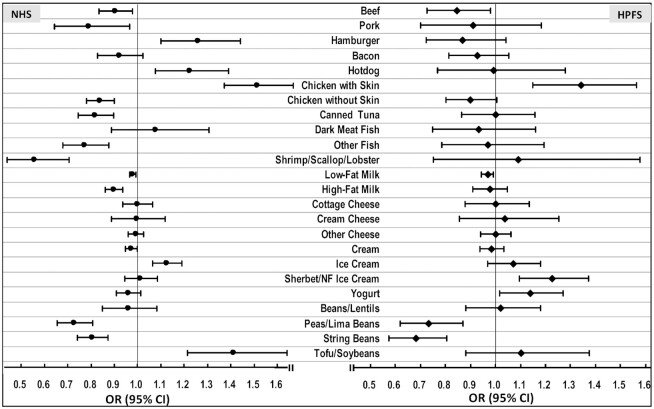
FIGURE 2.
ORs (95% CIs) of a 3-unit increment in subjective cognitive decline (SCD), associated with individual protein food sources in the Nurses’ Health Study (NHS) and Health Professionals Follow-up Study (HPFS). For each 3-serving/wk of protein foods as continuous variables. Multivariate model: NHS: adjusted for age (at SCD assessment, continuous, with a linear and a quadratic term, years), total energy intake (kcal, continuous), census tract income ($50,000, $50,000–$69,999, or $70,000/y), education (registered nursing degrees, bachelor's degree, master's or doctorate degree), husband's education (high school or lower education, college, graduate school), race (white, black, other), smoking history (never, ≤4 pack-years, 5–24 pack-years, ≥25 pack-years), depression, physical activity level (metabolic equivalent–h/wk, quintiles), BMI (<23, 23–25, 25-30, >30 kg/m2) from 1984 to 2006, intakes of alcohol (g/d), postmenopausal status and hormone replacement therapy use, family history of dementia, missing indicator for SCD measurement at 2012 or 2014, number of dietary assessments during 1984–2006, multivitamin use (yes/no), and parity (nulliparous, 1–2, >2). HPFS: adjusted for age, total energy intake, smoking history (never, 1–24 pack-years, 25–44 pack-years, ≥45 pack-years), cancer (yes/no), depression, family history of dementia, physical activity level (metabolic equivalent–h/wk, quintiles), BMI (<23, 23–24.9, 25–29.9, ≥30 kg/m2) from 1986 to 2002, multivitamin use (yes/no), intake of alcohol (g/d), profession (dentist, pharmacist, optometrist, osteopath, podiatrist, veterinarian), missing indicator for SCD measurement at 2008 or 2012, and number of dietary assessments during 1986–2002. Both cohorts also adjusted for dietary intakes of total vegetables, fruit, fruit juice, sugar-sweetened beverages, and sweets/desserts. Poisson regression was used for data analysis.