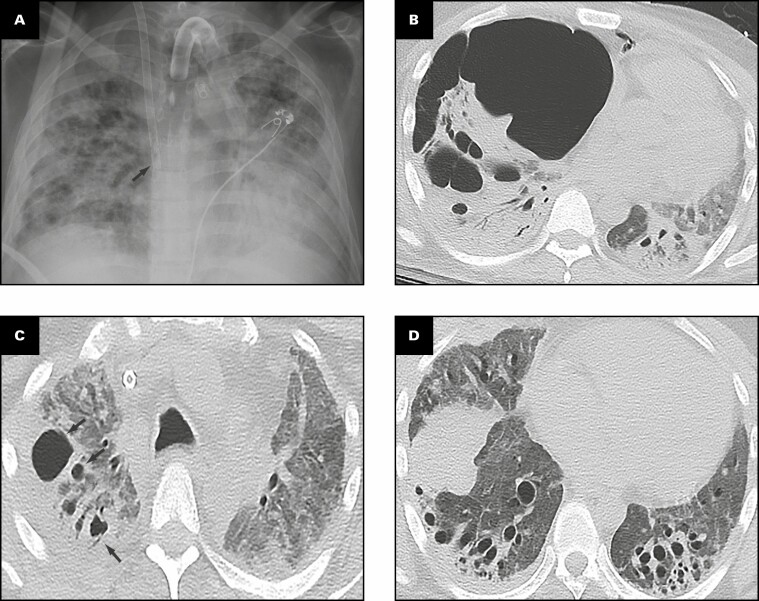
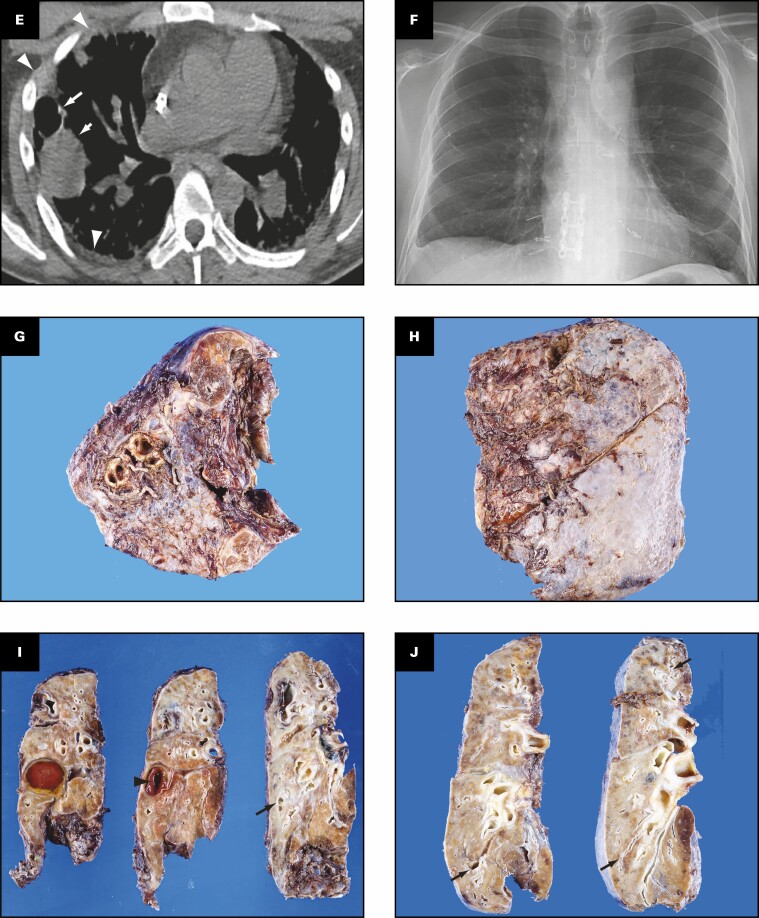
Figure 3.
Patient 2: A 33-year-old man who had a bilateral lung transplant for coronavirus disease 2019. Overview of radiographic and gross pathologic observations. A, Chest radiograph 3 months prior to hospital transfer shows a superior vena cava extracorporeal membrane oxygenation cannula tip overlying the superior cavoatrial junction (arrow), tracheostomy, and severe consolidation. B, On an axial lung window image from chest computed tomography (CT) 19 days later, a large right lower hemithorax air collection represents both pneumothorax and cavity. Multiple pneumatoceles (arrow) are in the right lung within bilateral consolidation and diffuse ground-glass attenuation. C, D, Two and a half months later, chest CT axial lung window images show opacification of the lung by ground-glass opacities and consolidation with right upper lobe cysts (C, arrows). At the lung bases (D), cylindrical bronchiectasis is now severe, consolidation is decreased, and extensive ground-glass opacities persist. E, Axial soft tissue windowed chest CT image shows a cyst (long arrow), fluid-filled cavity in the right middle lobe (short arrow), and right pleural thickening (arrowheads). Some consolidation is evident on the image. F, Chest radiograph 3.5 months after transplant demonstrates bilateral lung transplant changes. Grossly (G-J), the pleural surfaces of the right (G) and left (H) lungs have pleural adhesions. The cut surface of the lungs shows consolidation affecting all lobes diffusely (I, right lung; J, left lung), with bronchiectasis/bronchiolectasis (arrows, I and J). The right middle lobe has a cavity filled with blood (arrowhead, I).