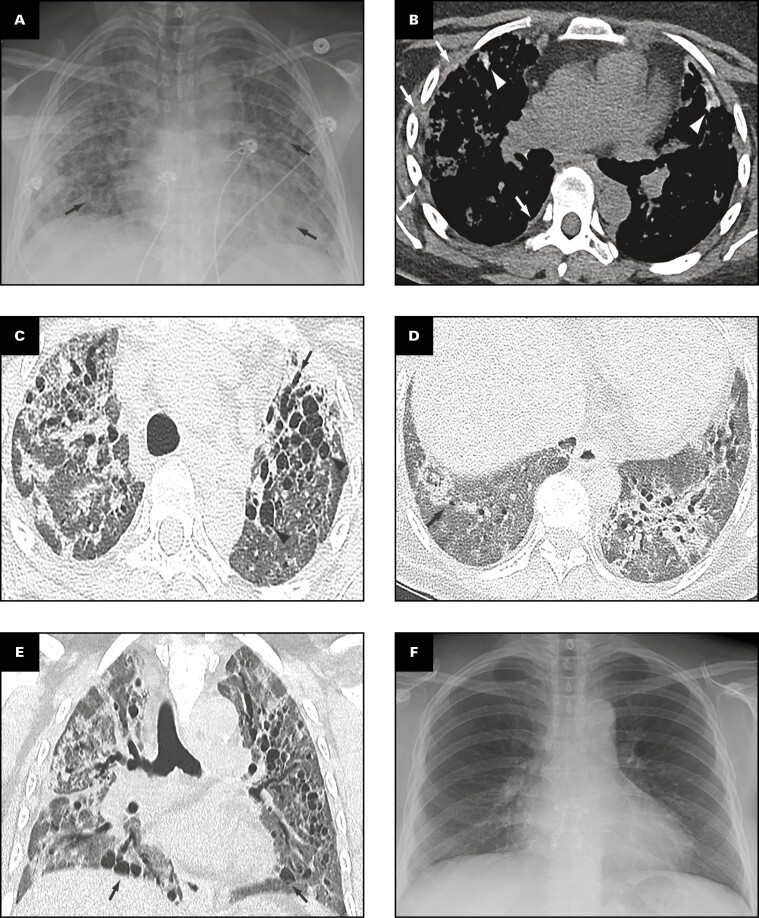
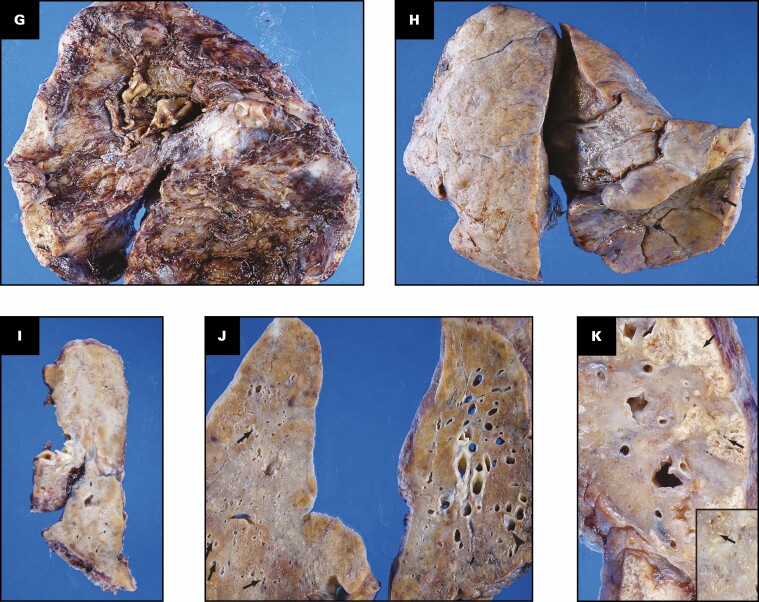
Figure 1.
Patient 1: A 40-year-old woman with coronavirus disease 2019 prior to and after bilateral lung transplant. Overview of radiographic and gross pathologic observations. A, Chest radiograph 2 months prior to transplant shows lucencies representing bilateral bronchiectasis (arrows) and extensive bilateral patchy and hazy parenchymal opacities. B, Chest computed tomography (CT) axial soft tissue window image shows right pleural thickening (arrows) and calcified peripheral triangular densities (arrowheads). C-E, Chest CT lung window images show all areas of lung affected by ground-glass opacity, consolidation, and bronchiectasis. Severe bronchiectasis is present bilaterally, particularly in the upper lobes and anteriorly, such as in the left upper lobe (C, arrow) with cystic areas (C, arrowheads) that represent cystic bronchiectasis and pneumatoceles. D, On a more caudal axial image, consolidation in the left lower lobe and right lower lobe is present with traction bronchiectasis (arrows). E, Coronal image demonstrates cystic areas (arrows) related to pneumatoceles and varicose and cystic bronchiectasis. F, Chest radiograph 4 months after bilateral transplanted lungs with sternal hardware and mediastinal clips. Grossly (G-K), the pleural surface of the right lung has adhesions (G), whereas that of the left lung (H) has few adhesions on the diaphragmatic surface (arrow). The cut surface of the lungs shows consolidation affecting all lobes diffusely (I, right lung; J, K, left lung), with multiple small cysts (arrows, J) and bronchiectasis/bronchiolectasis (arrowhead, J). The calcified peripheral triangular densities seen on the CT scan (arrowheads, B) are seen on the cut surface as denser areas of consolidations (arrows, K), with the inset in K showing tan white streaks of calcification (arrow).