. Transcult Psychiatry 2009;46:131–56. 10.1177/1363461509102291 [DOI] [PubMed] [Google Scholar]
- 102.Mullainathan S. Biased algorithms are easier to fix than biased people, 2019. Ny times. Available: https://www.cis.upenn.edu/~mkearns/teaching/ScienceDataEthics/nyt.pdf
- 103.Kleinberg J, Ludwig J, Mullainathan S. A guide to solving social problems with machine learning. Harv Bus Rev, 2016. Available: https://www.homeworksmontana.com/wp-content/uploads/edd/2019/07/kleinberg_ludwig_mullainathan_2016_hbr_a_guide_to_solving_social_problems_with_machine_learning.pdf
- 104.Kleinberg J, Ludwig J, Mullainathan S, et al. Algorithms as discrimination detectors. Proc Natl Acad Sci U S A 2020;117:30096–100. 10.1073/pnas.1912790117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Dourish P. What we talk about when we talk about context. Pers Ubiquitous Comput 2004;8:19–30. 10.1007/s00779-003-0253-8 [DOI] [Google Scholar]
- 106.de Paula R, Holanda M, Gomes LSA, et al. Provenance in bioinformatics workflows. BMC Bioinformatics 2013;14 Suppl 11:S6. 10.1186/1471-2105-14-S11-S6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mayernik MS. Open data: accountability and transparency. Big Data Soc 2017;4:205395171771885. 10.1177/2053951717718853 [DOI] [Google Scholar]
- 108.Wercelens P, da Silva W, Castro K. Data Provenance Management of Bioinformatics Workflows in Federated Clouds. In: 2019 IEEE International Conference on bioinformatics and biomedicine, 2019: 750–4. [Google Scholar]
- 109.Goble C, Cohen-Boulakia S, Soiland-Reyes S, et al. Fair computational Workflows. Data Intelligence 2020;2:108–21. 10.1162/dint_a_00033 [DOI] [Google Scholar]
- 110.Leavy S, Siapera E, O’Sullivan B. Ethical Data Curation forAI: An Approach based on Feminist Epistemology and CriticalTheories of Race. aies-conference.com. Available: https://www.aies-conference.com/2021/wp-content/posters/171_%20Ethical%20Data%20Curation%20for%20AI_%20An%20Approach%20based%20on%20Feminist%20Epistemology%20and%20Critical%20Theories%20of%20Race.pdf
- 111.ES J, Gebru T. Lessons from archives: strategies for collecting sociocultural data in machine learning. arXiv [cs.LG] 2019. [Google Scholar]
- 112.Seaver N. Algorithms as culture: some tactics for the ethnography of algorithmic systems. Big Data & Society 2017. 10.1177/2053951717738104 [DOI] [Google Scholar]
- 113.Zajko M. Conservative AI and social inequality: conceptualizing alternatives to bias through social theory. AI Soc 2007. https://arxiv.org/ftp/arxiv/papers/2007/2007.08666.pdf [Google Scholar]
- 114.Neff G, Tanweer A, Fiore-Gartland B, et al. Critique and contribute: a practice-based framework for improving critical data studies and data science. Big Data 2017;5:85–97. 10.1089/big.2016.0050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mayernik MS. Metadata accounts: achieving data and evidence in scientific research. Soc Stud Sci 2019;49:732–57. 10.1177/0306312719863494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Selbst AD, Boyd D, Friedler SA. Fairness and abstraction in Sociotechnical systems. in association for computing machinery. Proceedings of the Conference on Fairness, Accountability, and Transparency, New York, NY, USA, 2019:59–68. [Google Scholar]
- 117.Cury M, Whitworth E, Barfort S. Hybrid methodology: combining ethnography, cognitive science, and machine learning to inform the development of Context-Aware personal computing and assistive technology. Ethnographic Praxis in Industry Conference Proceedings, 2019:254–81. [Google Scholar]
- 118.Mitchell S, Potash E, Barocas S, et al. Algorithmic fairness: choices, assumptions, and definitions. Annu Rev Stat Appl 2021;8:141–63. 10.1146/annurev-statistics-042720-125902 [DOI] [Google Scholar]
- 119.Trewin S, Basson S, Muller M, et al. Considerations for AI fairness for people with disabilities. AI Matters 2019;5:40–63. 10.1145/3362077.3362086 [DOI] [Google Scholar]
- 120.et alHutchinson B, Prabhakaran V, Denton E. Social Biases in NLP Models as Barriers for Persons with Disabilities. arXiv [cs.CL], 2020. Available: http://arxiv.org/abs/2005.00813
- 121.Goldenstein J, Poschmann P. Analyzing meaning in big data: performing a MAP analysis using grammatical parsing and topic modeling. Sociol Methodol 2019;49:83–131. 10.1177/0081175019852762 [DOI] [Google Scholar]
- 122.Arnold T, Fuller HJA. In search of the user’s language: Natural language processing, computational ethnography, and error-tolerant interface design. In: Advances in Usability, User Experience and Assistive Technology. Cham: Springer International Publishing, 2019: 36–43. [Google Scholar]
- 123.Abramson CM, Joslyn J, Rendle KA, et al. The promises of computational ethnography: improving transparency, replicability, and validity for realist approaches to ethnographic analysis. Ethnography 2018;19:254–84. 10.1177/1466138117725340 [DOI] [Google Scholar]
- 124.Moore RJ, Smith R, Liu Q. Using computational ethnography to enhance the curation of real-world data (RWD) for chronic pain and invisible disability use cases. SIGACCESS Access. Comput. 2020:1–7. 10.1145/3412836.3412840 [DOI] [Google Scholar]
- 125.Leahey E. Overseeing research practice: the case of data editing. Sci Technol Human Values 2008;33:605–30. [Google Scholar]
- 126.Engle SM. The social life of measurement Sally Engle Merry. published online first:, 2016. Available: http://www.americanbarfoundation.org/uploads/cms/documents/merry-lsi_forum_rev.pdf
- 127.Friedler SA, Scheidegger C, Venkatasubramanian S. The (Im)possibility of fairness: different value systems require different mechanisms for fair decision making. Commun ACM 2021;64:136–43. [Google Scholar]
- 128.Blomberg SN, Christensen HC, Lippert F, et al. Effect of machine learning on Dispatcher recognition of out-of-hospital cardiac arrest during calls to emergency medical services: a randomized clinical trial. JAMA Netw Open 2021;4:e2032320. 10.1001/jamanetworkopen.2020.32320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sendak MP, Ratliff W, Sarro D, et al. Real-World integration of a sepsis deep learning technology into routine clinical care: implementation study. JMIR Med Inform 2020;8:e15182. 10.2196/15182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Emanuel EJ, Wachter RM. Artificial intelligence in health care: will the value match the hype? JAMA 2019;321:2281–2. 10.1001/jama.2019.4914 [DOI] [PubMed] [Google Scholar]
- 131.Tomlinson A, Furukawa TA, Efthimiou O, et al. Personalise antidepressant treatment for unipolar depression combining individual choices, risks and big data (PETRUSHKA): rationale and protocol. Evid Based Ment Health 2020;23:52–6. 10.1136/ebmental-2019-300118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Thieme A, Belgrave D, Doherty G. Machine learning in mental health: a systematic review of the HCI literature to support the development of effective and Implementable ml systems. ACM Trans Comput-Hum Interact 2020;27:1–53. [Google Scholar]
- 133.Bauer M, Monteith S, Geddes J, et al. Automation to optimise physician treatment of individual patients: examples in psychiatry. Lancet Psychiatry 2019;6:338–49. 10.1016/S2215-0366(19)30041-0 [DOI] [PubMed] [Google Scholar]
- 134.Mateescu A, Elish MC. Ai in context: the labor of integrating new technologies, 2019. Available: https://www.voced.edu.au/content/ngv:81783
- 135.Kemp J, Zhang T, Inglis F, et al. Delivery of compassionate mental health care in a digital Technology-Driven age: Scoping review. J Med Internet Res 2020;22:e16263. 10.2196/16263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chin-Yee B, Upshur R. Clinical judgement in the era of big data and predictive analytics. J Eval Clin Pract 2018;24:638–45. 10.1111/jep.12852 [DOI] [PubMed] [Google Scholar]
- 137.Hunt LM, Bell HS, Baker AM, et al. Electronic health records and the disappearing patient. Med Anthropol Q 2017;31:403–21. 10.1111/maq.12375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Topol EJ. High-Performance medicine: the convergence of human and artificial intelligence. Nat Med 2019;25:44–56. 10.1038/s41591-018-0300-7 [DOI] [PubMed] [Google Scholar]
- 139.Glasziou P, Moynihan R, Richards T, et al. Too much medicine; too little care. BMJ 2013;347:f4247. 10.1136/bmj.f4247 [DOI] [PubMed] [Google Scholar]
- 140.McCradden MD, Stephenson EA, Anderson JA. Clinical research underlies ethical integration of healthcare artificial intelligence. Nat Med 2020;26:1325–6. 10.1038/s41591-020-1035-9 [DOI] [PubMed] [Google Scholar]
- 141.All of Us Research Program Investigators, Denny JC, Rutter JL, et al. The "All of Us" Research Program. N Engl J Med 2019;381:668–76. 10.1056/NEJMsr1809937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Biruk C. Seeing like a research project: producing "high-quality data" in AIDS research in Malawi. Med Anthropol 2012;31:347–66. 10.1080/01459740.2011.631960 [DOI] [PubMed] [Google Scholar]
- 143.Ghassemi M, Naumann T, Schulam P, et al. Practical guidance on artificial intelligence for health-care data. Lancet Digit Health 2019;1:e157–9. 10.1016/S2589-7500(19)30084-6 [DOI] [PubMed] [Google Scholar]
- 144.Fox K. The Illusion of Inclusion: Large Scale Genomic Data Sovereignty and Indigenous Populations. In:Association for Computing Machinery. Proceedings of the 26th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining, New York, NY, USA, 2020:3591. [Google Scholar]
- 145.Snipp CM. What does data sovereignty imply: what does it look like Indigenous data sovereignty toward an agenda, 2016: 39–55. [Google Scholar]
- 146.Kukutai T, Taylor J O. Data sovereignty for Indigenous peoples: current practice and future needs. ANU Press, 2016. [Google Scholar]
- 147.Zakaria C, Balan R, Lee Y. StressMon: scalable detection of perceived stress and depression using passive sensing of changes in work Routines and group interactions. Proc ACM Hum-Comput Interact 2019;3:1–29.34322658 [Google Scholar]
- 148.Vincent N, Li H, Tilly N. Data Leverage: A Framework for Empowering the Public in its Relationship with Technology Companies. In:Association for Computing Machinery. Proceedings of the 2021 ACM Conference on Fairness, Accountability, and Transparency, New York, NY, USA, 2021:215–27. [Google Scholar]
- 149.Pinto AD, Glattstein-Young G, Mohamed A, et al. Building a Foundation to reduce health inequities: routine collection of sociodemographic data in primary care. J Am Board Fam Med 2016;29:348–55. 10.3122/jabfm.2016.03.150280 [DOI] [PubMed] [Google Scholar]
- 150.Mc Kenzie K, Antwi BAM, Tuck A. The case for diversity, 2016. Available: https://pdfs.semanticscholar.org/ebcd/d11cd033afc93b389e8a28c331155869d0a7.pdf [Accessed 23 Mar 2021].
- 151.Kiran T, Sandhu P, Aratangy T, et al. Patient perspectives on routinely being asked about their race and ethnicity: qualitative study in primary care. Can Fam Physician 2019;65:e363–9. [PMC free article] [PubMed] [Google Scholar]
- 152.Andrus M, Spitzer E, Brown J. What We Can’t Measure, We Can't Understand: Challenges to Demographic Data Procurement in the Pursuit of Fairness. In:Association for Computing Machinery. Proceedings of the 2021 ACM Conference on Fairness, Accountability, and Transparency, New York, NY, USA, 2021:249–60. [Google Scholar]
- 153.Cristina Mora G. Making Hispanics. University of Chicago Press, 2021. [Google Scholar]
- 154.Holmes JH, Beinlich J, Boland MR, et al. Why is the electronic health record so challenging for research and clinical care? Methods Inf Med 2021;60:032–48. 10.1055/s-0041-1731784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Thompson D. The schematic state. Cambridge University Press, 2016. [Google Scholar]
- 156.Saini A. Superior: the return of race science. Beacon Press, 2019. [Google Scholar]
- 157.Treviranus J. The Value of Being Different. In: Proceedings of the 16th International Web for All Conference. New York, NY, USA: : Association for Computing Machinery 2019:1–7.
- 158.Krawczyk B. Learning from imbalanced data: open challenges and future directions. Progress in Artificial Intelligence 2016;5:221–32. 10.1007/s13748-016-0094-0 [DOI] [Google Scholar]
- 159.He H, Garcia EA. Learning from imbalanced data. IEEE Trans Knowl Data Eng 2009;21:1263–84. [Google Scholar]
- 160.Willen SS. How is health-related "deservingness" reckoned? Perspectives from unauthorized im/migrants in Tel Aviv. Soc Sci Med 2012;74:812–21. 10.1016/j.socscimed.2011.06.033 [DOI] [PubMed] [Google Scholar]
- 161.Tomasev N, McKee KR, Kay J. Fairness for Unobserved Characteristics: Insights from Technological Impacts on Queer Communities. arXiv [cs.CY], 2021. Available: http://arxiv.org/abs/2102.04257
- 162.Guo A, Kamar E, Vaughan JW. Toward fairness in AI for people with disabilities: A research roadmap. arXiv [cs.CY], 2019. Available: http://arxiv.org/abs/1907.02227
- 163.Ford CL, Airhihenbuwa CO, Theory CR. Critical race theory, race equity, and public health: toward antiracism praxis. Am J Public Health 2010;100 Suppl 1:S30–5. 10.2105/AJPH.2009.171058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Seng JS, Lopez WD, Sperlich M, et al. Marginalized identities, discrimination burden, and mental health: empirical exploration of an interpersonal-level approach to modeling intersectionality. Soc Sci Med 2012;75:2437–45. 10.1016/j.socscimed.2012.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Rosenfield S. Triple jeopardy? mental health at the intersection of gender, race, and class. Soc Sci Med 2012;74:1791–801. 10.1016/j.socscimed.2011.11.010 [DOI] [PubMed] [Google Scholar]
- 166.Buolamwini J, Gebru T. Gender Shades: Intersectional Accuracy Disparities in Commercial Gender Classification. In: Proceedings of the 1st conference on fairness, accountability and transparency. New York, NY, USA: PMLR, 2018: 77–91. [Google Scholar]
- 167.Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev 1991;43:1241. 10.2307/1229039 [DOI] [Google Scholar]
- 168.Koppe G, Meyer-Lindenberg A, Durstewitz D. Deep learning for small and big data in psychiatry. Neuropsychopharmacology 2021;46:176–90. 10.1038/s41386-020-0767-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Bratich J. Digital age| occult (ING) transparency: an Epilogue. Int J Commun Syst 2016. https://ijoc.org/index.php/ijoc/article/download/4896/1526 [Google Scholar]
- 170.Kleinman A. From illness as culture to caregiving as moral experience. N Engl J Med 2013;368:1376–7. 10.1056/NEJMp1300678 [DOI] [PubMed] [Google Scholar]
- 171.Kleinman A. The Illness Narratives: Suffering, Healing, And The Human Condition. Basic Books, 2020. [Google Scholar]
- 172.Csordas TJ, Kleinman A. The therapeutic process medical anthropology contemporary theory and method, 1996: 3–20. [Google Scholar]
- 173.Topol E. Others. The Topol Review. In: Preparing the healthcare workforce to deliver the digital future, 2019: 1–48. [Google Scholar]
- 174.Cuperfain AB, Hui K, Berkhout SG, et al. Patient, family and provider views of measurement-based care in an early-psychosis intervention programme. BJPsych Open 2021;7. 10.1192/bjo.2021.1005 [DOI] [Google Scholar]
- 175.Dack C, Ross J, Papadopoulos C, et al. A review and meta-analysis of the patient factors associated with psychiatric in-patient aggression. Acta Psychiatr Scand 2013;127:255–68. 10.1111/acps.12053 [DOI] [PubMed] [Google Scholar]
- 176.Menger V, Spruit M, van Est R, et al. Machine learning approach to inpatient violence risk assessment using routinely collected clinical notes in electronic health records. JAMA Netw Open 2019;2:e196709. 10.1001/jamanetworkopen.2019.6709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Abebe R, Barocas S, Kleinberg J. Roles for computing in social change. arXiv [cs.CY] 2019. [Google Scholar]
- 178.Khan SS, Ye B, Taati B, et al. Detecting agitation and aggression in people with dementia using sensors-A systematic review. Alzheimers Dement 2018;14:824–32. 10.1016/j.jalz.2018.02.004 [DOI] [PubMed] [Google Scholar]
- 179.Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: data from the MacArthur violence risk assessment study. Am J Psychiatry 2000;157:566–72. 10.1176/appi.ajp.157.4.566 [DOI] [PubMed] [Google Scholar]
- 180.Meerai S, Abdillahi I, Poole J. An introduction to anti-black Sanism Intersectionalities: a global Journal of social work analysis, research, Polity, and practice 2016;5:18–35. [Google Scholar]
- 181.Olbert CM, Nagendra A, Buck B. Meta-Analysis of black vs. white racial disparity in schizophrenia diagnosis in the United States: do structured assessments attenuate racial disparities? J Abnorm Psychol 2018;127:104–15. 10.1037/abn0000309 [DOI] [PubMed] [Google Scholar]
- 182.Kohler-Hausmann I. Eddie Murphy and the dangers of counterfactual causal thinking about detecting racial discrimination. Nw UL Rev 2018;113:1163. [Google Scholar]
- 183.Papadopoulos C, Ross J, Stewart D, et al. The antecedents of violence and aggression within psychiatric in-patient settings. Acta Psychiatr Scand 2012;125:425–39. 10.1111/j.1600-0447.2012.01827.x [DOI] [PubMed] [Google Scholar]
- 184.Matthews M, Bell E. Assessment of risk of violent offending for adults with intellectual disability and/or autism spectrum disorder. In: The Wiley Handbook of what works in violence risk management, 2020: 349–66. [Google Scholar]
- 185.Gerson R, Malas N, Mroczkowski MM. Crisis in the emergency department: the evaluation and management of acute agitation in children and adolescents. Child Adolesc Psychiatr Clin N Am 2018;27:367–86. 10.1016/j.chc.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 186.Fernandes NA, Sawyer A, Zaheer J, et al. Adults with intellectual and developmental disabilities presenting to a psychiatric emergency department: a descriptive analysis and predictors of admission. J Ment Health Res Intellect Disabil 2020;13:384–95. 10.1080/19315864.2020.1822963 [DOI] [Google Scholar]
- 187.Valenti E, Giacco D, Katasakou C, et al. Which values are important for patients during involuntary treatment? A qualitative study with psychiatric inpatients. J Med Ethics 2014;40:832–6. 10.1136/medethics-2011-100370 [DOI] [PubMed] [Google Scholar]
- 188.McGuinness D, Murphy K, Bainbridge E, et al. Individuals' experiences of involuntary admissions and preserving control: qualitative study. BJPsych Open 2018;4:501–9. 10.1192/bjo.2018.59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Hui K, Cooper RB, Zaheer J. Engaging patients and families in the ethics of involuntary psychiatric care. Am J Bioeth 2020;20:82–4. 10.1080/15265161.2020.1754511 [DOI] [PubMed] [Google Scholar]
- 190.Care HKR. closeness, and becoming ‘better’: Transformation and therapeutic process in American adolescent psychiatric custody. Ethos 2016;44:313–32. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjhci-2021-100459supp001.pdf (199.1KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.


